Metagenomic Next-Generation Sequencing for Bacterial Identification: A Comprehensive Guide for Researchers and Drug Developers
Metagenomic next-generation sequencing (mNGS) is revolutionizing bacterial identification by enabling unbiased, culture-independent detection of pathogens directly from clinical samples.
Metagenomic Next-Generation Sequencing for Bacterial Identification: A Comprehensive Guide for Researchers and Drug Developers
Abstract
Metagenomic next-generation sequencing (mNGS) is revolutionizing bacterial identification by enabling unbiased, culture-independent detection of pathogens directly from clinical samples. This article provides a comprehensive overview for researchers and drug development professionals, covering the foundational principles of mNGS technology and its transformative advantages over conventional culture methods. It details the end-to-end workflow from sample preparation to bioinformatic analysis, explores clinical applications across diverse infection types, and addresses key methodological challenges and optimization strategies. The content further evaluates performance through validation studies and comparative analyses with traditional diagnostics, highlighting mNGS's superior sensitivity for detecting fastidious, rare, and polymicrobial infections. Finally, it discusses the translational pathway for integrating mNGS into precision infectious disease management and antimicrobial stewardship programs.
Unlocking the Microbial World: Core Principles and Advantages of mNGS in Bacteriology
Defining Metagenomic Next-Generation Sequencing (mNGS) and its Hypothesis-Free Approach
Metagenomic Next-Generation Sequencing (mNGS) is a high-throughput sequencing technology that enables the comprehensive and unbiased detection of microbial nucleic acids (DNA and/or RNA) directly from clinical, environmental, or other samples without the need for prior culturing [1]. This approach allows for the simultaneous identification and characterization of genomes from bacteria, viruses, fungi, and parasites present in a sample, providing a powerful tool for understanding microbial community composition and diagnosing infections [2] [3]. The core principle of mNGS involves sequencing all nucleic acids in a given sample and then using bioinformatic analysis to assign these sequences to their reference genomes, thereby determining which microbes are present and in what relative proportions [2].
The most significant advantage of mNGS, and the characteristic that distinguishes it from traditional diagnostic methods, is its hypothesis-free nature [2] [4]. Unlike targeted methods such as polymerase chain reaction (PCR) or culture-based techniques that require prior knowledge or suspicion of a specific pathogen to guide testing, mNGS does not rely on pre-formulated hypotheses about the causative agent [2]. This unbiased approach is particularly valuable for detecting rare, novel, or unexpected pathogens, as well as polymicrobial infections, that might be missed by conventional, targeted assays [1].
The Hypothesis-Free Nature of mNGS
Conceptual Foundation of Unbiased Detection
The hypothesis-free approach of mNGS stems from its fundamental design as an untargeted, comprehensive screening tool. Traditional molecular diagnostics, such as PCR, rely on primers designed to amplify specific sequences from pre-identified targets [2]. Even so-called "broad-range" PCR methods that target conserved genetic regions (e.g., bacterial 16S rRNA or fungal ITS sequences) are not truly metagenomic because they still depend on specific primers and cannot simultaneously identify pathogens across different kingdoms of life with equal efficiency [2].
In contrast, mNGS employs a shotgun sequencing approach that randomly fragments all nucleic acids in a sample for sequencing, without targeting any specific organisms [2] [3]. This methodology allows for the detection of virtually all pathogens in a single test, making it particularly useful in diagnostically challenging scenarios where conventional tests have failed or when infections present with atypical symptoms [5] [1]. The capacity to identify novel or unexpected pathogens was notably demonstrated during the emergence of new infectious diseases, where mNGS played a crucial role in pathogen discovery [6].
Contrasting Targeted and Hypothesis-Free Approaches
Table 1: Comparison between targeted molecular methods and hypothesis-free mNGS
| Feature | Targeted Methods (e.g., PCR) | Hypothesis-Free mNGS |
|---|---|---|
| Requirement for Prior Knowledge | Requires suspicion of specific pathogen(s) | No prior knowledge needed |
| Detection Range | Limited to pre-specified targets | Comprehensive across biological kingdoms |
| Novel Pathogen Detection | Generally unable to detect | Capable of identifying novel organisms |
| Polymicrobial Infection Diagnosis | Challenging, may require multiple tests | Can simultaneously detect mixed infections |
| Primary Limitation | Narrow scope | Requires sophisticated bioinformatics |
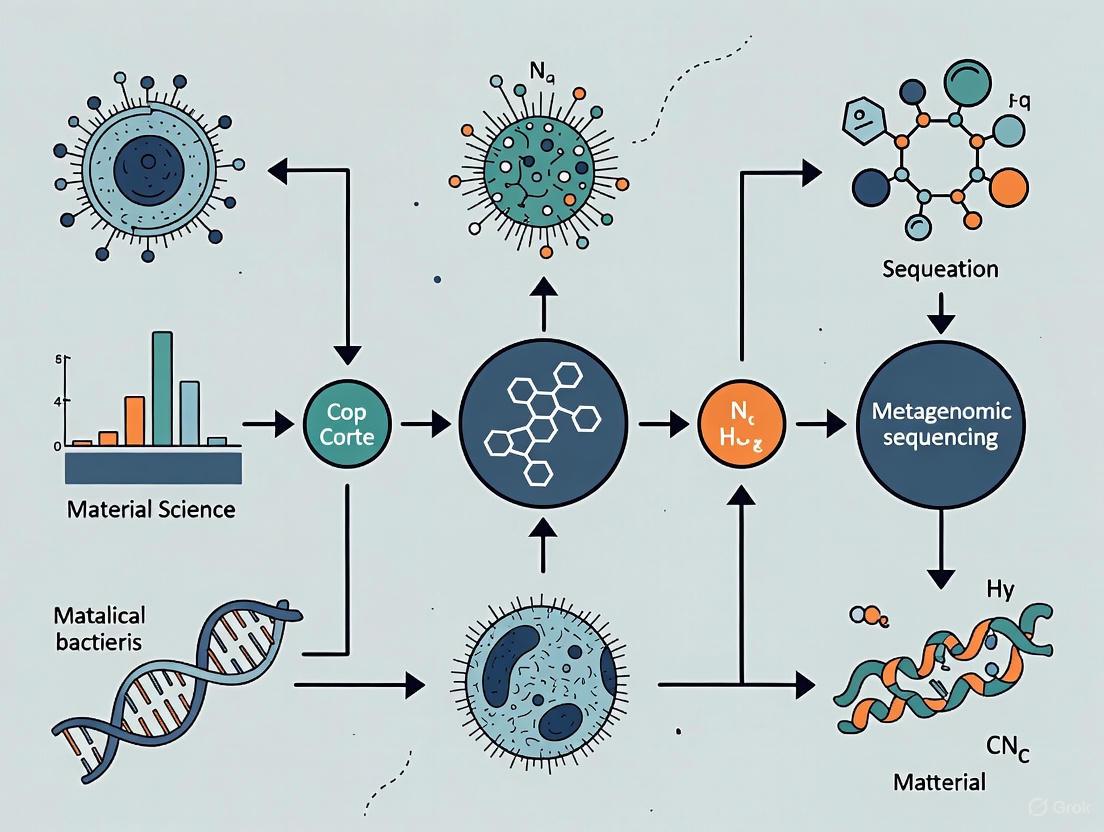
Diagram 1: Hypothesis-free versus targeted diagnostic approaches
Technical Workflow and Methodologies
Comprehensive mNGS Laboratory Workflow
The mNGS process consists of two major components: the wet lab procedures (laboratory testing) and the dry lab procedures (bioinformatic analysis) [1]. The wet lab component includes sample collection, nucleic acid extraction, library construction, and high-throughput sequencing, while the dry lab component encompasses quality control, removal of human sequences, alignment of sequences to microbial databases, and analysis of drug resistance or virulence genes [1].
Sample Collection and Processing: The initial step involves collecting appropriate samples, which for clinical applications may include cerebrospinal fluid (CSF), blood, bronchoalveolar lavage fluid (BALF), sputum, tissue, or other body fluids [1] [3]. Sample selection is critical, as some samples like blood and CSF have less background noise compared to others like stool or nasopharyngeal swabs that contain abundant commensal microorganisms [3]. Proper sample collection with minimal contamination is essential, especially given the analytical sensitivity of mNGS [2].
Nucleic Acid Extraction and Library Preparation: Total nucleic acid (both DNA and RNA) is extracted from the sample, often using commercial kits designed to maintain the representation of different microbial populations [3] [7]. For RNA viruses, RNA is reverse-transcribed into complementary DNA (cDNA). The extracted nucleic acids are then processed for library preparation, which involves fragmenting the DNA/cDNA, attaching adapters, and sometimes amplifying the material to create a sequencing library [1] [3].
Host DNA Depletion: One significant challenge in mNGS, particularly for clinical samples, is that the vast majority of sequenced nucleic acids (often >95%) may originate from the host rather than pathogens [2] [5]. To increase the sensitivity for detecting microbial pathogens, various strategies for host DNA depletion may be employed, such as differential lysis, nuclease treatment, or CRISPR-Cas9-based approaches [3]. These methods aim to reduce host background while preserving pathogen nucleic acids.
Sequencing Platforms: The most commonly used platform for mNGS is Illumina, which utilizes sequencing-by-synthesis technology with high accuracy and relatively low error rates (as low as 0.1%) [1]. Other platforms include Thermo Fisher Ion Torrent (which uses semiconductor sequencing), BGISEQ-500, and Oxford Nanopore Technologies (which enables real-time sequencing) [1]. Each platform has distinct advantages and limitations in terms of cost, throughput, read length, and error profiles.
Bioinformatic Analysis Pipeline
The bioinformatic analysis of mNGS data is a complex, multi-step process that requires specialized expertise and computational resources [2] [3]:
- Quality Control and Trimming: Raw sequencing reads are first processed to remove low-quality sequences, adapter sequences, and duplicate reads [3].
- Host Sequence Subtraction: The remaining reads are aligned to the human reference genome (e.g., hg38) and matching sequences are computationally subtracted to reduce background noise and increase the proportion of microbial reads [3].
- Taxonomic Classification: The non-host reads are then aligned to comprehensive microbial genome databases using various classification tools (e.g., Kraken, BLAST) to identify the species present in the sample [3] [4].
- Pathogen Identification: The classified reads are analyzed to determine which microorganisms are present, often using thresholds based on read counts, genomic coverage, and comparison to negative controls [8].
- Advanced Characterization: Further analysis may include assembly of pathogen genomes, identification of antimicrobial resistance genes, and detection of virulence factors [3].
Diagram 2: mNGS workflow overview
Research Reagent Solutions and Experimental Materials
Successful implementation of mNGS requires careful selection of reagents and materials throughout the workflow. The table below outlines essential components and their functions in a typical mNGS experiment.
Table 2: Key research reagent solutions and materials for mNGS workflows
| Category | Specific Examples | Function/Purpose |
|---|---|---|
| Nucleic Acid Extraction | TIANamp Micro DNA Kit, MagMAX Viral Isolation Kit, RNeasy PowerSoil Total RNA Kit | Isolation of total DNA and/or RNA from samples while maintaining representative abundance |
| Library Preparation | QIAseq Ultralow Input Library Kit | Conversion of extracted nucleic acids into sequencing-ready libraries; particularly important for low-biomass samples |
| Host Depletion | DNase I treatment, rRNA depletion kits, CRISPR-Cas9 based methods | Reduction of host (e.g., human) nucleic acids to enhance detection of low-abundance pathogens |
| Sequencing | Illumina NextSeq 550, MiSeq; Oxford Nanopore MinION | Platforms for high-throughput sequencing with different trade-offs in cost, throughput, and read length |
| Bioinformatics Tools | Kraken2, MetaPhlAn, MEGAHIT, Burrows-Wheeler Alignment, BLAST | Taxonomic classification, sequence alignment, de novo assembly, and database searching |
| Reference Databases | FDA-ARGOS, NCBI RefSeq, CARD (antibiotic resistance), VFDB (virulence factors) | Curated genomic databases for accurate taxonomic assignment and functional characterization |
Applications, Challenges, and Future Directions
Key Applications in Infectious Disease Research
The hypothesis-free nature of mNGS makes it particularly valuable in various clinical and research scenarios:
- Diagnosis of Neurological Infections: mNGS of cerebrospinal fluid has proven effective in identifying causes of meningitis and encephalitis, especially when conventional testing is negative or unavailable [2] [6].
- Respiratory Infections: Bronchoalveolar lavage fluid and sputum analyzed by mNGS can detect complex communities of bacteria, viruses, and fungi in patients with pneumonia, particularly in immunocompromised individuals where mixed infections are common [8].
- Detection of Uncultivable or Fastidious Pathogens: mNGS can identify microorganisms that cannot be cultured using standard methods, including some bacteria, viruses, and fungi [1].
- Antimicrobial Resistance Characterization: mNGS can detect resistance genes directly from clinical samples, providing insights into the resistome of infectious agents [5] [3].
- Outbreak Investigation: The ability to generate whole or partial genomes enables tracking of transmission pathways and infection control surveillance [2].
Current Challenges and Limitations
Despite its powerful capabilities, mNGS faces several significant challenges that limit its widespread clinical adoption:
- Distinguishing Pathogens from Contaminants: One of the most difficult aspects of mNGS interpretation is differentiating true pathogens from environmental contaminants or colonizing organisms [2]. This requires careful analysis and correlation with clinical findings.
- High Cost and Resource Requirements: mNGS remains expensive compared to conventional diagnostics and requires specialized equipment, reagents, and bioinformatics expertise [2] [1].
- Bioinformatic Complexity: The analysis of mNGS data demands substantial computational resources and specialized expertise that may not be available in routine clinical laboratories [2] [3].
- Regulatory Hurdles: As of the time of writing, there are no FDA-cleared or approved mNGS tests specifically for microbial identification, although CLIA-certified laboratories may offer such testing [2].
- Database Limitations: The accuracy of mNGS is highly dependent on the completeness and quality of reference databases, which may have gaps for rare or novel organisms [2].
Emerging Innovations and Future Directions
The field of mNGS continues to evolve rapidly with several promising developments:
- Targeted Metagenomics (tNGS): This approach uses multiplex PCR with primers targeting common pathogens before sequencing, increasing sensitivity for specific targets while reducing cost [8]. One study reported a higher coincidence rate with clinical diagnoses for tNGS (81.4%) compared to untargeted mNGS (40.0%) for respiratory infections [8].
- AI-Assisted Bioinformatics: Artificial intelligence and machine learning approaches are being integrated into mNGS analysis to improve sensitivity, specificity, and interpretation [4]. These systems can help distinguish pathogens from contaminants and identify novel organisms.
- Portable Sequencing Technologies: Platforms such as Oxford Nanopore's MinION enable real-time, field-deployable sequencing that can reduce turnaround times [5] [3].
- Genome-Resolved Metagenomics: Advanced computational methods now allow reconstruction of metagenome-assembled genomes (MAGs) directly from sequencing data, enabling more detailed characterization of microbial communities [9].
- Standardization Efforts: Professional organizations are developing guidelines and recommendations for implementing mNGS in clinical laboratories to improve reproducibility and reliability [7].
Metagenomic Next-Generation Sequencing represents a transformative approach in microbial identification and infectious disease diagnosis through its hypothesis-free, comprehensive analysis of nucleic acids in clinical and environmental samples. Unlike targeted methods that require prior knowledge of suspected pathogens, mNGS simultaneously detects bacteria, viruses, fungi, and parasites across all kingdoms of life without bias. While challenges remain in interpretation, cost, and standardization, ongoing innovations in wet lab methodologies, bioinformatics, and artificial intelligence are steadily addressing these limitations. As the technology continues to evolve and become more accessible, mNGS is poised to play an increasingly central role in clinical microbiology, outbreak investigation, and microbial research, ultimately enhancing our ability to diagnose and understand complex infectious diseases.
Metagenomic next-generation sequencing (mNGS) has emerged as a transformative, hypothesis-free tool in clinical microbiology and infectious disease diagnostics, enabling the simultaneous detection of a broad spectrum of pathogens—including bacteria, viruses, fungi, and parasites—directly from clinical specimens [10]. Unlike traditional culture-based methods and targeted molecular assays that require prior knowledge of the suspected pathogen, mNGS sequences all nucleic acids present in a sample, allowing for the identification of novel, fastidious, and polymicrobial infections [10] [11]. This capability is particularly valuable for diagnosing complex cases in immunocompromised patients, sepsis, and culture-negative infections where conventional methods often fail [10] [12]. The core principle of mNGS involves the comprehensive sequencing of all microbial DNA and/or RNA in a sample, followed by sophisticated bioinformatic analysis to map the sequences to their respective genomes [13].
The application of mNGS extends beyond human medicine into agricultural sciences, where it is employed for detecting fungal plant pathogens and ensuring crop health, demonstrating its versatility across fields [11]. Despite its powerful capabilities, mNGS is best viewed as a complementary tool rather than a replacement for traditional diagnostics, enhancing diagnostic accuracy when integrated with culture, PCR, and serological assays [10]. This in-depth technical guide details the core mNGS workflow, from sample collection to sequencing and data analysis, providing researchers and drug development professionals with a comprehensive framework for implementing this technology in bacterial identification research.
Wet Lab Workflow: From Sample to Library
Sample Collection and Nucleic Acid Extraction
The first critical step in the mNGS workflow is the collection of appropriate samples and the subsequent extraction of nucleic acids. Suitable specimens vary widely depending on the application and can include bronchoalveolar lavage fluid (BALF), blood, cerebrospinal fluid (CSF), tissue samples, and pleural effusion [10] [14] [12]. For latent pathogen detection in plants, samples should be taken from highly infected, living plants where infection symptoms are most evident [11]. Proper handling is paramount; samples should be transported cold (at 4°C) and stabilized promptly to prevent contamination and DNA degradation, which could compromise the sensitivity of the metagenomic analysis [11].
Nucleic acid extraction can be performed using commercial kits or standard manual procedures, though kits are recommended to minimize the risk of environmental contamination [11]. The extracted nucleic acids constitute a mixture of DNA from multiple species, referred to as mix-DNA, or as environmental DNA (eDNA) when collected from environmental samples [11]. A major challenge in this step, particularly from clinical samples, is the high abundance of host-derived nucleic acids, which can obscure microbial signals. To improve the detection of microbial content, especially in low-biomass specimens, host DNA depletion methods are often employed [10] [15]. For example, a protocol optimized for respiratory samples may use a combination of Sputasol, saponin, and DNase treatment to reduce host background [15].
Table 1: Common Sample Types and Processing Considerations for mNGS
| Sample Type | Recommended Volume | Key Processing Considerations | Common Applications |
|---|---|---|---|
| Bronchoalveolar Lavage Fluid (BALF) | ≥ 5 mL [14] | Host depletion critical; high human DNA content | Lower respiratory tract infections, pneumonia [14] [12] |
| Blood | ≥ 250 µl [15] | Lower microbial biomass; requires sensitive detection | Sepsis, systemic infections [10] |
| Cerebrospinal Fluid (CSF) | Variable | >99% of reads may be host-derived; sterile fluid | Meningitis, encephalitis [10] [16] |
| Tissue | Variable | Homogenization required; potential for high host DNA | Localized infections, pathogen discovery [12] |
| Sputum/Endotracheal Aspirates | ≥ 250 µl [15] | Requires digestion (e.g., with Sputasol) | Pulmonary infections [15] |
Library Preparation
Library preparation is the process that makes the extracted nucleic acid mixture compatible with sequencing platforms while preserving the diversity of DNA sequences present [11]. The specific methods can differ based on the sequencing technology and the target pathogens.
For bacterial and fungal detection from DNA extracts, the process often involves tagmentation (fragmentation and adapter ligation) using kits like the Rapid PCR Barcoding Kit (SQK-RPB114.24) [15]. This is typically followed by PCR amplification to incorporate full adapters and sample-specific barcodes, enabling the multiplexing of multiple samples in a single sequencing run [15].
For projects aiming to detect viruses or RNA pathogens, an initial reverse transcription (RT) step is necessary to convert RNA into complementary DNA (cDNA). One optimized method uses a "shotgun approach" with 9N random primers for reverse transcription, followed by PCR amplification to generate sequencing-ready libraries from both DNA and RNA pathogens [15].
The entire library preparation process, from tagmentation/RT to a ready-to-sequence library, can be completed in approximately 5-6 hours for a batch of 24 samples using streamlined protocols [15]. Automation is becoming a key driver of clinical NGS adoption, with integrated systems that combine nucleic acid extraction, library preparation, and sequencing into streamlined workflows capable of delivering same-day results [10].
Sequencing Platforms and Data Generation
Following library preparation, the next step is high-throughput sequencing. Several platforms are available, each with distinct characteristics suitable for different research needs.
Short-read sequencing technologies, such as those offered by Illumina (e.g., NextSeq 500, NovaSeq 6000), are widely used in mNGS due to their high accuracy and throughput [16] [14]. These systems generate massive amounts of data, with output ranging from 1.3 billion to 20 billion reads per run, and read lengths typically up to 300 base pairs [16]. This makes them ideal for detecting a wide array of pathogens with high sensitivity.
Long-read sequencing platforms, notably from Oxford Nanopore Technologies (ONT; e.g., MinION, GridION) and Pacific Biosciences (PacBio), offer the advantage of generating much longer reads—spanning thousands of bases [10]. The portability of devices like the MinION is particularly beneficial for point-of-care diagnostics and real-time surveillance in field settings or resource-limited environments [10] [15]. Long reads facilitate the resolution of complex genomic regions, detection of structural variants, and complete reconstruction of plasmids and viral genomes [10].
Table 2: Comparison of Key Next-Generation Sequencing Platforms
| Sequencing Platform | Maximum Read Length | Maximum Data Output per Run | Key Advantages |
|---|---|---|---|
| Illumina iSeq 100 | 2 x 150 bp [16] | 1.2 Gb / 4 million reads [16] | Low-cost, compact system |
| Illumina MiSeq | 2 x 300 bp [16] | 15 Gb / 25 million reads [16] | Mid-range output, versatile |
| Illumina NovaSeq 6000 S4 | 2 x 150 bp [16] | 3000 Gb / 20 billion reads [16] | Ultra-high throughput for large studies |
| Oxford Nanopore MinION/GridION | Thousands of bases (long-read) [10] | Dependent on flow cell and run time | Real-time, portable sequencing; long reads [10] [15] |
The following diagram illustrates the complete mNGS workflow, integrating both short-read and long-read paths from sample to diagnosis:
Bioinformatics Analysis and Quality Control
Primary Data Processing and Quality Control
Once sequencing is complete, the generated raw data must undergo rigorous bioinformatic analysis. The initial step is quality control (QC) to assess the quality of the sequencing data. This involves evaluating several key metrics [16]:
- Input Reads: Checking the total number of reads helps identify samples with insufficient data.
- Reads Passing QC: A high percentage of reads passing QC filtering indicates good quality data. The CZ ID pipeline, for example, removes reads with >15 uncalled bases (N's) and bases with Phred quality scores <17 (corresponding to >98% base call accuracy) [16].
- Insert Length: The length of the nucleotide sequence between adapters should be as expected; shorter lengths may indicate sample degradation.
- Host/Human Reads: The percentage of reads removed as host sequences varies by sample type (e.g., >99% in sterile CSF, lower in stool) [16].
- Read Duplication Levels: High duplication, measured by the Duplicate Compression Ratio (DCR), can indicate low library diversity or PCR amplification bias [16].
Table 3: Key Quality Control Metrics in mNGS Data Analysis
| QC Metric | Interpretation | Tool/Method Example |
|---|---|---|
| Phred Quality Score | Base call accuracy; Q20 = 99% accuracy, Q30 = 99.9% accuracy [16] | FastQC, CZ ID pipeline |
| Host Read Percentage | Varies by sample type; high in sterile sites (CSF), low in high-microbial biomass (stool) [16] | Alignment to host genome (e.g., hg19) [14] |
| Duplicate Compression Ratio (DCR) | Ratio of total to unique sequences; high DCR indicates over-amplification or low complexity [16] | CZ ID pipeline |
| Spike-in Control Recovery (e.g., ERCC) | Assesses sequencing depth and potential bias; under-recovery suggests need for more sequencing [16] | Alignment to control sequences |
Microbial Identification and Contamination Management
After QC, non-host reads are aligned to comprehensive microbial databases for taxonomic classification. Commonly used tools include Kraken2 for rapid classification and Bowtie2/BLAST for validation [14]. A critical aspect of mNGS analysis is distinguishing true pathogens from background contamination introduced during sampling or laboratory processing.
The recommended strategy is to include negative control samples in every run. These controls are used to create a background model, which enables the calculation of a Z-score for each detected taxon in a clinical sample. The Z-score is computed as follows, where "rPM" is reads per million [16]:
Z = (rPM in sample - Mean rPM in negative controls) / Standard Deviation of rPM in negative controls
Taxa present at higher abundance in the sample than in the negative controls will have a Z-score > 1. If a taxon is absent from the negative controls, the Z-score is set to 100 [16]. This Z-score is then used to calculate an aggregate score, an empirical heuristic that ranks microbial matches by combining relative abundance and Z-score information at both the species and genus levels, helping to prioritize likely pathogens over contaminants [16].
The final interpretation must be done in the context of clinical data, as the mere presence of microbial DNA does not automatically establish pathogenicity. For plant pathogens, Koch's postulates may be followed, requiring the identification of pathogen nucleic acid in host tissues and mutation of virulence genes to confirm causality [11].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the mNGS workflow relies on a suite of specialized reagents and equipment. The following table details key solutions and their functions in the context of a typical mNGS experiment.
Table 4: Essential Research Reagent Solutions for mNGS Workflows
| Item Name | Function/Application | Example Products/Formats |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolates total DNA/RNA from complex samples; critical for yield and purity | MagMAX Viral/Pathogen Nucleic Acid Isolation Kit [15] |
| Host Depletion Reagents | Reduces host nucleic acids to improve microbial signal | Saponin solution, HL-SAN Triton Free DNase [15] |
| Library Preparation Kit | Fragments DNA, adds adapters, and incorporates barcodes for multiplexing | Rapid PCR Barcoding Kit (SQK-RPB114.24) [15] |
| Reverse Transcription Kit | Converts RNA to cDNA for detection of RNA viruses | Maxima H Minus Reverse Transcriptase, RLB RT 9N primer [15] |
| PCR Master Mix | Amplifies library fragments for sequencing | LongAmp Hot Start Taq 2X Master Mix [15] |
| Magnetic Beads | Purifies and size-selects nucleic acids during library prep | Agencourt AMPure XP beads [15] |
| DNA Quantification Kit | Precisely measures library concentration before sequencing | Qubit dsDNA HS Assay Kit [15] |
| Sequencing Flow Cell | The surface where sequencing chemistry occurs | R10.4.1 flow cells (FLO-MIN114) for Nanopore [15] |
| Bioinformatics Tools | For quality control, taxonomic classification, and contamination assessment | Kraken2, Bowtie2, BLAST, CZ ID [16] [14] |
The mNGS workflow represents a powerful, comprehensive approach for pathogen detection and discovery. From meticulous sample collection and nucleic acid extraction through sophisticated library preparation, high-throughput sequencing, and rigorous bioinformatic analysis, each step is critical for generating reliable, clinically actionable data. As sequencing technologies continue to advance, becoming faster, more portable, and more cost-effective, and as bioinformatic tools become more standardized and accessible, the implementation of mNGS is poised to expand further. This will enhance our ability to diagnose complex infections, conduct real-time outbreak surveillance, and ultimately advance both clinical medicine and agricultural science through precise microbial identification. For researchers and drug development professionals, mastering this end-to-end workflow is essential for harnessing the full potential of metagenomic sequencing in the fight against infectious diseases.
For over a century, microbiological understanding of bacteria was constrained by a fundamental limitation: the necessity to culture organisms in artificial laboratory media. This culture-based paradigm created what is often termed the "great plate count anomaly"—the consistent observation that microscopic microbial counts exceed culturable counts by several orders of magnitude [17]. This discrepancy is particularly dramatic in aquatic environments, where plate counts and viable cells estimated by staining can differ by four to six orders of magnitude, and in soil, where only 0.1% to 1% of bacteria are readily culturable on common media [17]. The development of metagenomics, defined as the genomic analysis of microorganisms by direct extraction and cloning of DNA from an assemblage of microorganisms, has fundamentally addressed this limitation by enabling researchers to study microorganisms without the requirement for cultivation [17]. This approach provides a second tier of technical innovation that facilitates study of the physiology and ecology of environmental microorganisms, representing a transformative shift in microbiological investigation [17]. This technical guide examines the core advantages of metagenomic sequencing over traditional culture methods, with specific focus on its application in detecting unculturable, fastidious, and novel bacterial species.
Key Advantages of Metagenomic Sequencing Over Culture Methods
Comprehensive Access to Microbial Diversity
Metagenomic sequencing enables researchers to comprehensively sample all genes in all organisms present in a given complex sample, providing unprecedented access to microbial diversity [18]. This approach allows microbiologists to evaluate bacterial diversity and detect the abundance of microbes in various environments while simultaneously studying unculturable microorganisms that are otherwise difficult or impossible to analyze [18]. The application of 16S rRNA gene sequence analysis amplified directly from environmental samples first revealed that as-yet-uncultured microorganisms represent the vast majority of organisms in most environments on Earth, leading to the discovery of vast new lineages of microbial life [17]. While 16S studies revolutionized our understanding of microbial community membership, they provided limited insight into the genetics, physiology, and biochemistry of the members—a limitation addressed by the more comprehensive approach of shotgun metagenomic sequencing [17].
Detection of Unculturable and Fastidious Organisms
A significant advantage of metagenomic sequencing is its capacity to identify pathogens in patients with prior antibiotic exposure, where traditional culture methods often fail [19]. Both fastidious organisms (those with specific nutritional requirements that cannot be met in standard culture) and viable but non-culturable (VBNC) organisms (those that are metabolically active but cannot proliferate in culture conditions) can be detected through metagenomic approaches. This capability is particularly valuable in clinical settings where antibiotic treatment often precedes diagnostic testing. Research has demonstrated that the positive rates of metagenomic testing of puncture fluid and tissue samples were significantly higher than those of culture in patients who had prior antibiotic use, with this difference being statistically significant (p = 0.000) [19]. This independence from prior antibiotic exposure represents a crucial diagnostic advantage over culture-based methods.
Discovery of Novel and Unexpected Pathogens
Metagenomic next-generation sequencing (mNGS) operates as a hypothesis-free detection method, enabling identification of novel, rare, and unexpected pathogens that would not be targeted by specific PCR assays or culture conditions [20] [10]. This unbiased approach has proven particularly valuable for detecting emerging pathogens and co-infections that conventional methods might miss. Clinical studies have demonstrated that mNGS provides more comprehensive information about pathogens compared to conventional diagnostic methods, with the capability to identify novel, rare, and unexpected pathogens that were previously undetectable [20]. This discovery potential extends beyond clinical medicine to environmental and industrial applications, where metagenomics has been used to identify novel enzymes and metabolic pathways from uncultured microbial communities [21].
Rapid Turnaround Time and Diagnostic Efficiency
In clinical contexts, metagenomic sequencing offers significantly faster pathogen identification compared to traditional culture methods, particularly for slow-growing organisms. While conventional culture typically requires 1-5 days (and longer for slow-growing microorganisms like fungi and mycobacteria), metagenomic workflows can generate results within hours [19]. Advanced workflows have demonstrated the capability to produce first automated reports after just 30 minutes of sequencing from a 7-hour end-to-end workflow, with sensitivity and specificity for bacterial detection reaching 90% and 100%, respectively, after just 2 hours of sequencing [22]. This rapid turnaround enables more timely targeted treatment, which is particularly crucial for critically ill patients and those with infections caused by fastidious or slow-growing organisms.
Table 1: Comparison of Diagnostic Performance Between Metagenomic Sequencing and Culture Methods
| Parameter | Metagenomic Sequencing | Conventional Culture |
|---|---|---|
| Sensitivity | 58.01% (for all pathogens) [19] | 21.65% (for all pathogens) [19] |
| Specificity | 85.40% [19] | 99.27% [19] |
| Time to Result | 7-24 hours [22] [19] | 1-5 days (longer for slow-growing organisms) [19] |
| Effect of Prior Antibiotics | Minimal impact [19] | Significant reduction in yield [19] |
| Novel Pathogen Detection | Capable [20] [10] | Not capable |
| Polymerase Chain Reaction (PCR) | 92% sensitivity, 100% specificity for viruses after 2h sequencing [22] | Not applicable for virus detection |
Table 2: Applications of Metagenomic Sequencing Across Sample Types
| Sample Type | Key Applications | Considerations |
|---|---|---|
| Bronchoalveolar Lavage Fluid (BALF) | Diagnosis of pulmonary infections; simultaneous pathogen detection and malignancy screening via copy number variation analysis [14] | Higher human DNA background requires effective depletion methods [22] |
| Cerebrospinal Fluid (CSF) | Diagnosis of central nervous system infections; demonstrated diagnostic yield up to 63% vs <30% for conventional approaches [10] | Low microbial biomass requires high sensitivity methods |
| Blood | Detection of bloodstream infections and sepsis pathogens [19] | Effective host DNA depletion critical for sensitivity |
| Tissue | Identification of pathogens in deep-seated infections [19] | Requires homogenization; less affected by antibiotics than culture |
| Environmental Samples | Exploration of novel enzymes from uncultured microbes [21]; environmental surveillance [23] | Extreme microbial diversity requires sufficient sequencing depth |
Experimental Protocols and Methodologies
Sample Processing and Host DNA Depletion
Effective host DNA depletion is crucial for enhancing sensitivity in metagenomic sequencing, particularly in samples with high human DNA background. A mechanical host-depletion method has been developed that allows simultaneous detection of RNA and DNA microorganisms. This protocol involves:
- Sample Preparation: Centrifuge samples at 1200g for 10 minutes to pellet human cells [22].
- Bead-Beating Lysis: Transfer 500 µL of supernatant to bead-beating tubes containing 1.4 mm zirconium-silicate spheres and process for 3 minutes at 50 oscillations/second in a tissue lyser to mechanically lyse human cells [22].
- Enzymatic Digestion: Transfer 200 µL to a clean tube with 10 µl of HL-SAN nuclease (without buffer) and incubate at 37°C for 10 minutes at 1000 rpm to digest released human nucleic acids [22].
- Nucleic Acid Extraction: Extract DNA and RNA from preserved intact microorganisms using automated systems with 200 μL input volume and 50 μl elution volume [22].
This method has been shown to decrease human DNA concentration by a median of eight Ct values while preserving a broad range of microorganisms including bacteria, fungi, and both DNA and RNA viruses [22].
Library Preparation and Sequencing
The converted double-stranded DNA undergoes library preparation followed by sequencing:
- Library Preparation: DNA is prepared using a Rapid PCR barcoding kit with increased PCR cycles (30 cycles) to amplify microbial DNA [22].
- Sequencing: Samples are sequenced on platforms such as the GridION (Oxford Nanopore Technologies) or Illumina NextSeq500, multiplexing 3-10 samples per flowcell [22] [14].
- Base Calling and Demultiplexing: Raw reads are demultiplexed and base-called using software like Guppy within MinKNOW, filtering reads with q-score <7 and length below minimum thresholds [22].
For Illumina-based approaches, libraries are typically sequenced to generate 10-20 million reads per sample to ensure sufficient coverage for pathogen detection [14].
Bioinformatic Analysis for Pathogen Detection
Bioinformatic processing is essential for accurate pathogen identification:
- Host Sequence Removal: The SNAP software is used to eliminate human sequences based on the human reference database (hg38) [19].
- Taxonomic Classification: Non-human reads are aligned to manually curated microbial databases using classifiers such as Kraken2 (confidence = 0.5) for rapid classification [14].
- Validation: Classified reads of interested microorganisms are realigned using Bowtie2 for validation, with inconsistent classifications further validated by BLAST alignment to nucleotide databases [14].
- Clinical Interpretation: Potential pathogens are selected based on clinical phenotype and reviewed by clinicians to determine clinical relevance, with species typically categorized as definite, probable, possible, or unlikely pathogens based on clinical, radiologic, or laboratory findings [14].
Workflow Visualization: From Sample to Pathogen Identification
Metagenomic Sequencing and Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for Metagenomic Sequencing Workflows
| Reagent/Equipment | Function | Examples/Specifications |
|---|---|---|
| Zirconium-Silicate Beads | Mechanical lysis of human cells while preserving intact microorganisms | 1.4 mm spheres for effective cell disruption [22] |
| HL-SAN Nuclease | Digestion of released human nucleic acids without buffer requirement | Digests DNA at roughly 10-fold higher efficiency than RNA [22] |
| Nucleic Acid Extraction Kits | Simultaneous extraction of DNA and RNA from bacteria, viruses, and fungi | MagNA Pure 24 System with total NA isolation kit [22] |
| Reverse Transcription Mix | Conversion of RNA to cDNA for inclusion in sequencing | LunaScript RT SuperMix Kit for cDNA synthesis [22] |
| Double-Strand DNA Synthesis Kit | Conversion of single-stranded DNA to double-stranded form for sequencing | Sequenase version 2.0 for dsDNA synthesis [22] |
| PCR Barcoding Kit | Library preparation with sample multiplexing capability | Rapid PCR barcoding kit with increased cycle number (30 cycles) [22] |
| Sequencing Platforms | High-throughput DNA sequencing | GridION (Oxford Nanopore), Illumina NextSeq500 [22] [14] |
| Bioinformatic Tools | Taxonomic classification and pathogen identification | Kraken2, Bowtie2, BLAST for validation [14] |
Metagenomic sequencing represents a paradigm shift in microbial detection and characterization, offering significant advantages over traditional culture methods. Its capacity to identify unculturable, fastidious, and novel bacteria; its reduced susceptibility to prior antibiotic exposure; and its rapid turnaround time make it an indispensable tool for both clinical diagnostics and environmental microbiology. As sequencing technologies continue to advance and become more accessible, metagenomic approaches are poised to become standard practice for comprehensive microbial analysis, enabling researchers to explore the vast diversity of the microbial world that has remained largely inaccessible through culture-based methods alone. The integration of metagenomics with other omics technologies and the development of standardized protocols will further enhance our ability to detect and characterize previously elusive microorganisms, opening new frontiers in microbial ecology, infectious disease management, and bioprospecting.
The diagnostic landscape for infectious diseases is undergoing a revolutionary transformation driven by metagenomic next-generation sequencing (mNGS). This technological advancement represents a fundamental shift from hypothesis-dependent methods to comprehensive, unbiased pathogen detection, directly addressing critical limitations of conventional microbiological diagnostics. Traditional culture-based techniques and targeted molecular assays, while foundational, suffer from prolonged turnaround times, limited pathogen spectrum, and inherent difficulties in detecting polymicrobial infections [10] [24]. These limitations are particularly consequential in critically ill patients, where diagnostic delays lead to empiric broad-spectrum antibiotic use, escalating healthcare costs, and contributing to suboptimal outcomes, including mortality risks that increase significantly with each hour of delayed appropriate treatment [10] [24].
Metagenomic NGS enables the simultaneous, hypothesis-free detection of a vast array of pathogens—including bacteria, viruses, fungi, and parasites—directly from clinical specimens [10]. By sequencing all nucleic acids present in a sample, mNGS transcends the culturing capabilities of fastidious, slow-growing, or non-culturable organisms and provides a powerful solution for analyzing complex polymicrobial infections [25]. This in-depth technical guide examines the core mechanisms through which mNGS overcomes traditional diagnostic barriers, with a specific focus on speed, expansive pathogen coverage, and sophisticated polymicrobial infection analysis, providing researchers and drug development professionals with a comprehensive framework for its application in clinical and research settings.
The Technical Superiority of mNGS Over Conventional Diagnostics
Quantitative Performance Comparison
The advantages of mNGS over traditional diagnostic methods are substantial and consistently demonstrated across clinical studies. The table below summarizes a direct performance comparison from recent clinical investigations.
Table 1: Comparative Diagnostic Performance of mNGS vs. Traditional Culture Methods
| Diagnostic Parameter | mNGS Performance | Traditional Culture Performance | Clinical Context (Study) |
|---|---|---|---|
| Sensitivity | 82.3% [26] - 95.35% [27] | 17.5% [26] - 81.08% [27] | Spinal infections [26], Lower respiratory tract infections (LRTI) [27] |
| Detection Rate | 77.6% [26] | 18.4% [26] | Spinal infections |
| Average Turnaround Time | 1.65 days [26] | 3.07 days [26] | Spinal infections |
| Polymicrobial Infection Detection | Capable of comprehensive profiling [10] [25] | Misses an estimated 30-40% of co-pathogens [25] | Diabetic foot infections, intra-abdominal infections [25] |
| Pathogen Coverage | Identified 36.36% of bacteria and 74.07% of fungi detected by cultures, plus additional pathogens [27] | Limited to cultivable organisms under specific conditions | LRTI in COVID-19 patients [27] |
Core Technical Workflow of Metagenomic Sequencing
The robust performance of mNGS stems from its culture-independent, comprehensive workflow. The entire process, from sample to report, integrates sophisticated wet-lab and computational steps to achieve unbiased pathogen detection.
Diagram 1: The End-to-End mNGS Workflow for Pathogen Detection. This comprehensive pipeline transforms a clinical sample into a actionable diagnostic report through integrated laboratory and computational processes.
Overcoming the Speed Barrier: Rapid Molecular Identification
Significant Reduction in Time-to-Result
The rapid turnaround time of mNGS is a critical advantage in acute clinical settings. A comparative study on spinal infections demonstrated that the average diagnosis time for mNGS was 1.65 days, significantly shorter (p < 0.001) than the 3.07 days required for standard bacterial culture [26]. This ~1.5-day reduction in time-to-result can dramatically alter patient management, enabling clinicians to transition from broad-spectrum empiric therapy to targeted antimicrobial treatment much earlier in the clinical course [10] [26].
This acceleration is largely attributable to the elimination of the prolonged incubation periods required for microbial growth in culture. The mNGS process, from sample processing to sequencing, can be completed within 24-48 hours, with emerging portable sequencing technologies like Oxford Nanopore Technologies (ONT) platforms pushing this further toward real-time, point-of-care diagnostics [10]. These platforms have been deployed in field settings for rapid diagnosis during outbreaks of Ebola, Zika, and SARS-CoV-2, underscoring their utility in decentralized and time-sensitive healthcare delivery [10].
Detailed Protocol for Rapid mNGS
Protocol: Rapid mNGS from Sample to Data (Adapted from Clinical Studies) [10] [26]
Sample Collection & Processing (2-4 hours):
- Collect appropriate clinical specimen (e.g., cerebrospinal fluid, blood, bronchoalveolar lavage fluid, tissue). For sputum, assess quality using the Bartlett grading system (score ≤1) to minimize oropharyngeal contamination [27].
- Host DNA Depletion (Critical Step): Treat samples with commercial kits (e.g., benzonase) or differential lysis to reduce human background, significantly improving microbial signal, especially in low-biomass specimens [10].
- Nucleic Acid Co-Extraction: Extract total DNA and RNA simultaneously using validated kits (e.g., TIANamp Magnetic DNA Kit). For RNA viruses, include a reverse transcription step to generate cDNA [26].
Library Preparation & Sequencing (6-12 hours):
- Library Construction: Fragment nucleic acids and ligate with sequencing adapters using high-throughput preparation kits (e.g., KAPA HyperPrep Kit). This step can include indexing to multiplex multiple samples in a single run [26].
- Sequencing: Load libraries onto a next-generation sequencer (e.g., Illumina, Ion PGM System, or MinION). For the Dif seq platform, a target depth of 20 million reads is often used for the metagenomic workflow to ensure sufficient coverage [26].
Bioinformatic Analysis (2-6 hours):
- Quality Control & Host Removal: Remove low-quality reads, adapter contamination, and sequences aligning to the human reference genome (e.g., hs37d5) using tools like Bowtie2 [26].
- Pathogen Identification: Align non-human reads to comprehensive microbial genome databases (bacteria, fungi, viruses, parasites) using specialized classifiers [26].
Achieving Unprecedented Breadth in Pathogen Coverage
Hypothesis-Free Detection of Diverse Pathogens
The "unbiased" nature of mNGS is its most transformative feature, allowing for the detection of nearly any pathogen from a single sample without prior suspicion. This broad coverage is effective against a wide spectrum of infectious agents, including bacteria (cultivable and fastidious), viruses, fungi, and parasites [10]. In lower respiratory tract infections (LRTI), particularly in COVID-19 patients, mNGS demonstrated a superior sensitivity of 95.35% compared to 81.08% for traditional cultures, while also identifying a broader range of pathogens, including 36.36% of bacteria and 74.07% of fungi that were also detected by cultures, plus additional pathogens missed by conventional methods [27].
This capability is invaluable for diagnosing infections with unknown etiology, where routine tests return negative, and for identifying rare or novel pathogens. The initial discovery of the SARS-CoV-2 virus itself was a result of applying mNGS, highlighting its power in outbreak settings against novel threats [27]. Furthermore, mNGS can characterize antimicrobial resistance (AMR) genes, providing concurrent insights into potential treatment challenges. Studies on Mycobacterium tuberculosis have shown high concordance between whole-genome sequencing (WGS) by NGS and phenotypic susceptibility testing, supporting its use in predicting resistance to both first- and second-line therapies [10].
Key Methodologies for Comprehensive Pathogen Detection
Different NGS approaches offer varying levels of breadth and depth, allowing researchers to select the optimal strategy for their specific application.
Table 2: Key NGS Methodologies for Pathogen Identification and Characterization
| Sequencing Methodology | Primary Application & Strength | Typical Target/Approach | Considerations |
|---|---|---|---|
| Shotgun Metagenomics (mNGS) | Unbiased detection of all pathogens in a sample; AMR gene profiling [10] | Sequencing all DNA in a sample; culture-independent | Higher host background; complex bioinformatics [10] |
| 16S rRNA Amplicon Sequencing | Bacterial identification and diversity analysis; cost-effective [28] | Amplification and sequencing of the 16S rRNA gene (bacteria-specific) | Limited to bacteria; cannot detect viruses or fungi [28] |
| ITS Amplicon Sequencing | Fungal identification and mycobiome analysis [28] | Amplification and sequencing of the Internal Transcribed Spacer (ITS) region | Limited to fungi; cannot detect bacteria or viruses [28] |
| Targeted NGS (tNGS) | Rapid, sensitive detection of pre-defined pathogens or resistance genes [10] [26] | Multiplex PCR or hybrid capture to enrich specific targets | Not unbiased; limited to panel content [10] |
| Whole Genome Sequencing (WGS) | High-resolution typing, outbreak tracking, comprehensive AMR detection [10] | Sequencing of the entire genome from a cultured isolate | Requires culture first; not direct from sample [10] |
The relationship between these methodologies and their application in a diagnostic pipeline can be visualized as a decision tree.
Diagram 2: Diagnostic Decision Tree for Selecting Appropriate NGS Methodologies. The choice between unbiased and targeted approaches depends on the clinical or research question and prior knowledge of suspected pathogens.
Deciphering the Complexity of Polymicrobial Infections
The Clinical Burden and Diagnostic Challenge
Polymicrobial infections (PMIs), defined as diseases caused by mixed infections of two or more microorganisms, represent a significant clinical burden, accounting for an estimated 20–50% of severe clinical infection cases globally [25]. In specific contexts like biofilm-associated device infections and diabetic foot infections (DFIs), this rate soars to 60–80% in hospitalized patients [25]. These infections increase the risk of mortality by 2- to 3-fold and extend hospital stays compared to their monomicrobial counterparts [24]. The increased mortality has been associated with inadequate and inappropriate antimicrobial treatments, which occur frequently because conventional diagnostics fail to paint a complete microbial picture [24].
Culture-based methods are particularly inadequate for PMIs due to differential inherent microbial fitness and co-culture conditions that may favor one species over another, prohibiting a comprehensive survey [24]. It is estimated that traditional cultures can miss up to 30–40% of co-pathogens in polymicrobial samples, leading to suboptimal therapy and worsened outcomes [25]. mNGS overcomes this by providing a culture-independent, high-resolution view of the entire microbial community.
mNGS Applications in Major Polymicrobial Infection Types
The ability of mNGS to profile complex microbial communities has proven critical in several infection types:
- Diabetic Foot Infections (DFIs): 60–80% are polymicrobial, involving complex mixtures of Gram-positive cocci (e.g., Staphylococcus aureus), Gram-negative bacilli (e.g., Pseudomonas aeruginosa), and obligate anaerobes. mNGS identifies these consortia, which are directly linked to biofilm formation, AMR, and treatment failure rates up to 30% [25].
- Respiratory Infections: In ventilator-associated pneumonia (VAP), 40–70% of cases involve multidrug-resistant Gram-negative organisms like Acinetobacter baumannii and P. aeruginosa. PMIs in this context have a 15–25% higher ICU mortality. During the COVID-19 pandemic, mortality increased by over 50% owing to polymicrobial coinfections with bacteria and fungi [25].
- Intra-Abdominal Infections (IAIs): PMIs account for over 80% of IAIs following gastrointestinal perforation. mNGS can identify classic combinations like Escherichia coli and Bacteroides fragilis, which synergistically promote greater virulence and abscess formation [25].
- Biofilm-Associated Infections: Infections from indwelling medical devices are fundamentally polymicrobial. Biofilm-embedded communities exhibit a 10- to 1000-fold reduction in antibiotic effectiveness. mNGS can identify the constituent members of these resilient communities, which frequently recur at rates exceeding 20% despite aggressive treatment [25].
Experimental Protocol for Polymicrobial Infection Analysis
Protocol: mNGS for Polymicrobial Community Profiling [10] [29]
Sample Collection & DNA Extraction:
- Collect tissue or fluid from the infection site, ensuring representative sampling. For biofilm infections, sonication of explanted devices can dislodge embedded communities for analysis [30].
- Extract total DNA as described in Section 3.2. Avoid methods that may bias against specific cell wall types (e.g., Gram-positive bacteria).
Shotgun Metagenomic Library Preparation and Sequencing:
- Follow the library preparation steps for shotgun mNGS (Section 3.2) to ensure all genomic material is equally represented.
Bioinformatic Analysis for Community Profiling:
- Taxonomic Profiling: Use tools like Kraken (k-mer based) or MetaPhlAn (marker-gene based) to assign taxonomic labels to each sequencing read against a curated database (e.g., GreenGenes, NCBI) [29].
- Abundance Estimation: Generate a quantitative profile of the microbial community, calculating the relative abundance of each identified taxon.
- Data Visualization: Use tools like Krona to create interactive hierarchical pies of taxonomic abundances, or Pavian for in-depth analysis and comparison of community profiles between samples [29].
Advanced Analysis (Optional):
- Alpha Diversity: Calculate within-sample diversity metrics (e.g., Shannon Index) to compare microbial richness and evenness between patient groups (e.g., severe vs. non-severe COVID-19) [27].
- Beta Diversity: Calculate between-sample diversity metrics (e.g., Bray-Curtis dissimilarity) to visualize overall community structural differences using PCoA plots [27].
- AMR Gene Screening: Align non-human reads to a database of antimicrobial resistance genes (e.g., CARD, MEGARes) to predict the functional resistance potential of the microbial community [10].
Successful implementation of mNGS in a research or clinical setting requires a suite of wet-lab and dry-lab reagents and tools.
Table 3: Essential Research Reagent Solutions for mNGS Workflows
| Category | Specific Tool / Kit / Platform | Primary Function in the Workflow |
|---|---|---|
| Nucleic Acid Extraction | TIANamp Magnetic DNA Kit [26] | Co-extraction of DNA and RNA from clinical samples. |
| Host Depletion | Benzonase-based Kits [10] | Enzymatic degradation of human host nucleic acids to increase microbial sequencing depth. |
| Library Preparation | KAPA HyperPrep Kit [26] | Fragmentation, end-repair, A-tailing, and adapter ligation for Illumina-compatible libraries. |
| Sequencing Platforms | Illumina (NextSeq 1000/2000) [28], Ion Torrent PGM [31], Oxford Nanopore [10] | High-throughput sequencing generating millions to billions of reads. |
| Bioinformatic Tools - Classification | Kraken (k-mer based) [29], MetaPhlAn (marker-based) [29], PathoScope [10] | Taxonomic assignment of sequencing reads to identify pathogens. |
| Bioinformatic Tools - Visualization | Krona [29], Pavian [29] | Interactive visualization of complex taxonomic profiling results. |
| Bioinformatic Tools - Database | NCBI RefSeq, GreenGenes [28] [29] | Curated genomic databases used as a reference for pathogen identification. |
Metagenomic next-generation sequencing represents a cornerstone technology in the new era of infectious disease diagnostics and research. By decisively overcoming the traditional limits of speed, pathogen coverage, and polymicrobial analysis, mNGS provides a powerful, unbiased lens through which to view the microbial world. The quantitative data and detailed protocols outlined in this guide provide a foundation for researchers and drug development professionals to integrate this transformative technology into their work. As sequencing technologies continue to evolve toward portability and lower costs, and as bioinformatic tools become more standardized and accessible, the integration of mNGS into routine clinical practice and clinical trials is poised to expand, ultimately enabling more precise, personalized, and effective management of infectious diseases.
Metagenomic next-generation sequencing (mNGS) is a transformative, non-targeted technique that enables the direct detection and characterization of microbial genomes from clinical samples without prior knowledge of the infectious agent [1]. This approach sequences the total nucleic acids extracted from diverse sample types, allowing for the simultaneous identification of bacteria, viruses, fungi, and parasites, thereby providing a comprehensive view of microbial communities that surpasses traditional culture-based methods [1]. The selection of an appropriate sequencing platform is a critical decision that directly influences the depth, accuracy, and scope of microbial detection in research on bacterial identification. This guide provides an in-depth technical comparison of three major sequencing technologies—Illumina, Oxford Nanopore, and BGI platforms—focusing on their application within metagenomic sequencing workflows for bacterial research.
Core Sequencing Technologies
- Illumina: Utilizes Sequencing by Synthesis (SBS) chemistry. This process involves fluorescently labeled, reversible-terminator nucleotides that are incorporated into growing DNA strands. As each nucleotide is added, a camera captures its fluorescent signal, enabling base determination [32] [33]. This technology is known for its high accuracy and output, making it a dominant platform in production-scale genomics [34] [33].
- Oxford Nanopore Technologies (ONT): Based on the measurement of electrical current changes. Single strands of DNA or RNA are passed through a protein nanopore. Each different nucleotide base disrupts the ionic current flowing through the pore in a characteristic way, and these changes are decoded in real-time to determine the sequence [35] [36]. A key advantage is its ability to sequence ultra-long reads and detect base modifications natively.
- BGI Platforms: Employs a proprietary method called Combinatorial Probe-Anchor Ligation (cPAL). This technology uses DNA nanoball (DNB) arrays, where DNA is amplified into nano-sized balls and deposited on a patterned array. Sequencing is then performed through repeated cycles of probe ligation and imaging [37]. This method is noted for its high accuracy, with a claimed error rate as low as 1 in 100,000 bases [37].
Technical Specifications at a Glance
The following tables summarize the key performance metrics for benchtop and production-scale sequencers from the leading platforms, providing a basis for direct comparison.
Table 1: Key Specifications of Benchtop Sequencing Systems
| Platform / Model | Max Output per Flow Cell | Max Read Length | Key Applications in Metagenomics |
|---|---|---|---|
| Illumina MiSeq (Kit v3) | 13.2–15 Gb [32] | 2 × 300 bp [32] | Small whole-genome sequencing (microbe, virus), 16S metagenomic sequencing [34] |
| Illumina MiSeq (Kit v2) | 7.5–8.5 Gb [32] | 2 × 250 bp [32] | Targeted gene sequencing (amplicon-based), metagenomic profiling [34] |
| Oxford Nanopore MinION | Up to 30 Gb [34] | > 30 kb (ultra-long) [35] | Real-time pathogen detection, shotgun metagenomics, full-length 16S sequencing [38] |
Table 2: Key Specifications of Production-Scale Sequencing Systems
| Platform / Model | Max Output per Flow Cell | Max Read Length | Typical Run Time |
|---|---|---|---|
| Illumina NovaSeq 6000 (S4 Flow Cell) | 2400–3000 Gb [33] | 2 × 150 bp [33] | ~44 hours [33] |
| Illumina NovaSeq X Plus | 8000 Gb [34] | 2 × 150 bp [34] | ~17–48 hours [34] |
| Oxford Nanopore PromethION | 540 Gb [34] | 2 × 300 bp [34] | ~8–44 hours [34] |
Detailed Workflows and Data Analysis
General mNGS Wet and Dry Lab Workflow
The process of metagenomic sequencing consists of two main parts: the wet lab (laboratory testing) and the dry lab (bioinformatic analysis) [1]. The wet lab phase includes sample collection, nucleic acid extraction, library construction, and high-throughput sequencing. The dry lab phase involves data quality control, removal of human host sequences, alignment of sequences to microbial databases, and analysis of drug resistance or virulence genes [1]. The general workflow is depicted below.
Oxford Nanopore-Specific Data Analysis
A distinct advantage of Oxford Nanopore technology is the ability to perform basecalling and analysis in real-time. The core of this process is the conversion of raw electrical signals into nucleotide sequences.
Basecalling Models: Oxford Nanopore provides several basecalling models optimized for different needs [36]:
- Fast Model: Designed to keep up with data generation on most devices; ideal for quick, real-time insights.
- High Accuracy (HAC) Model: Provides higher raw read accuracy than the Fast model; recommended for high-throughput variant analysis.
- Super Accurate (SUP) Model: The most accurate and computationally intensive model; recommended for de novo assembly and low-frequency variant analysis.
Furthermore, designated models are available for the direct detection of base modifications (e.g., 5mC, 5hmC for DNA and m6A for RNA) without additional experiments, a feature unique to nanopore sequencing [35] [36].
Essential Research Reagent Solutions
Successful metagenomic sequencing relies on a suite of specialized reagents and kits for sample and library preparation. The table below details key solutions used in typical workflows.
Table 3: Key Research Reagent Solutions for Metagenomic Sequencing
| Reagent / Kit Name | Platform | Primary Function |
|---|---|---|
| Rapid PCR Barcoding Kit [38] | Oxford Nanopore | Enables quick library preparation and sample multiplexing for rapid pathogen identification. |
| Ultra-long Sequencing Kit (ULK) [35] | Oxford Nanopore | Facilitates the generation of ultra-long reads (>>30 kb), crucial for resolving complex genomic regions and complete genome assembly. |
| Assembly Polishing Kit (APK) [35] | Oxford Nanopore | Used in conjunction with ultra-long reads to achieve high-accuracy, telomere-to-telomere genome assemblies. |
| NovaSeq 6000 Reagent Kits (v1.5, S1-S4) [33] | Illumina | Production-scale sequencing reagents with patterned flow cell technology for high-throughput metagenomic studies. |
| MiSeq Reagent Kits (v2, v3) [32] | Illumina | Benchtop sequencing reagents offering flexibility in output and read length for smaller-scale microbial projects. |
| Agilent SureSelect / Roche NimbleGen [37] | Multiple | Target enrichment platforms used to isolate specific genomic regions of interest, such as the exome, from complex samples. |
Application in Pathogen Metagenomics: A Specific Workflow
Metagenomic sequencing is a key technique for identifying potential pathogens without prior knowledge of microbial sample composition, providing critical insights for outbreak surveillance [38]. Oxford Nanopore's streamlined workflow for respiratory samples exemplifies this application.
- Rapid Identification: The use of the Rapid PCR Barcoding Kit on a MinION or GridION allows for rapid sequencing and analysis, delivering data that can be critical for timely outbreak control [38].
- Comprehensive Detection: The ability to sequence any fragment length enables thorough characterization of mixed microbial samples, simultaneously identifying bacterial, fungal, and viral pathogens [38].
- Overcoming "Dark" Genomes: Short-read technologies are estimated to miss about 8% of the human genome, which includes many disease-relevant repetitive regions. Nanopore technology has been shown to reduce these inaccessible areas by 81%, providing a more complete picture of the genomic landscape [35].
The choice between Illumina, Oxford Nanopore, and BGI sequencing platforms for bacterial metagenomics depends heavily on the specific research goals. Illumina platforms offer high-throughput and base-level accuracy ideal for large-scale, quantitative microbial profiling. Oxford Nanopore provides real-time data, long reads that resolve complex regions, and direct epigenetic detection, which are advantageous for rapid pathogen identification and complete genome assembly. BGI's technology, with its cPAL chemistry and DNB arrays, presents an alternative with very high claimed accuracy for comprehensive variant detection. As these technologies continue to evolve, advances in bioinformatics, chemistry, and hardware will further consolidate mNGS as a pivotal, comprehensive tool for pathogen detection and characterization in modern research.
From Bench to Bedside: mNGS Workflow Optimization and Clinical Deployment
Metagenomic sequencing has revolutionized the study of microbial communities, enabling researchers to decipher the genetic material of entire ecosystems directly from environmental or clinical samples. For bacterial identification research, the fidelity of the final genomic data is profoundly dependent on the initial wet-lab procedures. This guide details three critical wet-lab steps—sample collection, host DNA depletion, and library preparation—framed within the context of metagenomic sequencing. The choices made during these phases are not merely procedural; they directly influence downstream outcomes, including the accuracy of taxonomic profiling, the ability to detect low-abundance pathogens, and the overall reliability and reproducibility of the research [39] [10]. The following sections provide an in-depth technical examination of these steps, summarizing key quantitative data for informed decision-making and outlining detailed protocols.
Sample Collection and Preservation
The foundation of any successful metagenomic study is the integrity of the initial sample. Inadequate collection or preservation can introduce biases that no downstream analysis can correct.
Core Principles
The primary goal during sample collection is to obtain a representative microbial community while minimizing any changes to its composition from the point of collection until nucleic acid extraction. Key considerations include:
- Immediate Stabilization: Microbial activities continue after sample collection. For many sample types, especially those with high microbial biomass, immediate freezing at -80°C is the gold standard. However, when freezing is not immediately possible, such as during field collection, the use of commercial stabilization solutions is critical. These solutions lyse cells and inhibit nuclease activity, preserving the nucleic acid profile at the moment of preservation [10].
- Avoiding Contamination: The use of sterile, DNA-free collection containers and reagents is paramount. This is particularly crucial for low-biomass samples (e.g., tissue biopsies, cerebrospinal fluid), where contaminating DNA from collection kits or the environment can constitute a significant portion of the sequenced material [10].
- Sample-Specific Protocols: The optimal method varies by sample type. For instance, swabs from mucosal surfaces may require different handling than fecal samples or water samples from environmental sources.
Experimental Protocol: Fecal Sample Collection for Gut Microbiome Studies
Materials:
- DNA/RNA-free collection tube with stabilizer (e.g., DNA/RNA Shield)
- Sterile spatula or swab
- Personal protective equipment (PPE)
- -80°C freezer or dry ice for immediate storage
Methodology:
- Using a sterile spatula, collect approximately 100-200 mg of fecal material.
- Immediately place the sample into the collection tube containing a DNA/RNA stabilizer solution. Ensure the sample is fully submerged.
- Vortex the tube vigorously for at least 30 seconds to ensure homogenization and complete lysis of cells upon contact with the stabilizer.
- Label the tube clearly and store at 4°C for short-term transport (up to 1 week) or at -80°C for long-term storage.
- Record all metadata, including time of collection, patient/donor identifier, and any clinical symptoms or dietary information, as this contextual data is essential for later interpretation.
Host DNA Depletion
In clinical metagenomics, where samples are often dominated by host DNA (e.g., human DNA in blood or tissue), depleting this host material is a critical step to increase the sensitivity for detecting bacterial pathogens.
Host DNA depletion techniques selectively remove or degrade host nucleic acids, thereby enriching the relative proportion of microbial DNA. The efficiency of depletion is a major factor in the success of sequencing low-biomass infections [10]. Common methods include:
- Enzymatic Digestion: Uses nucleases that are specific to mammalian cells (e.g., Benzonase) which digest DNA in the extracellular environment or in host cells that have been selectively lysed using mild detergents. The microbial cells, with their intact cell walls, are protected from digestion. After digestion, the nuclease is inactivated, and the microbial DNA is extracted.
- Probe-Based Capture: Involves designing biotinylated oligonucleotide probes that are complementary to highly conserved regions of the host genome (e.g., human rRNA genes). The probes are hybridized to the sample DNA, and host-probe complexes are removed using streptavidin-coated magnetic beads. This method can achieve high levels of depletion but is more costly and complex.
The choice of method involves a trade-off between depletion efficiency, cost, and potential loss of some microbial taxa.
Performance Comparison of Depletion Methods
The following table summarizes the key characteristics of the primary host DNA depletion methodologies.
Table 1: Comparison of Host DNA Depletion Methods
| Method | Mechanism | Typical Depletion Efficiency | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Enzymatic Digestion | Selective lysis of host cells followed by nuclease digestion of exposed DNA. | 70-95% [10] | Cost-effective; relatively simple workflow; maintains microbial integrity. | Potential for incomplete lysis or digestion; may not be effective for all sample types. |
| Probe-Based Capture | Hybridization and magnetic bead removal of host DNA sequences. | 90-99.9% [10] | Very high depletion efficiency; can be tailored to specific hosts. | Higher cost; requires specialized probe sets; potential for co-depletion of microbes with similar sequences. |
Library Preparation for Metagenomic Sequencing
Library preparation is the process of converting the extracted DNA into a format compatible with high-throughput sequencing platforms. The chosen protocol can significantly impact data quality, including fragment length distribution, GC bias, and the recovery of endogenous microbial DNA [39].
Fundamentals of Library Construction
Most next-generation sequencing (NGS) library prep protocols share common steps: DNA fragmentation, end-repair, adapter ligation, and library amplification. However, specific adaptations are crucial for metagenomic applications, particularly when dealing with degraded DNA or low-input samples.
Comparison of Common Library Prep Methods
The two predominant approaches in metagenomics are double-stranded and single-stranded library methods. A systematic comparison is essential for selecting the appropriate protocol.
Table 2: Characteristics of Library Preparation Methods for Metagenomics
| Method | Principle | Ideal Fragment Size | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Double-Stranded (DSL) [39] | Ends of double-stranded DNA molecules are repaired and ligated to double-stranded adapters. | >100 bp | Widely used; robust and cost-effective; shorter protocol duration. | Lower conversion efficiency of short, fragmented DNA; higher clonality [39]. |
| Single-Stranded (SSL) [39] | DNA is denatured into single strands before adapter ligation, enabling higher conversion of short fragments. | <100 bp | Superior for degraded/low-input samples; higher conversion efficiency; lower clonality [39]. | Historically more expensive and time-consuming; though newer methods (e.g., Santa Cruz Reaction) have addressed this [39]. |
Experimental Protocol: Double-Stranded Library Preparation for Illumina
This is a generalized protocol based on common commercial kits (e.g., Illumina Nextera Flex).
Materials:
- Purified DNA (1-100 ng in volume)
- Tagment DNA Buffer
- Amplicon Tagment Mix
- Neutralize Tagment Buffer
- PCR Master Mix
- Unique Dual Indexes (UDIs)
- Magnetic beads (e.g., SPRIselect)
- Fresh 80% Ethanol
- Nuclease-free water
- Thermal cycler, magnetic stand, and microcentrifuge
Methodology:
- Tagmentation: Combine DNA, Tagment DNA Buffer, and Amplicon Tagment Mix in a PCR tube. Incubate in a thermal cycler at 55°C for 10-15 minutes. This simultaneously fragments and tags the DNA with adapter sequences.
- Neutralization: Add Neutralize Tagment Buffer to stop the tagmentation reaction. Mix thoroughly by pipetting.
- PCR Amplification: To the neutralized tagmentation reaction, add PCR Master Mix and a unique pair of Dual Index Primers. Perform PCR amplification with the following cycling conditions:
- 72°C for 3 minutes
- 95°C for 30 seconds
- 12-15 cycles of: 95°C for 10 seconds, 55°C for 30 seconds, 72°C for 30 seconds
- 72°C for 5 minutes
- Hold at 4°C
- Library Clean-up: Add a calculated volume of magnetic beads to the PCR product to purify the final library. Incubate, separate on a magnetic stand, wash twice with 80% ethanol, and elute in nuclease-free water.
- Quality Control: Quantify the library using a fluorometric method (e.g., Qubit) and assess the size distribution using a bioanalyzer or tape station. The library is now ready for sequencing.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and their critical functions in the metagenomic wet-lab workflow.
Table 3: Research Reagent Solutions for Metagenomic Workflows
| Reagent / Kit | Function | Application Note |
|---|---|---|
| DNA/RNA Stabilization Solution | Preserves nucleic acid integrity at room temperature by inactivating nucleases. | Essential for field collections and clinical settings where immediate freezing is not feasible [10]. |
| Methylated DNA Depletion Kit | Selectively removes mammalian (host) DNA based on differential methylation patterns. | An alternative to probe-based methods; effectiveness depends on the sample type and host organism [10]. |
| PCR-Free Library Prep Kit | Prepares sequencing libraries without PCR amplification. | Avoids PCR bias and improves coverage uniformity, but requires higher input DNA [39]. |
| Magnetic Beads (SPRI) | Size-selects and purifies nucleic acids based on binding to carboxylated beads in PEG buffer. | A versatile tool for clean-up and size selection post-fragmentation and post-amplification. |
| High-Fidelity DNA Polymerase | Amplifies library fragments with low error rates during PCR. | Critical for minimizing mutations during the limited-cycle amplification step of library prep. |
Workflow Visualization and Emerging Methods
The following diagram illustrates the logical progression of the critical wet-lab steps discussed in this guide, from sample to sequencer.
An emerging method that redefines targeted sequencing is adaptive sampling, a software-based technique available on Oxford Nanopore Technologies (ONT) platforms. Unlike traditional wet-lab enrichment, adaptive sampling performs target selection in silico during the sequencing run itself. As a DNA strand is sequenced in real-time, its initial sequence is basecalled and matched against a user-provided reference. If it is not a target of interest (or is a target for depletion, like host DNA), a voltage reversal is applied to eject the molecule from the pore, freeing it to sequence another strand. This enables PCR-free, probe-free enrichment or depletion, preserving long reads and native DNA modifications [40]. This method is particularly powerful for depleting host DNA in microbial samples or enriching for rare pathogens directly during sequencing, representing a significant shift in the metagenomic workflow [40].
Metagenomic sequencing has revolutionized microbiology by enabling the direct, unbiased study of genomic material from complex microbial communities, bypassing the need for culture-based methods [41]. This approach is transforming clinical diagnostics, public health, and microbial ecology by allowing researchers to identify novel species, characterize community structures, and detect pathogens directly from samples like tissue, soil, or water [41] [42]. The core challenge lies in computationally processing the millions of short sequences generated to accurately identify all species present amidst substantial host genetic contamination and sequencing errors [41] [43].
A robust bioinformatic pipeline is therefore essential for meaningful biological interpretation. This in-depth technical guide outlines the three critical stages of metagenomic analysis for bacterial identification: initial quality control of raw sequencing data, removal of host-derived sequences, and final taxonomic classification. We frame this within the context of a broader thesis on metagenomic sequencing, providing researchers and drug development professionals with standardized methodologies, performance benchmarks of current tools, and practical implementation protocols to ensure accurate and reproducible results.
The standard bioinformatic pipeline for metagenomic analysis proceeds through several critical stages, from raw data to biological interpretation. The following diagram illustrates the complete workflow, highlighting the three core components covered in this guide.
Stage 1: Quality Control of Raw Sequencing Data
The Importance of Quality Control
Quality control (QC) is the foundational first step in any metagenomic workflow. Modern sequencers are imperfect, generating various errors and technical artifacts that can severely impact downstream analysis [44]. Effective QC assesses data integrity, identifies issues related to sequencing instruments or library preparation, and filters or trims reads to maximize the number of sequences that can be accurately aligned and classified [45] [42]. The exponential growth of sequencing initiatives has led to the establishment of global standards, such as the GA4GH Whole Genome Sequencing Quality Control Standards, to ensure consistent, reliable, and comparable genomic data quality across institutions [46].
Understanding FASTQ Format and Quality Scores
Sequencing data is typically delivered in FASTQ format. Each read is represented by four lines containing the sequence identifier, the nucleotide sequence, a separator (+), and a quality score string [44]. The quality of each base is encoded as an ASCII character representing the Phred quality score (Q), which quantifies the probability of an incorrect base call [44]. The score is calculated as:
Q = -10 × log₁₀(P)
where P is the probability of an error. This means a base with Q=30 has a 1 in 1000 chance of being incorrect (99.9% accuracy) [44].
Essential QC Metrics and Tools
Table 1: Key Quality Control Metrics for Metagenomic Data
| Metric | Description | Acceptable Range |
|---|---|---|
| Per-base Sequence Quality | Distribution of quality scores (Q) at each position across all reads. | Q > 20 for most bases [45]. |
| GC Content | Distribution of the proportion of G and C bases across all reads. | Should match the expected GC distribution of the sample [44]. |
| Adapter Content | Percentage of reads containing adapter sequences. | As low as possible; typically < 1-5% [45]. |
| Read Length | Distribution of the length of sequences. | Varies by technology; should be consistent with sequencing protocol. |
| Sequence Duplication | Percentage of duplicate reads in the library. | Lower is better; indicates good library complexity [45]. |
Several computational tools are available for assessing these metrics. FastQC is one of the most well-known, providing an overview of data quality through interactive graphs and plots [45] [44]. For long-read data from platforms like Oxford Nanopore Technologies, NanoPlot and PycoQC are specialized tools that visualize read quality and length distributions [45].
Read Trimming and Filtering Protocols
If QC reports indicate issues like poor quality ends or adapter contamination, reads must be trimmed or filtered. This step removes low-quality data, improving the accuracy of downstream mapping and assembly algorithms [45].
Protocol: Standard Read Trimming with Cutadapt/Fastp
- Identify Adapters: Determine the adapter sequences used during library preparation.
- Set Quality Threshold: Define the minimum quality score (e.g., Q20) for trimming. Bases below this threshold will be removed from the ends of reads.
- Set Minimum Length: Define the minimum acceptable read length post-trimming (e.g., 50 bp). Reads shorter than this will be discarded.
- Execute Trimming: Run the trimming tool. For example, a basic Cutadapt command might look like:
cutadapt -a ADAPTER_SEQ -q 20 --minimum-length 50 -o output_trimmed.fastq input.fastq - Re-assess Quality: Run FastQC again on the trimmed files to confirm quality improvement [45] [44].
For long reads, tools like Chopper (for filtering) and Porechop (for adapter removal) are commonly used within workflows such as NanoGalaxy [45].
Stage 2: Host Sequence Removal
The Critical Need for Host Decontamination
In metagenomic studies of host-associated environments (e.g., human tissue, sputum, or blood), the extracted DNA is predominantly from the host. The human genome is ~3 Gb, while a bacterial genome is ~1-5 Mb, and a viral genome is ~30 kb—a difference of up to five orders of magnitude [43]. Consequently, over 99% of sequences in a metagenomic dataset can originate from the host, drastically diluting the microbial signal, consuming sequencing resources, and obscuring the detection of pathogens [43]. Effective host sequence removal is therefore a critical prerequisite, increasing the sensitivity of microbial detection by 1-2 orders of magnitude and raising the proportion of target sequences from less than 1% to 10-50% [43].
Methods for Host DNA Removal
Host DNA can be addressed through both wet-lab (experimental) and computational methods. A combined approach often yields the best results.
Table 2: Comparison of Host DNA Removal Methods
| Method | Principle | Advantages | Limitations | Best For |
|---|---|---|---|---|
| Physical Separation (e.g., Centrifugation, Filtration) | Exploits density/size differences between host cells and microbes. | Low cost, rapid operation. | Cannot remove intracellular or free host DNA from lysed cells. | Virus enrichment, body fluid samples [43]. |
| Targeted Amplification (e.g., 16S PCR, MDA) | Selectively amplifies conserved microbial genes. | High sensitivity and specificity for known targets. | Primer bias affects quantification; not assumption-free. | Low biomass samples, known pathogen screening [43]. |
| Host Genome Digestion (e.g., DNase I) | Enzymatically degrades exposed host DNA while microbes are fixed. | Efficient removal of free host DNA. | Risk of damaging microbial cell integrity. | Tissue samples with high host content [43]. |
| Bioinformatics Filtering | Maps reads to a host reference genome and removes matches. | No experimental manipulation; highly compatible. | Dependent on a complete host reference genome; cannot remove sequences homologous to host (e.g., HERVs). | Routine samples, final data cleaning step [43] [47]. |
Benchmarking Bioinformatics Tools for Host Removal
Computational decontamination is a vital final defense. Tools for this task typically use alignment (e.g., Bowtie2, BWA, Minimap2) or k-mer-based classification (e.g., Kraken2) to identify host-derived reads [43] [47]. A recent benchmark study evaluated multiple pipelines using synthetic and real datasets:
Table 3: Performance of Selected Host Removal Tools on Simulated Nanopore Data
| Tool / Pipeline | Rate (reads/sec) | Memory (GB) | Sensitivity | Specificity | Youden's Index |
|---|---|---|---|---|---|
| Kraken2 (HPRC database) | 2,384 | 4.7 | 0.9998 | 0.9999 | 0.9998 |
| Kraken2 (Default database) | 1,618 | 4.1 | 0.9998 | 1.0 | 0.9998 |
| Minimap2 | 412 | 9.0 | 0.9998 | 0.9999 | 0.9998 |
| Hostile | 263 | 12.8 | 0.9998 | 1.0 | 0.9998 |
| HRRT | 281 | 1.0 | 0.9809 | 1.0 | 0.9809 |
Data adapted from [48]. HPRC: Human Pangenome Reference Consortium database. Youden's index (Sensitivity + Specificity - 1) balances both metrics.
Another study, evaluating the tool HoCoRT, found that for short-read data (e.g., Illumina), the optimal combination of speed and accuracy was achieved with BioBloom, Bowtie2 in end-to-end mode, and HISAT2. Kraken2 was the fastest but with a slight trade-off in accuracy. For long reads, a combination of Kraken2 followed by Minimap2 achieved the highest accuracy, detecting 59% of human reads [47].
Recommended Protocol and Impact on Analysis
Protocol: Host Read Removal with Kraken2 and a Custom Database
- Obtain Host Genome: Download a comprehensive host reference, such as the CHM13v2 human genome assembly.
- Build a Custom Database (Recommended): For the best balance of accuracy and computational efficiency, especially on laptop-grade hardware, build a Kraken2 database from multiple human genomes (e.g., the HPRC pangenome) [48].
kraken2-build --download-library human --db ./my_kraken_db - Classify Reads: Run Kraken2 against the database to generate a report and file with classification labels.
kraken2 --db ./my_kraken_db --paired input_1.fastq input_2.fastq --report kr2_report.txt --output kr2_output.txt - Extract Non-Host Reads: Use auxiliary tools to extract reads not classified as host (e.g., Homo sapiens).
extract_kraken_reads.py -k kr2_output.txt -s input.fastq -o microbial_reads.fastq -t 9606 --exclude
The impact of successful host removal is profound. Studies on colon biopsy samples show that it significantly increases the number of microbial reads detected, enhances bacterial species richness (alpha-diversity), and improves coverage of bacterial genes without significantly altering the overall perceived structure of the microbial community [43].
Stage 3: Taxonomic Classification
Principles of Taxonomic Classification
Taxonomic classification is the process of assigning individual sequencing reads to specific taxonomic groups (e.g., phylum, genus, species) by comparing them to reference databases of known genomic sequences [41] [49]. This step answers the fundamental question: "What species are present in my sample?" [42]. This is distinct from, though related to, taxonomic profiling, which estimates the relative abundances of taxa without necessarily classifying every read [41]. The sheer volume of data and the exponential growth of reference databases have driven the development of highly efficient algorithms that trade some sensitivity for massive gains in speed compared to traditional tools like BLAST [41].
Classification Algorithms and Reference Databases
Classifiers can be categorized by their underlying comparison strategy:
- DNA-to-DNA (BLASTn-like): Compares reads directly to a database of genomic DNA sequences. Generally faster but potentially less sensitive to evolutionarily distant relatives [41] [49].
- DNA-to-Protein (BLASTx-like): Translates reads in all six frames and compares them to a protein sequence database. More computationally intensive but often more sensitive for detecting novel species due to the higher conservation of amino acid sequences [41] [49].
- Marker-Based: Uses a pre-defined set of clade-specific marker genes (e.g., the 16S rRNA gene for bacteria). Very fast and efficient but can introduce bias if markers are not universally present or are unevenly distributed among microbes of interest [41] [49] [50].
The choice of reference database is paramount. Popular databases include RefSeq (curated complete genomes), the NCBI nucleotide collection (nt, more comprehensive but less curated), and SILVA (for 16S rRNA) [41]. The classifier's performance is directly dependent on the database's completeness and quality. A key challenge is that classifiers distributed with pre-compiled databases may yield performance differences attributable to the database itself, not the algorithm [41] [49]. Therefore, benchmarking studies that use a uniform database are most informative for comparing classifier performance [41].
Benchmarking Classifier Performance
Classifier performance is typically measured using precision (the proportion of identified species that are true positives) and recall (the proportion of true positive species that are successfully identified) [41]. The F1 score, the harmonic mean of precision and recall, provides a single metric balancing both [41] [50]. Since users often filter out low-abundance taxa, the Area Under the Precision-Recall Curve is a more robust metric than a single F1 score [41].
A comprehensive benchmark of 20 tools highlighted that no single "best" classifier exists; the choice depends on the application and requirements [41]. A more recent benchmark focusing on nanopore data for defined mock communities categorized classifiers into three groups [49]:
- Low Precision / High Recall: Most classifiers fall here, though precision can be improved with abundance filtering.
- Medium Precision / Medium Recall
- High Precision / Medium Recall
Specialized long-read classifiers like MetaMaps, MEGAN-LR, and CCMetagen generally show better performance on nanopore data [49]. CCMetagen, which uses the KMA aligner, has been shown to achieve the highest precision and F1 scores in identifying both bacterial and fungal taxa, substantially outperforming other commonly used software, especially when using the entire NCBI nt database [50].
Table 4: Performance of Selected Taxonomic Classifiers on Bacterial Communities
| Classifier | Type | Key Characteristic | Reported Performance |
|---|---|---|---|
| Kraken2 [49] | k-mer-based (DNA-to-DNA) | Very fast, low memory. | High recall, but can have lower precision leading to false positives [49] [50]. |
| Centrifuge [50] | DNA-to-DNA | Uses a novel indexing scheme for efficiency. | Very high recall, but very low precision (reported 6950 species in a 30-species mock community) [50]. |
| CCMetagen [50] | Alignment-based (KMA) | Uses ConClave sorting for highly accurate alignments. | Highest precision and F1 scores in benchmarks for bacteria and fungi [50]. |
| MetaPhlAn2/3 [49] | Marker-based (Profiler) | Relies on clade-specific marker genes. | Fast, but a large fraction of reads remain unclassified [49]. |
Recommended Classification Protocol
Protocol: Taxonomic Classification with CCMetagen
- Install CCMetagen: The pipeline is available via Conda or GitHub. It requires KMA and a reference database.
- Select a Database: For comprehensive identification of eukaryotes and prokaryotes, the NCBI
ntdatabase is recommended. For faster, more specific analysis, a RefSeq database can be used. - Run the CCMetagen Pipeline:
a. Map reads with KMA:
kma -i reads.fastq -o output -t_db reference_database.b. Process alignments with CCMetagen:CCMetagen.py -i output.res -o Results - Interpret Output: CCMetagen produces a ranked taxonomic classification file and interactive Krona plots for visualization [50].
The Scientist's Toolkit
Table 5: Essential Research Reagent Solutions for Metagenomic Analysis
| Category | Tool / Resource | Primary Function |
|---|---|---|
| Quality Control | FastQC [45] [44] | Provides a quick overview of raw read quality through multiple diagnostic plots. |
| NanoPlot / PycoQC [45] | Generates quality control plots and summaries for long-read (ONT) data. | |
| Cutadapt / Trimmomatic [45] [44] | Trims adapter sequences and low-quality bases from read ends. | |
| Host Removal | Kraken2 [48] [47] | k-mer-based taxonomic classifier; fast and efficient for host read identification. |
| Bowtie2 [43] [47] | An alignment tool that can be used in end-to-end mode for highly accurate host read mapping. | |
| Minimap2 [48] [47] | A versatile aligner for long reads that is effective for mapping to a host genome. | |
| HoCoRT [47] | A user-friendly, modular tool that wraps multiple host-removal methods into a single pipeline. | |
| Taxonomic Classification | CCMetagen [50] | A highly accurate pipeline for identifying prokaryotes and eukaryotes, excellent for comprehensive surveys. |
| Kraken2 [49] | A very fast k-mer-based classifier useful for rapid profiling of microbial communities. | |
| MetaPhlAn2/3 [49] | A marker-based profiler that estimates taxonomic abundances quickly and efficiently. | |
| Reference Databases | NCBI RefSeq [41] | A curated collection of complete microbial genomes; high quality but less comprehensive. |
| NCBI nucleotide (nt) [41] [50] | A comprehensive but less curated database; enables detection of species with incomplete genome data. | |
| Custom Pangenome DBs [48] | User-built databases (e.g., from HPRC) that can improve accuracy and reduce computational load for specific tasks. |
Integrated Analysis Workflow
The final stage of the pipeline involves integrating the outputs from the previous steps into a cohesive analysis. The following diagram summarizes the logical flow and key decision points from raw data to a finalized taxonomic profile.
A rigorous, standardized bioinformatic pipeline is the backbone of reliable metagenomic research for bacterial identification. This guide has detailed the three pillars of this pipeline: Quality Control to ensure data integrity, Host Sequence Removal to enrich for microbial signals, and Taxonomic Classification to identify the community members. By leveraging benchmarked tools like FastQC, Kraken2 with custom databases, and CCMetagen, researchers can achieve accurate, reproducible results. As sequencing technologies and computational methods continue to evolve, ongoing benchmarking and adherence to global quality standards will be crucial for advancing our understanding of microbial worlds in health, disease, and the environment.
Clinical Applications in Respiratory Infections, Sepsis, and Central Nervous System Infections
Metagenomic next-generation sequencing (mNGS) is a high-throughput sequencing method that enables the unbiased detection of all nucleic acids (DNA and RNA) in a clinical sample without prior knowledge of the causative organisms [51] [2]. This technology represents a paradigm shift from traditional, targeted diagnostic methods like culture and polymerase chain reaction (PCR) to a comprehensive approach capable of identifying bacteria, viruses, fungi, and parasites in a single assay [51]. The core strength of mNGS lies in its hypothesis-free nature, making it particularly valuable for diagnosing challenging, rare, or novel pathogens that evade conventional testing [51] [52]. As sequencing costs decrease and bioinformatic capabilities advance, mNGS is rapidly moving from research settings into clinical laboratories, transforming the landscape of infectious disease diagnosis and management [52].
The workflow involves multiple critical steps: nucleic acid extraction from the sample, library preparation, high-throughput sequencing, and sophisticated bioinformatic analysis to classify sequences by comparing them to comprehensive genomic databases [51] [53]. Two primary metagenomic approaches are employed: targeted sequencing, which amplifies conserved regions like 16S rRNA for bacteria or ITS for fungi, and shotgun sequencing, which indiscriminately sequences all nucleic acids in a sample [51]. While targeted sequencing provides great depth for specific genomic regions, shotgun sequencing offers greater resolution for species identification, can assess microbial function, and is capable of discovering novel organisms [51].
mNGS Workflow and Technologies
The successful application of mNGS in clinical settings relies on a standardized, multi-stage process. The following diagram illustrates the complete workflow from sample collection to clinical diagnosis.
Detailed Experimental Protocol
The mNGS methodology requires meticulous execution at each stage to ensure reliable results:
Sample Collection and Processing: For cerebrospinal fluid (CSF) analysis, 1.5-3 ml is collected via lumbar puncture [53]. The sample is vigorously agitated with 0.5 mm glass beads for 30 minutes for mechanical disruption, followed by the addition of lysozyme for enzymatic wall-breaking reaction [53].
Nucleic Acid Extraction: DNA is extracted using commercial kits (e.g., TIANamp Micro DNA Kit) according to manufacturer's protocols [53]. For RNA viruses, extracted RNA undergoes reverse transcription to generate single-strand cDNA, followed by synthesis of double-strand cDNA [53].
Library Preparation: DNA libraries are constructed through enzymatic fragmentation (37°C for 20 minutes), followed by end repair, adapter ligation, and PCR amplification using specialized kits (e.g., PMseq RNA Infection Pathogen High-throughput Detection Kit) [53]. Each library is uniquely barcoded to enable multiplexing.
Sequencing: Quality-approved libraries are pooled in equimolar amounts, converted into DNA nanoballs (DNBs), and sequenced on platforms such as BGISEQ-50/MGISEQ-2000 [53]. Negative controls are included in each run to monitor contamination.
Bioinformatic Analysis: Raw sequences are filtered to remove low-quality reads, then mapped to the human reference genome (hg38) using Burrows-Wheeler alignment to subtract human sequences [53]. The remaining data is aligned against pathogen-specific databases (e.g., RefSeq) containing 4945 viral taxa, 6350 bacterial genomes, 1064 fungi, and 234 parasites associated with human infections [53].
mNGS in Central Nervous System (CNS) Infections
CNS infections represent one of the most established applications for mNGS, particularly when conventional diagnostics fail. The technique demonstrates exceptional performance in diagnosing meningitis and encephalitis, where rapid pathogen identification is critical for patient outcomes.
Diagnostic Performance in CNS Infections
Recent prospective comparative studies have quantified the advantages of mNGS over conventional methods for CNS infection diagnosis.
Table 1: Diagnostic Performance of mNGS vs. Conventional Culture in Suspected CNS Infections (n=110) [53]
| Diagnostic Metric | mNGS Method | Conventional CSF Culture |
|---|---|---|
| Pathogen Detection Rate | 77.11% (62/69) | 6.36% (7/110) |
| Clinically Confirmed True Positives | 49.09% (54/110) | Not specified |
| Average Turnaround Time | ≤24 hours | 72-120 hours |
| Independent Predictive Value | Yes (p<0.05) | Not significant |
The data demonstrates mNGS's superior sensitivity and markedly faster turnaround time compared to culture, which is critical for timely therapeutic intervention [53]. mNGS was identified as an independent predictor of CNS infection through logistic regression analysis, alongside CSF protein and glucose levels [53]. The area under the curve (AUC) for mNGS in diagnosing CNS infections was 0.794, indicating robust diagnostic accuracy [53].
Clinical Impact on Patient Management
The implementation of mNGS for CNS infection diagnosis directly influences clinical decision-making and patient outcomes. Patients with CNS infections confirmed by mNGS had significantly higher ICU admission rates, prolonged hospital stays, and increased healthcare costs compared to the non-infection group, reflecting the severity of these conditions [53]. Critically, mNGS results led to targeted adjustments in antimicrobial regimens, optimizing therapy and potentially improving outcomes [53].
mNGS in Sepsis and Respiratory Infections
While the provided search results focus more prominently on CNS applications, mNGS shows growing importance in sepsis and respiratory infections, where comprehensive pathogen detection is equally critical.
Application in Sepsis
Sepsis remains a life-threatening condition with high mortality, accounting for 19.7% of global deaths [53]. mNGS offers a powerful approach for pathogen detection in bloodstream infections, especially when conventional cultures are negative or delayed.
- Cell-Free DNA Sequencing: mNGS tests analyzing microbial cell-free DNA from plasma have been clinically validated for sepsis, enabling non-invasive detection of pathogens without prior blood culture [52].
- Polymicrobial Infections: mNGS excels at characterizing polymicrobial infections that challenge traditional diagnostic methods, particularly through its unbiased approach [2].
- Antimicrobial Resistance Detection: While not a primary focus in the available literature, mNGS has potential for detecting antimicrobial resistance genes, contributing to more targeted therapy [52].
Application in Respiratory Infections
Lower respiratory tract infections represent another promising application for mNGS, particularly in complex cases and immunocompromised patients.
- Comprehensive Pathogen Detection: mNGS can simultaneously identify viruses, bacteria, and fungi in respiratory samples (BAL, sputum), providing a complete picture of the respiratory microbiome [52].
- Integrated Host Response Analysis: Combining microbial metagenomic data with host gene expression (transcriptomics) improves diagnostic accuracy for lower respiratory tract infections in critically ill adults [52].
- Outbreak Investigation: mNGS has been utilized to investigate outbreaks of respiratory pathogens, enabling precise strain identification and tracking of transmission routes [52].
Comparative Analysis of Diagnostic Methods
Understanding the position of mNGS within the broader diagnostic landscape is essential for appropriate clinical implementation.
Table 2: Comparison of Conventional Diagnostic Methods vs. mNGS [51]
| Method | Advantages | Disadvantages | Turnaround Time |
|---|---|---|---|
| Culture | Gold standard; low cost; high specificity | Low sensitivity; cannot identify fastidious organisms; manual operation | 3-5 days (up to 1-2 weeks for slow growers) |
| Immunology Assay | Easy operation; relatively low price; high throughput | Low sensitivity and specificity; cross-reactivity | Several hours |
| PCR Assay | High sensitivity; quantitative; multiplexing | Only identifies specific pre-targeted organisms | Several hours |
| mNGS | Unbiased detection; discovers novel/rare pathogens; comprehensive | High cost; complex analysis; contamination risk; cannot distinguish live/dead organisms | 24-72 hours (average 48 hours) |
mNGS fills a critical diagnostic gap, especially for difficult-to-detect, rare, and novel pathogens that evade conventional methods [51]. Approximately 40-50% of CNS infections historically lacked a definitive pathogen diagnosis, a gap mNGS is particularly suited to address [51].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of mNGS requires specific reagents and computational resources throughout the workflow.
Table 3: Essential Research Reagents and Materials for mNGS Workflow
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of DNA and RNA from clinical samples | TIANamp Micro DNA Kit (DP316), TIANamp Micro RNA Kit (DP431) [53] |
| Library Preparation Kits | Fragment processing, adapter ligation, amplification | PMseq RNA Infection Pathogen High-throughput Detection Kit [53] |
| Enzymes | DNA fragmentation, reverse transcription, amplification | Lysozyme (cell wall disruption), reverse transcriptase [53] |
| Sequencing Platforms | High-throughput nucleic acid sequencing | BGISEQ-50/MGISEQ-2000, Illumina (iSeq 100, MiniSeq, MiSeq) [51] [53] |
| Bioinformatic Tools | Sequence alignment, human read removal, pathogen classification | Burrows-Wheeler Aligner (BWA) for human sequence subtraction (hg38) [53] |
| Reference Databases | Pathogen identification and classification | Pathogens Metagenomics Database (RefSeq): 4945 viral taxa, 6350 bacterial genomes, 1064 fungi, 234 parasites [53] |
Technical Considerations and Implementation Challenges
Despite its promise, several significant hurdles must be addressed for widespread clinical adoption of mNGS. The following diagram outlines the primary challenges and their relationships.
Key Challenge Areas
Bioinformatic Complexity: The analysis of mNGS data generates massive, complex datasets that require sophisticated computational tools and expertise not routinely available in clinical microbiology laboratories [51] [2]. Lack of universal workflow validation and standardized quality assurance remains a significant hurdle [51].
Clinical Interpretation: Perhaps the most significant challenge is distinguishing true pathogens from background contamination or colonization [2]. The detection of microbial sequences does not necessarily indicate they are contributing to the patient's disease, requiring careful clinical correlation [2].
Technical Limitations: mNGS can be insensitive in samples with high host nucleic acid background (e.g., CSF with high cell count) or low microbial biomass [51]. Like PCR, it cannot distinguish between viable and non-viable organisms, potentially detecting nucleic acids from dead pathogens after successful treatment [51].
Regulatory and Validation Hurdles: Currently, no FDA-cleared or approved mNGS tests exist for general microbial detection, though CLIA-certified laboratories offer testing [2]. Rigorous clinical utility and cost-effectiveness studies are needed before mainstream adoption [2].
mNGS represents a transformative technology for diagnosing infectious diseases, with demonstrated clinical value in CNS infections, sepsis, and respiratory infections. Its unbiased, comprehensive nature offers a powerful alternative to conventional diagnostic methods, particularly for difficult-to-diagnose cases. While challenges remain in standardization, interpretation, and integration into clinical workflows, ongoing advancements in sequencing technologies and bioinformatic analysis are steadily addressing these limitations. As validation studies accumulate and costs decrease, mNGS is poised to become an increasingly essential tool in clinical microbiology, ultimately enabling more precise and timely treatment for patients with severe infections.
Lower respiratory tract infections (LRTIs) represent a significant global health challenge, remaining a leading cause of morbidity and mortality worldwide despite advances in antimicrobial therapy [54] [55]. The etiological landscape of LRTIs is highly diverse, encompassing Gram-positive and Gram-negative bacteria, atypical pathogens, viruses, and fungi, creating substantial diagnostic challenges [56]. Traditional pathogen identification systems, primarily relying on conventional culture techniques, polymerase chain reaction (PCR)-based nucleic acid detection, and antigen/antibody immunological assays, exhibit critical limitations including lengthy detection cycles, suboptimal sensitivity, and a priori requirement of pathogen classification knowledge [56] [10]. Notably, it has been reported that nearly 60% of patients with fatal LRIs lacked a definitive etiological diagnosis at the time of death [56].
Metagenomic next-generation sequencing (mNGS) has emerged as a transformative diagnostic tool that overcomes these technical limitations. This culture-independent, hypothesis-free approach enables simultaneous detection of a broad array of pathogens directly from clinical specimens such as bronchoalveolar lavage fluid (BALF) [10]. By providing rapid, comprehensive pathogen identification and antimicrobial resistance (AMR) gene detection, mNGS offers robust technical support for precision anti-infective therapy and represents a crucial methodology within the broader context of metagenomic sequencing for bacterial identification research [56] [10].
This case study examines the clinical application and technical implementation of metagenomic sequencing for pathogen identification in LRTIs using BALF samples, with particular focus on performance comparisons with conventional methods, detailed experimental protocols, and emerging innovations in the field.
Comparative Performance of Pathogen Detection Methods
Diagnostic Performance: mNGS vs. Conventional Methods
Multiple clinical studies have demonstrated the superior sensitivity of metagenomic sequencing approaches compared to conventional microbiological tests (CMTs). A 2025 retrospective study of 400 patients with suspected LRTIs found that mNGS of BALF samples significantly outperformed culture methods, with sensitivity of 93.3% versus 55.6% when compared against final clinical diagnosis as the reference standard [55]. The area under the receiver-operating curve (AUC) of mNGS was 0.744 (95% CI: 0.67-0.82), significantly higher than that of cultures at 0.636 (95% CI: 0.57-0.71) [55].
Another 2025 study evaluating Nanopore targeted sequencing (NTS) in 70 suspected LRTI patients reported similar findings, with NTS showing higher complete (73.21% vs. 16.07%) and partial (23.21% vs. 35.71%) diagnostic rates than CMTs [56]. Diagnostic metrics favored NTS across multiple parameters: sensitivity (96.43% vs. 69.64%), negative predictive value (75.00% vs. 32.00%), Youden index (0.464 vs. 0.363), and AUC (0.732 vs. 0.682) [56].
Table 1: Comparative Diagnostic Performance of Sequencing Methods vs. Conventional Microbiology
| Diagnostic Metric | mNGS (n=400) | Culture (n=400) | NTS (n=70) | CMTs (n=70) |
|---|---|---|---|---|
| Sensitivity | 93.3% | 55.6% | 96.43% | 69.64% |
| Specificity | 54.9% | 71.8% | 50.00% | 66.67% |
| Positive Predictive Value | - | - | 90.00% | 90.70% |
| Negative Predictive Value | 63.9% | 25.9% | 75.00% | 32.00% |
| Area Under Curve (AUC) | 0.744 | 0.636 | 0.732 | 0.682 |
Pathogen Spectrum and Detection Rates
Metagenomic sequencing demonstrates particular advantages in detecting intracellular, fastidious, and mixed pathogens that often evade conventional methods. In a study of 329 patients with confirmed LRTIs, mNGS detected significantly more Streptococcus pneumoniae (7.0% vs. 0%), Haemophilus influenzae (6.7% vs. 0%), Aspergillus (9.4% vs. 3.5%), and Pneumocystis jirovecii (11.9% vs. 0%) compared to culture [55]. A separate analysis of 160 LRTI patients identified Pseudomonas aeruginosa, Corynebacterium striatum, Klebsiella pneumoniae, Candida, and human herpesvirus as the most prevalent pathogens, with distinct seasonal distribution patterns observed for certain bacteria and viruses [54].
The comprehensive detection capability of mNGS is further evidenced by a study of 43 LRTI patients (including 34 COVID-19 cases), where mNGS demonstrated superior sensitivity (95.35% vs. 81.08%) and broader pathogen coverage compared to traditional culture, identifying 36.36% of bacteria and 74.07% of fungi detected by cultures [27]. This enhanced detection range is particularly valuable for identifying co-infections, which were prevalent across multiple studies, with bacterial-viral co-infections being especially common [54].
Table 2: Pathogen Detection Rates by Sequencing vs. Conventional Methods
| Pathogen Category | Specific Pathogens | mNGS/NTS Detection Rate | Conventional Method Detection Rate |
|---|---|---|---|
| Bacteria | Streptococcus pneumoniae | 7.0% | 0% |
| Haemophilus influenzae | 6.7% | 0% | |
| Klebsiella pneumoniae | High prevalence | Lower detection | |
| Fungi | Aspergillus species | 9.4% | 3.5% |
| Pneumocystis jirovecii | 11.9% | 0% | |
| Candida species | High prevalence | Lower detection | |
| Viruses | Human herpesvirus | High prevalence | Lower detection |
| Epstein-Barr virus | Seasonal variation observed | Limited detection |
Metagenomic Sequencing Methodologies
Sample Collection and Processing
Proper sample collection and processing are critical for successful metagenomic sequencing. For BALF samples, collection should follow standardized bronchoscopy procedures. Key considerations include:
- Sample Source: BALF should be collected from the lesion sites identified by chest CT imaging, with samples sourced from the middle segment while discarding the anterior segment's collected liquid [57].
- Sample Volume: Recommended volumes are 5-10 mL for BALF and 4 mL for sputum samples [57].
- Transport Conditions: Samples should be transported to the designated laboratory at ≤ -20°C within 24 hours to maintain sample integrity [57].
- Quality Assessment: Sputum samples should be assessed using the Bartlett grading system, with only samples having a Bartlett score of ≤1 (indicating ≤10 squamous epithelial cells per low-power field and ≥25 leukocytes per low-power field) being included for analysis to minimize oropharyngeal contamination [27].
For sample processing, mechanical disruption through bead-beating has proven effective. One protocol recommends transferring 1.2 mL of vortex-mixed BALF to a tube containing heterogeneously sized glass beads, followed by mechanical disruption at 30 Hz for 10 minutes [55]. After centrifugation (12,000 rpm, 3 minutes), the supernatant is collected for nucleic acid extraction.
Nucleic Acid Extraction and Library Preparation
Effective nucleic acid extraction is essential for obtaining high-quality genetic material for sequencing. The TIANamp Micro DNA Kit (TIANGEN Biotech, Beijing, China) has been successfully employed for DNA extraction from BALF samples [55]. For comprehensive pathogen detection, including RNA viruses, dual DNA/RNA extraction should be considered.
Library construction approaches vary by sequencing platform:
- Illumina Platforms: Libraries can be constructed using the Nextera XT kit, with quality control performed using Qubit and Agilent 2100 Bioanalyzer systems [55].
- Nanopore Targeted Sequencing (NTS): This approach combines metagenomic sequencing (unbiased screening of all microbial nucleic acids) with targeted sequencing (enrichment of clinically high-risk or difficult-to-lyse pathogens) [56]. The technical strategy utilizes the Oxford Nanopore platform in combination with specific transducer proteins like α-hemolysin, where double-stranded DNA is unwound and passes through nanopores under an applied voltage, causing specific ion current changes that are captured and converted to base sequences by machine learning algorithms [56].
Bioinformatics Analysis Pipeline
The bioinformatics workflow for mNGS data analysis typically includes:
- Quality Control and Adapter Trimming: Tools like fastp (v0.19.5) and Komplexity (v0.3.62) filter adapter contamination, low-quality, and low-complexity reads [55].
- Host DNA Depletion: Human host DNA reads mapping to the human reference assembly GRCh38 are removed with Bowtie2 (v2.3.4.3) to enhance microbial signal detection [55].
- Taxonomic Classification: Residual sequencing data are mapped to microbial genome databases using various algorithms. Tools like Kraken2, MetaPhlAn, and Centrifuge utilize k-mer based alignment strategies for taxonomic classification [4].
- Result Interpretation: Microorganisms are classified as potential pathogens based on normalized read counts and estimated microbial concentration. One reporting framework categorizes pathogens as:
- Class A: Specific pathogenic pathogens or clinically common pathogenic pathogens in respiratory specimens
- Class B: Opportunistic pathogens in patients with immune deficiency/damage
- Class C: Normal respiratory microbiota that generally doesn't cause infection [57]
Sequencing Workflow: Sample to Clinical Report
Research Reagent Solutions and Experimental Tools
Successful implementation of metagenomic sequencing for LRTI pathogen identification requires specific reagents, kits, and computational tools. The following table details essential components for establishing a robust mNGS workflow.
Table 3: Essential Research Reagents and Tools for Metagenomic Sequencing
| Category | Specific Product/Platform | Application/Function | Reference |
|---|---|---|---|
| Nucleic Acid Extraction | TIANamp Micro DNA Kit (TIANGEN Biotech) | DNA extraction from BALF samples | [55] |
| Library Preparation | Nextera XT Kit (Illumina) | Library construction for Illumina platforms | [55] |
| Sequencing Platforms | Oxford Nanopore Technologies | Long-read, real-time sequencing | [56] [10] |
| Illumina NextSeq-550Dx | Short-read, high-throughput sequencing | [55] | |
| Bioinformatics Tools | fastp (v0.19.5) | Quality control and adapter trimming | [55] |
| Bowtie2 (v2.3.4.3) | Host DNA depletion | [55] | |
| Kraken2, MetaPhlAn | Taxonomic classification | [4] | |
| Sample Processing | Bead-beating system with glass beads | Mechanical disruption of microbial cells | [55] |
Advanced Applications and Innovations
Antimicrobial Resistance Gene Detection
Beyond pathogen identification, metagenomic sequencing provides valuable capabilities for detecting antimicrobial resistance (AMR) genes. In a study of 70 LRTI patients, NTS detected 16 resistance genes in 15 patients, with high coverage of ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) [56]. This functionality enables not only pathogen identification but also simultaneous analysis of antimicrobial resistance profiles, significantly enhancing treatment guidance.
The ability of mNGS to detect plasmid-mediated resistance genes—such as mcr-1 and blaNDM-5—that often go undetected by routine phenotypic methods represents a significant advancement in resistance monitoring [10]. This capability is particularly valuable for tracking the spread of resistance mechanisms and informing public health interventions.
Artificial Intelligence-Enhanced Pathogen Identification
Recent innovations integrate artificial intelligence (AI) with metagenomic sequencing to address interpretation challenges. AI-assisted architectures enhance accuracy, scalability, and biological interpretability through several core innovations:
- Structured Probabilistic Modeling: Formulates pathogen detection as a hierarchical and compositional inference task under taxonomic and ecological constraints, integrating phylogenetic priors and sparsity-aware mechanisms to reduce noise and ambiguity [4].
- Taxon-aware Compositional Inference Network (TCINet): A deep learning model that processes sequencing reads to produce taxonomic embeddings, estimates abundance distributions via masked neural activations, and propagates uncertainty through log-normal variance modeling [4].
- Hierarchical Taxonomic Reasoning Strategy (HTRS): A post-inference module that refines predictions by enforcing compositional constraints, propagating evidence across taxonomic hierarchies, and calibrating confidence using entropy and variance-based metrics [4].
These AI-enhanced approaches are particularly valuable for distinguishing true pathogens from background microbiota in complex respiratory samples, addressing a key challenge in mNGS implementation.
AI-Enhanced Analysis Workflow
Impact on Antimicrobial Stewardship
The diagnostic advantages of metagenomic sequencing translate directly to improved antimicrobial stewardship. In a study of 329 LRTI patients, antibiotic treatment was modified based on mNGS results in more than half of the cases (50.5%, 166/329), including 20 cases with adjusted antimicrobial regimens, 70 cases with de-escalated empirical antibiotic treatment, and 76 patients with escalated treatment by increasing dosage or medication [55]. Importantly, 60.8% (101/166) of patients responded to these modified antibiotic treatments, demonstrating the clinical utility of mNGS-guided therapy [55].
Another study focusing on grassroots hospitals found that early use of targeted NGS (t-NGS) reduced the antibiotic replacement rate in elderly patients after 3 days of admission, highlighting the role of rapid sequencing technologies in optimizing antibacterial drug management strategies, particularly in resource-limited settings [57].
Metagenomic sequencing represents a paradigm shift in the diagnosis and management of lower respiratory tract infections. The technology's ability to provide rapid, comprehensive pathogen identification directly from BALF samples addresses critical limitations of conventional microbiological methods, particularly for fastidious, intracellular, and mixed pathogens. The integration of antimicrobial resistance gene detection and emerging AI-enhanced analytical frameworks further expands the clinical utility of this approach.
While challenges remain in standardization, interpretation, and cost-effectiveness, the demonstrated impact on antimicrobial stewardship and patient outcomes underscores the transformative potential of metagenomic sequencing in respiratory infection diagnostics. As sequencing technologies continue to evolve and become more accessible, their role in precision medicine for infectious diseases is poised to expand, ultimately enhancing our ability to combat the global burden of lower respiratory tract infections.
Antimicrobial resistance (AMR) represents a formidable global health crisis, projected to cause 10 million deaths annually by 2050 if unaddressed [58]. The concept of the resistome has fundamentally reshaped our understanding of AMR, encompassing all antibiotic resistance genes (ARGs) in a given environment, including those intrinsic to bacterial genomes, acquired via horizontal gene transfer (HGT), and cryptic determinants with potential to evolve into active resistance mechanisms [58]. Unlike traditional clinical microbiology which focuses on isolated pathogens, metagenomics enables the comprehensive study of resistomes directly from environmental, animal, and human samples without requiring cultivation [59] [60]. This approach has revealed that ARGs predate clinical antibiotic use by millions of years, having evolved in environmental bacteria as survival tools against naturally produced antimicrobial compounds [58]. The One Health framework acknowledges that AMR dynamics span human, animal, and environmental ecosystems, necessitating integrated surveillance strategies [59] [61].
Metagenomic analysis of AMR moves beyond simple identification of resistance genes to profile their abundance, diversity, and mobility potential within microbial communities. This is particularly crucial because environmental reservoirs serve as silent incubators of resistance genes, with horizontal gene transfer and stress-induced mutagenesis fueling their evolution and dissemination into human pathogens [58]. The power of metagenomics lies in its ability to capture the full genetic content of complex microbial communities, including unculturable organisms that may represent significant reservoirs of novel resistance mechanisms [60] [61]. This in-depth profiling provides researchers and drug development professionals with critical insights into emerging resistance trends, transmission pathways, and potential targets for novel therapeutic interventions.
Molecular Mechanisms of Antimicrobial Resistance
A comprehensive understanding of AMR mechanisms is essential for effective metagenomic profiling. Bacteria employ diverse molecular strategies to circumvent antibiotic action, which can be categorized into several major classes.
Table 1: Fundamental Mechanisms of Antimicrobial Resistance
| Resistance Mechanism | Molecular Basis | Example Genes | Effect on Antibiotic |
|---|---|---|---|
| Enzymatic Inactivation | Antibiotic modification or destruction through enzyme activity | β-lactamases (bla), aminoglycoside-modifying enzymes | Direct cleavage or chemical modification of antibiotic structure |
| Target Modification | Alteration of antibiotic binding sites through mutation or enzymatic alteration | mecA, gyrA, parC | Reduced antibiotic affinity to cellular targets |
| Efflux Systems | Overexpression of membrane transporters that export antibiotics | RND family efflux pumps (mexB, acrB) | Reduced intracellular antibiotic accumulation |
| Reduced Permeability | Modification of cell wall/membrane structure to limit antibiotic entry | Porin mutations, membrane lipid modifications | Decreased antibiotic uptake into bacterial cell |
| Bypass Pathways | Activation of alternative metabolic pathways that circumvent antibiotic targets | Alternative peptidoglycan synthesis enzymes | Development of resistance without direct target modification |
At the molecular level, resistance is driven by chromosomal mutations, enzymatic drug inactivation, efflux pump overexpression, target modification, and horizontal gene transfer (HGT) [58]. The mobilization of resistance genes via mobile genetic elements (MGEs) represents a particularly critical aspect of AMR dissemination. Plasmids, integrons, transposons, and integrative conjugative elements (ICEs) serve as vehicles for ARG transfer between bacterial species, including between commensal and pathogenic microbes [58] [60]. Recent studies using structural biology techniques have elucidated how resistance enzymes like β-lactamases and carbapenemases adapt their catalytic sites, allowing even subtle amino acid substitutions to expand their substrate profiles [58]. The discovery of mobilized colistin resistance (MCR) proteins on self-transmissible plasmids underscores the role of horizontal transfer in the global spread of even last-resort antibiotics like colistin [58].
Environmental conditions significantly influence these molecular dynamics. Sub-inhibitory antibiotic concentrations, commonly found in wastewater treatment plants, agricultural soils, and aquaculture ponds, activate bacterial SOS responses that accelerate mutagenesis and prophage induction, thereby enhancing ARG mobilization [58]. Integrons serve as natural gene capture and expression systems, facilitating the dissemination of ARGs through cassette insertion and rearrangement [58]. Understanding these mechanisms informs the strategic development of metagenomic profiling approaches that can capture not only the presence of ARGs but also their genetic context and mobilization potential.
Metagenomic Workflow for AMR Profiling
The complete metagenomic workflow for AMR profiling encompasses multiple stages from sample collection to biological interpretation, each with critical considerations for ensuring data quality and relevance.
Sample Collection and Processing
Sample processing represents a foundational step that significantly impacts downstream analysis. For water samples (e.g., from urban lakes, wastewater treatment plants), filtration through 0.22μm membranes effectively captures microbial biomass [62]. For complex solid matrices (e.g., soil, sediment), mechanical disruption through bead beating improves cell lysis efficiency. The DNeasy PowerWater Kit (QIAGEN) and DNeasy PowerSoil Kit have demonstrated efficacy in environmental metagenomic studies [62]. DNA concentration and purity should be assessed using fluorometric methods (e.g., Qubit fluorometer) rather than spectrophotometry, which is sensitive to contaminants [62]. The quality of extracted DNA must be rigorously controlled, as inhibitors co-extracted from complex matrices can severely compromise library preparation and sequencing efficiency.
Sequencing Strategies and Considerations
Two primary sequencing approaches are employed in AMR metagenomics: short-read (Illumina) and long-read (Oxford Nanopore, PacBio) technologies. Short-read platforms offer high accuracy and throughput at lower cost, making them suitable for ARG annotation and abundance quantification [61]. Long-read technologies facilitate complete genome assemblies, precise plasmid reconstruction, and structural variation analysis, providing crucial information about ARG genomic context [61]. For comprehensive AMR profiling, a hybrid approach combining both technologies often yields optimal results. Sequencing depth requirements vary by application: ≥100× coverage is needed for precise SNP detection and plasmid tracking, while 30-50× coverage may suffice for broader resistome characterization [61].
Table 2: Bioinformatics Tools for AMR Metagenomics Analysis
| Analysis Type | Tool Options | Primary Function | Database Dependencies |
|---|---|---|---|
| Quality Control & Preprocessing | FASTP, Trimmomatic | Adapter removal, quality filtering, read trimming | - |
| Assembly | MEGAHIT, metaSPAdes | De novo assembly of contigs from metagenomic reads | - |
| ORF Prediction | Prodigal, MetaGeneMark | Identification of protein-coding sequences | - |
| ARG Annotation | DeepARG, ARGs-OAP, AMR++ | Resistance gene identification and classification | CARD, ARDB, DeepARG-DB |
| MGE Annotation | mobileOG-db, PlasmidFinder | Identification of mobile genetic elements | MobileElementDB, ACLAME |
| Taxonomic Profiling | MetaPhlAn, Kraken2 | Microbial community composition analysis | Custom genome databases |
| Binning & MAG Generation | MetaBAT2, MaxBin2 | Reconstruction of metagenome-assembled genomes | - |
| Visualization & Statistics | R packages (ggplot2, phyloseq), ITOL | Data visualization, statistical analysis | - |
Bioinformatics Analysis Pipeline
The bioinformatics workflow for AMR profiling involves multiple steps that transform raw sequencing data into biologically meaningful information. After quality control (e.g., using FASTP) [62], reads are assembled into contigs using tools like MEGAHIT [62]. Open reading frame (ORF) prediction is performed with Prodigal [62], followed by creation of a non-redundant gene catalog using CD-HIT (98% identity, 90% coverage) [62]. For functional annotation, DIAMOND with an E-value cutoff of ≤1e-5 provides efficient alignment against reference databases [62]. ARG annotation can be performed using DeepARG [62] or similar tools against specialized databases. To enable cross-sample comparisons, gene abundance should be normalized to transcripts per million (TPM) or similar metrics that account for variations in sequencing depth and gene length [62].
For more comprehensive analysis, binning procedures using pipelines like MetaWRAP facilitate the reconstruction of metagenome-assembled genomes (MAGs) [62]. Binning tools such as MetaBAT2 group contigs into putative genomes based on sequence composition and abundance patterns [62]. Quality assessment with CheckM ensures only bins meeting thresholds (>50% completeness, <10% contamination) are retained for downstream analysis . Taxonomic classification of MAGs can be performed using GTDB-Tk, which leverages the Genome Taxonomy Database [62]. Functional annotation of MAGs against databases like KEGG, COG, and pathogen-host interaction (PHI) databases provides insights into metabolic potential and virulence traits [62].
Figure 1: Comprehensive Workflow for Metagenomic AMR Profiling. The diagram illustrates the integrated process from sample collection through bioinformatics analysis to resistome interpretation, highlighting critical quality control checkpoints (green boxes) and specialized analyses like MAG reconstruction and mobile element tracking.
Critical Analysis Components for AMR Profiling
ARG Annotation and Abundance Quantification
Accurate ARG annotation requires specialized databases and tools. The DeepARG tool utilizes a deep learning framework to identify ARGs with high precision, leveraging the DeepARG-DB [62]. Alternative approaches include alignment-based methods against the Comprehensive Antibiotic Resistance Database (CARD) or ARDB. For abundance quantification, normalization is essential for cross-sample comparisons. The transcripts per million (TPM) metric effectively normalizes for variations in sequencing depth and gene length [62]. This involves calculating reads per kilobase per million reads mapped (RPKM) for each gene followed by scaling to one million. Statistical analysis such as Analysis of Variance (ANOVA) can then assess significance of differences in mean gene abundance among sample groups [62]. Principal Coordinate Analysis (PCoA) implemented with R packages (e.g., 'vegan', 'amplicon') enables visualization of β-diversity patterns based on ARG profiles [62].
Mobile Genetic Elements and Horizontal Gene Transfer
Analyzing MGEs is crucial for understanding ARG dissemination potential. Plasmids represent the most critical vehicles for ARG dissemination, often carrying multiple resistance genes simultaneously [58]. Integrons serve as natural gene capture systems, facilitating the dissemination of ARGs through cassette insertion and rearrangement [58]. Transposons and insertion sequences further mobilize ARGs across bacterial species. Bioinformatic tools like mobileOG-db can identify MGEs in metagenomic data [62]. The co-localization of ARGs with MGEs significantly increases transmission risk, which can be quantified using frameworks like MetaCompare to estimate resistome risk by evaluating the coexistence of ARGs, MGEs, and human pathogens [62].
Taxonomic Profiling and Host Assignment
Linking ARGs to their bacterial hosts represents a significant challenge and opportunity in metagenomic AMR profiling. Two primary approaches exist: read-based taxonomic assignment without assembly (faster but lower resolution) and contig-based assignment after assembly (more computationally intensive but higher accuracy) [60]. For contig-based approaches, tools like Kraken2 or MetaPhlAn provide taxonomic classification. The reconstruction of metagenome-assembled genomes (MAGs) through binning enables more precise host assignment, allowing researchers to determine which specific bacterial taxa harbor particular resistance determinants [62]. This is particularly valuable for identifying pathogenic hosts of concern. Taxonomic assignment also facilitates analysis of microbial community composition, which can be correlated with environmental parameters and ARG abundance [60].
Advanced Applications and Integration
One Health Surveillance Framework
The One Health approach integrates genomic surveillance across human, animal, and environmental compartments to comprehensively track AMR transmission [61]. This framework recognizes that resistance genes circulate between clinical settings, agriculture, wastewater, and natural environments [58] [61]. Implementing this approach requires standardized methodologies across sectors, including consistent DNA extraction protocols, sequencing platforms, and bioinformatics pipelines [61]. The integration of whole-genome sequencing (WGS) of bacterial isolates with shotgun metagenomics of complex samples creates a powerful surveillance system that combines high-resolution pathogen data with community-level resistome profiling [61]. Global initiatives like the WHO's GLASS (Global Antimicrobial Resistance and Use Surveillance System) aim to incorporate One Health data to inform strategies at all levels [59].
Resistance Risk Assessment
Beyond cataloging ARGs, metagenomic data enables risk assessment of resistomes. The MetaCompare tool estimates resistome risk by evaluating the coexistence of ARGs, MGEs, and human pathogens [62]. Statistical approaches like Spearman rank correlation analysis can examine associations between environmental factors and resistance genes [62]. Univariate linear regression further models relationships between functional genes and resistance risk [62]. For example, a 2025 study of urban lakes found that eutrophication enhanced certain vitamin B12 synthesis pathways while increasing abundance of metal resistance genes, demonstrating unexpected linkages between metabolic processes and resistance profiles [62]. Such integrated analysis provides valuable insights for risk prioritization and intervention strategies.
Figure 2: AMR Gene Dynamics and Transfer Mechanisms. This diagram illustrates the complex interplay between resistance mechanisms, genetic elements, and environmental factors that drive the development and dissemination of antimicrobial resistance in microbial communities.
Research Reagent Solutions for Metagenomic AMR Studies
Table 3: Essential Research Reagents and Tools for Metagenomic AMR Profiling
| Category | Specific Product/Kit | Application in Workflow | Key Features |
|---|---|---|---|
| DNA Extraction | DNeasy PowerWater Kit (QIAGEN) | DNA isolation from water samples | Effective for low-biomass samples, inhibitor removal |
| DNA Extraction | DNeasy PowerSoil Kit (QIAGEN) | DNA isolation from complex matrices | Mechanical lysis for difficult-to-lyse organisms |
| Quality Control | Qubit Fluorometer (Thermo Fisher) | DNA/RNA quantification | Fluorometric specificity for nucleic acids |
| Library Preparation | Illumina DNA Prep Kits | Library construction for Illumina sequencing | Streamlined workflow, high complexity libraries |
| Sequencing | Illumina HiSeq/NovaSeq | Short-read sequencing | High accuracy, high throughput for ARG profiling |
| Sequencing | Oxford Nanopore MinION | Long-read sequencing | Real-time data, long reads for assembly |
| Functional Annotation | DIAMOND | BLAST-like alignment tool | Ultra-fast for large metagenomic datasets |
| ARG Database | DeepARG-DB | Resistance gene reference | Comprehensive ARG collection with deep learning models |
| MGE Database | mobileOG-db | Mobile genetic element reference | Curated database of MGE proteins |
| VB12 Pathway | VB12Path Database | Vitamin B12 synthesis genes | Specialized database for cobalamin biosynthesis |
Metagenomic approaches for profiling antimicrobial resistance genes have revolutionized our ability to monitor and understand the complex dynamics of resistomes across diverse ecosystems. By moving beyond simple identification to comprehensive characterization of ARG abundance, mobility potential, and host associations, researchers can generate critical insights into AMR transmission pathways and emerging threats. The integration of metagenomic data within a One Health framework provides a powerful surveillance approach that spans clinical, agricultural, and environmental compartments [61].
Future directions in this field include the development of standardized protocols and bioinformatics pipelines to enhance data comparability across studies and regions [61]. The growing application of machine learning and artificial intelligence approaches promises to improve ARG prediction, risk assessment, and even anticipation of novel resistance mechanisms [58] [59]. Additionally, the integration of metatranscriptomics and metaproteomics could provide insights into which resistance genes are actively expressed and functioning in complex microbial communities. As sequencing technologies continue to advance and costs decrease, metagenomic AMR profiling will likely become an increasingly routine component of global antimicrobial resistance surveillance and management strategies, ultimately contributing to more targeted interventions and preservation of antimicrobial efficacy for future generations.
Navigating Technical Challenges: Strategies for Enhanced mNGS Sensitivity and Specificity
Metagenomic next-generation sequencing (mNGS) has revolutionized microbial diagnostics and microbiome research by enabling unbiased detection of pathogens and functional characterization of complex communities. However, a significant challenge in analyzing host-derived samples is the overwhelming abundance of host DNA, which can constitute over 95% of sequenced material in respiratory samples, 99.7% in bronchoalveolar lavage fluid (BALF), and similar proportions in other sample types [63] [64]. This high host background reduces microbial sequencing depth, diminishes detection sensitivity for low-abundance pathogens, and increases sequencing costs, ultimately limiting the clinical utility and research applications of mNGS technologies.
Host DNA depletion methods have emerged as essential solutions to overcome these limitations, employing mechanical, enzymatic, and chemical approaches to selectively remove host DNA while preserving microbial genetic material. The effectiveness of these methods varies considerably across sample types, microbial communities, and specific clinical contexts. This technical guide provides a comprehensive overview of current host depletion methodologies, their performance characteristics, experimental protocols, and implementation considerations for researchers and clinicians working in bacterial identification research.
Classification of Host Depletion Strategies
Host DNA depletion methods can be broadly categorized into pre-extraction and post-extraction approaches, each with distinct mechanisms and applications.
Pre-extraction Methods
Pre-extraction methods physically separate or selectively degrade host material before DNA extraction:
Selective host cell lysis utilizes differential susceptibility of host and microbial cells to lysis conditions. Osmotic lysis with pure water or mild detergents disrupts fragile mammalian membranes while resilient microbial walls remain intact [65]. Saponin-based lysis at concentrations ranging from 0.025% to 0.50% effectively lyses human cells in respiratory samples [63].
Enzymatic digestion of exposed DNA follows host cell lysis. Benzonase and DNase degrade liberated host DNA without damaging DNA within intact microbial cells [66].
Physical separation techniques include:
- Microfiltration using pore sizes (e.g., 10μm) that retain host cells while allowing microbial passage [63].
- Differential centrifugation separates cells by size and density through sequential low-speed (host cell pelleting) and high-speed (microbial pelleting) steps [65].
- Novel filtration technologies such as Zwitterionic Interface Ultra-Self-assemble Coating (ZISC)-based filters selectively bind host leukocytes while allowing microbial passage, achieving >99% white blood cell removal [67].
Viability-based approaches employ propidium monoazide (PMA), a DNA intercalator that penetrates compromised host membranes. Photoactivation creates covalent DNA crosslinks, inhibiting amplification [65]. Optimal PMA concentration is typically 10μM [63] [65].
Post-extraction Methods
Post-extraction methods target host DNA after extraction:
Methylation-based depletion exploits differential CpG methylation patterns between host and microbial genomes. Commercial kits like NEBNext Microbiome DNA Enrichment Kit bind and remove methylated host DNA [68] [69].
CRISPR/Cas9 systems target host-specific sequences for degradation, though this approach is not yet widely adopted for whole-genome host depletion [65].
Bioinformatic subtraction computationally identifies and filters host reads post-sequencing using alignment or k-mer based methods [69].
Performance Comparison Across Methods
The effectiveness of host depletion methods varies significantly by sample type, with each method exhibiting unique strengths and limitations.
Table 1: Host Depletion Efficiency Across Respiratory Sample Types
| Method | Mechanism | BALF (Host % →) | Oropharyngeal (Host % →) | Sputum (Host % →) | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Saponin + Nuclease (S_ase) | Selective host lysis + DNA digestion | 99.99% reduction (to 0.01%) [63] | 94.1% → ~34.4% non-host [63] | Effective for CF sputum [66] | High host depletion efficiency | Diminishes some commensals/pathogens |
| Filtration + Nuclease (F_ase) | Size exclusion + DNA digestion | 99.99% reduction (to 0.01%) [63] | - | - | Balanced performance | May miss intracellular microbes |
| HostZERO (K_zym) | Commercial kit (selective lysis) | 99.99% reduction (to 0.01%) [63] | 94.1% → ~38.4% non-host [63] | 99.2% → ~54.5% non-host [64] | High host depletion | Variable bacterial retention |
| QIAamp Microbiome (K_qia) | Commercial kit (selective lysis) | ~98.61% reduction [63] | 94.1% → ~37.0% non-host [63] | - | Good bacterial retention | Moderate host depletion |
| Osmotic Lysis + PMA (lyPMA) | Osmotic lysis + DNA crosslinking | - | 94.1% → ~91.5% non-host [64] | Effective for saliva [65] | Minimal hands-on time, cost-effective | Less effective for some sample types |
| Benzonase Treatment | Hypotonic lysis + nuclease digestion | - | - | Effective for CF sputum [66] | Targets extracellular DNA | Requires fresh sample processing |
| MolYsis Basic | Chaotropic lysis + nuclease | ~98.23% reduction in BALF [64] | - | 99.2% → ~29.6% non-host [64] | Effective for high-host samples | Potential Gram-positive bias |
| NEBNext Microbiome | Methylation-based depletion | Poor performance [63] | Ineffective [63] | - | Post-extraction application | Bias against AT-rich microbes |
Table 2: Impact on Microbial Read Recovery and Diversity
| Method | Fold-Increase Microbial Reads (BALF) | Fold-Increase Microbial Reads (OP) | Effect on Species Richness | Effect on Functional Profiling |
|---|---|---|---|---|
| Saponin + Nuclease (S_ase) | 55.8-fold [63] | 5.9-fold [63] | Increased | Enhanced gene coverage |
| HostZERO (K_zym) | 100.3-fold [63] | - | Significantly increased [64] | Improved functional characterization |
| QIAamp Microbiome (K_qia) | 55.3-fold [63] | 4.2-fold [63] | Increased | Improved antibiotic resistance detection |
| Filtration + Nuclease (F_ase) | 65.6-fold [63] | - | - | Balanced improvement |
| Osmotic Lysis + PMA (lyPMA) | - | - | Moderate increase | Moderate improvement |
| MolYsis Basic | - | - | Significantly increased in BALF [64] | Enhanced functional profiling |
| Benzonase Treatment | - | - | Increased | Improved antibiotic resistance gene detection [66] |
Sample Type-Specific Considerations
Respiratory samples present unique challenges due to variability in host content and microbial biomass. BALF contains extremely high host DNA (median 99.7%) with low bacterial loads (median 1.28 ng/mL) [63]. Saponin-based lysis with nuclease digestion and HostZERO methods show particularly strong performance for these samples [63] [70]. For sputum samples from cystic fibrosis patients, benzonase-based approaches effectively reduce extracellular DNA from biofilms and dead cells [66].
Blood samples require specialized approaches due to low microbial biomass. The novel ZISC-based filtration system achieves >99% white blood cell removal while preserving bacteria and viruses, increasing microbial reads tenfold in sepsis samples [67]. Genomic DNA-based mNGS with host depletion outperforms cell-free DNA approaches, detecting 100% of expected pathogens in clinical validation [67].
Urine samples, particularly from healthy individuals, represent low-biomass environments where host depletion significantly improves metagenome-assembled genome (MAG) recovery. The QIAamp DNA Microbiome Kit maximizes microbial diversity while effectively depleting host DNA in urine [71].
Saliva samples with ~90% host DNA benefit from osmotic lysis with PMA treatment, reducing host reads to 8.53% while minimizing taxonomic bias [65].
Detailed Experimental Protocols
Saponin-Based Host Depletion for Respiratory Samples
This protocol, optimized for BALF and oropharyngeal samples, achieves >99.99% host DNA depletion [63]:
Reagents and Equipment:
- Saponin stock solution (0.025-0.50% in PBS)
- DNase I or Benzonase endonuclease
- DNA digestion buffer (Tris-HCl, MgCl₂, CaCl₂)
- Microcentrifuge and refrigerated centrifuge
- DNA extraction kit (standard phenyl:chloroform or commercial kits)
Procedure:
- Sample Preparation: Homogenize 200-500μL of respiratory sample (BALF or swab suspension) by vortexing.
- Host Cell Lysis: Add saponin to a final concentration of 0.025%. Mix thoroughly and incubate at room temperature for 10 minutes.
- Enzymatic Digestion: Add DNase I (5U/μL) or Benzonase (25U/μL) in appropriate buffer. Incubate at 37°C for 30 minutes.
- Enzyme Inactivation: Add EDTA to 5mM final concentration and heat at 75°C for 10 minutes.
- Microbial Pellet Recovery: Centrifuge at 10,000×g for 10 minutes at 4°C. Discard supernatant.
- DNA Extraction: Proceed with standard DNA extraction on the pellet.
Optimization Notes:
- Saponin concentration optimization is critical—higher concentrations may damage certain microbial cells [63].
- For samples with high extracellular DNA (68.97% in BALF, 79.60% in OP), combine with propidium monoazide (PMA) treatment to crosslink free DNA [63].
Osmotic Lysis with PMA (lyPMA) for Saliva and Respiratory Samples
This cost-effective method requires minimal hands-on time and effectively depletes extracellular host DNA [65]:
Reagents and Equipment:
- Molecular grade water
- Propidium monoazide (PMA) stock solution (1-2mM in water)
- Light source (LED lamp or halogen light)
- Microcentrifuge and vortex mixer
Procedure:
- Sample Preparation: Aliquot 200μL of sample into a light-transparent tube.
- Osmotic Lysis: Add 400μL molecular grade water. Vortex briefly and incubate at room temperature for 5 minutes.
- PMA Treatment: Add PMA to final concentration of 10μM. Mix thoroughly and incubate in dark for 10 minutes.
- Photoactivation: Place tubes on ice and expose to bright light source for 15 minutes.
- Microbial Recovery: Centrifuge at 10,000×g for 10 minutes. Discard supernatant.
- DNA Extraction: Proceed with standard DNA extraction on pellet.
Optimization Notes:
- PMA concentration should be optimized for specific sample types—10μM works for most saliva samples [65].
- The method is particularly effective for samples with high extracellular DNA content.
Benzonase-Based Extracellular DNA Depletion for Sputum
This protocol specifically targets extracellular DNA in complex, polymicrobial samples like cystic fibrosis sputum [66]:
Reagents and Equipment:
- Hypotonic lysis buffer (10mM Tris-HCl, 1mM EDTA, pH 8.0)
- Benzonase endonuclease (≥250U/μL)
- MgCl₂ stock solution (25mM)
- Water bath or thermal mixer
- Refrigerated centrifuge
Procedure:
- Sample Homogenization: Mix sputum sample with equal volume of Sputasol or dithiothreitol (DTT) solution. Incubate at room temperature for 15 minutes with occasional vortexing.
- Hypotonic Lysis: Add 2 volumes of hypotonic lysis buffer. Incubate on ice for 10 minutes.
- Benzonase Digestion: Add MgCl₂ to 2mM final concentration and Benzonase to 50U/mL. Mix gently and incubate at 37°C for 45 minutes with occasional mixing.
- Microbial Recovery: Centrifuge at 8,000×g for 15 minutes at 4°C. Discard supernatant.
- Wash Step: Resuspend pellet in PBS and centrifuge again at 10,000×g for 10 minutes.
- DNA Extraction: Proceed with standard DNA extraction.
Application Notes:
- This method increases microbial sequencing depth and improves detection of antibiotic resistance genes [66].
- Particularly valuable for chronic infection samples where extracellular DNA from biofilms and dead cells dominates.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Kits for Host DNA Depletion
| Reagent/Kit | Manufacturer | Mechanism | Optimal Sample Types | Key Considerations |
|---|---|---|---|---|
| HostZERO Microbial DNA Kit | Zymo Research | Selective host cell lysis & DNA digestion | BALF, respiratory samples, urine | Highest host depletion efficiency; variable bacterial retention [63] [71] |
| QIAamp DNA Microbiome Kit | Qiagen | Selective lysis using buffer conditions | Respiratory, urine, diverse samples | Good bacterial retention; moderate host depletion [63] [71] |
| MolYsis Complete5 | Molzym | Chaotropic lysis + nuclease digestion | Sputum, tissue, high-host samples | Effective for high-host content; potential Gram-positive bias [64] [66] |
| NEBNext Microbiome DNA Enrichment Kit | New England Biolabs | Methyl-CpG binding domain depletion | Various (post-extraction) | Bias against AT-rich microbes; poor for respiratory samples [63] [65] |
| Benzonase Nuclease | Sigma-Aldrich/Merck | Degrades extracellular DNA | Sputum, CF samples, high-extracellular DNA | Requires fresh processing; effective for biofilm DNA [66] |
| Propidium Monoazide (PMA) | Biotium/BioVision | Photoactivatable DNA crosslinker | Saliva, urine, fresh samples | Targets compromised cells; requires light exposure [65] |
| Saponin | Various suppliers | Selective host membrane disruption | BALF, respiratory samples | Concentration-critical (0.025-0.50%) [63] |
| ZISC-based Filtration Device | Micronbrane | Zwitterionic interface host binding | Blood, liquid biopsies | >99% WBC removal; preserves microbes [67] |
Technical Considerations and Method Selection
Method-Specific Biases and Limitations
All host depletion methods introduce some degree of taxonomic bias that researchers must consider during experimental design:
Gram-status bias: Methods relying on cell wall integrity may underrepresent Gram-negative bacteria or fragile taxa. Saponin-based treatments can significantly diminish certain commensals and pathogens including Prevotella spp. and Mycoplasma pneumoniae [63]. Commercial kits like MolYsis show potential Gram-positive bias due to differential susceptibility to lysis conditions [66].
Extracellular DNA impact: Samples with high extracellular DNA (68.97% in BALF, 79.60% in OP) require methods that specifically address this fraction [63]. Benzonase treatment and PMA-based approaches effectively target extracellular DNA but may miss intracellular pathogens.
Biomass considerations: Low microbial biomass samples (<1ng/mL) risk complete DNA loss during processing. Methods with minimal wash steps (e.g., lyPMA) preserve biomass but offer moderate depletion efficiency [65].
Integration with Downstream Applications
The choice of host depletion method should align with research objectives:
Genome-centric metagenomics requires high-molecular-weight DNA, favoring gentle mechanical methods like filtration over harsh enzymatic treatments [72].
Antibiotic resistance profiling benefits from methods that increase sequencing depth for functional genes. Benzonase treatment improves detection of antibiotic resistance loci by increasing coverage [66] [70].
Metatranscriptomics requires RNA preservation, limiting options to physical separation methods or specialized commercial kits.
Culture-independent pathogen detection in clinical diagnostics prioritizes methods with proven clinical validation, such as saponin-based depletion for pulmonary tuberculosis diagnosis [70].
Emerging Technologies and Future Directions
Recent advances in host depletion technologies focus on minimizing bias while improving efficiency:
Novel filtration technologies like ZISC-based filters demonstrate >99% host cell removal with preserved microbial composition, showing particular promise for bloodstream infection detection [67].
Combination approaches integrating multiple depletion mechanisms may overcome limitations of individual methods. For example, coupling mechanical separation with enzymatic digestion addresses both cellular and extracellular host DNA [63].
Microfluidics and automated systems enable more reproducible processing while reducing hands-on time and cross-contamination risks.
CRISPR-based depletion methods, though not yet widely implemented, offer potential for sequence-specific host DNA removal with minimal impact on microbial communities [68].
As metagenomic sequencing continues evolving toward clinical diagnostics, standardized host depletion protocols with demonstrated reproducibility across institutions will become increasingly important. Method validation using mock communities and standardized metrics will enable more accurate comparison across studies and eventual regulatory approval for clinical applications.
Effective host DNA depletion is essential for successful metagenomic sequencing of host-derived samples. The optimal method depends on sample type, research objectives, and practical constraints. Mechanical methods like filtration offer minimal taxonomic bias, while enzymatic approaches provide superior depletion efficiency. Commercial kits deliver standardized performance but at higher cost. Researchers must carefully balance these factors when selecting host depletion strategies for bacterial identification research.
As the field advances, integration of multiple depletion mechanisms, development of standardized protocols, and validation across diverse sample types will further enhance the sensitivity and reproducibility of metagenomic sequencing for both research and clinical applications.
Metagenomic next-generation sequencing (mNGS) has emerged as a powerful, hypothesis-free tool for the detection and taxonomic characterization of microorganisms in clinical and environmental samples [73]. This culture-independent approach allows researchers to investigate the vast majority of microorganisms that cannot be readily cultivated in laboratory settings, providing unprecedented insights into microbial community structure and function [74]. However, the accuracy of microbial community surveys based on marker-gene and metagenomic sequencing suffers significantly from the presence of contaminants—DNA sequences not truly present in the sample [75]. These contaminants can originate from various sources, including laboratory reagents, sample collection instruments, laboratory surfaces, air, and even investigators' bodies [75].
The impact of contamination on metagenomic data interpretation is profound and multifaceted. Contamination falsely inflates within-sample diversity, obscures genuine differences between samples, and interferes with meaningful comparisons across studies [75]. The problem is particularly acute in low-biomass environments where the ratio of contaminating DNA to true sample DNA is highest, potentially leading to controversial claims about the presence of bacteria in environments like blood and body tissues [75]. Even in high-biomass environments, contaminants can comprise a significant fraction of low-frequency sequences, limiting reliable resolution of rare variants and contributing to false-positive associations in exploratory analyses [75]. This technical guide provides a comprehensive framework for mitigating contamination and false positives throughout the metagenomic workflow, from initial sample collection to final bioinformatic analysis.
Laboratory Practices for Contamination Prevention
Contamination in metagenomic studies can be categorized into two major types: external contamination and internal (cross-) contamination. External contamination is introduced from outside the samples being measured, with primary sources including laboratory reagents, sample collection instruments, and the laboratory environment [75]. Internal contamination arises when samples mix with each other during sample processing or sequencing [75]. Even minimal contamination can significantly impact results from low-biomass samples, where the amount of endogenous microbial DNA is limited.
The composition of microbial communities themselves presents analytical challenges. Community complexity—a function of species richness (number of species) and evenness (relative abundance distribution)—directly influences the types of analyses that can be performed effectively [74]. Communities with dominant populations (comprising more than a few percent of total cells) enable better assembly and recovery of genomic fragments, while species-rich communities without dominant species may only support analyses of averaged community properties [74].
Pre-Sequencing Quality Control Measures
Implementing rigorous quality control measures during sample preparation is crucial for generating reliable metagenomic data:
- Sample Collection and Handling: Use sterile, DNA-free collection instruments and containers. For samples associated with eukaryotic hosts, consider physical separation methods (e.g., density gradients) to remove host cells or DNA [74].
- DNA Extraction Controls: Include extraction blank controls containing no sample material to monitor contamination introduced during DNA extraction.
- Reagent Quality Assessment: Use high-purity reagents specifically certified for molecular biology applications. Some laboratories employ additional purification methods, such as UV irradiation or enzymatic treatment, to reduce contaminating DNA in reagents [75].
- Laboratory Workflow Separation: Maintain physical separation of pre- and post-amplification areas to prevent cross-contamination with amplified PCR products [75].
- Negative Controls: Process reagent-only negative controls alongside biological samples at both DNA extraction and PCR amplification steps [75].
Control Samples and Their Applications
Including appropriate control samples throughout the experimental workflow is essential for identifying contamination sources:
Table 1: Essential Control Samples for Metagenomic Studies
| Control Type | Composition | Purpose | Interpretation |
|---|---|---|---|
| Extraction Blank | No biological material, only reagents | Identifies contamination from DNA extraction kits and reagents | Any sequences detected likely represent contaminants |
| PCR Blank | PCR-grade water instead of template DNA | Detects contamination from PCR reagents and amplification process | Amplified sequences indicate contamination in amplification reagents |
| Negative Control | Sterile sampling equipment processed like samples | Identifies contamination from collection instruments | Sequences reveal contaminants introduced during sampling |
| Positive Control | DNA from known microbial community | Verifies experimental and sequencing workflow performance | Confirms sensitivity and detection capability |
While these laboratory practices can significantly reduce contamination, they rarely eliminate it completely [75] [73]. Therefore, bioinformatic methods remain essential for comprehensive contamination mitigation.
Bioinformatic Tools for Contamination Identification
Statistical Frameworks for Contaminant Detection
Bioinformatic approaches leverage statistical patterns unique to contaminant sequences to distinguish them from true biological signals. The decontam R package implements two primary classification methods based on widely reproduced signatures of external contamination [75]:
Frequency-based contaminant identification exploits the inverse relationship between contaminant frequency and sample DNA concentration. This method compares two models for each sequence feature: a contaminant model where expected frequency varies inversely with total DNA concentration (slope = -1), and a non-contaminant model where expected frequency is independent of total DNA concentration (slope = 0). The method calculates a score statistic based on the ratio of sum-of-squared residuals between these models, with low scores indicating better fit to the contaminant model [75].
Prevalence-based contaminant identification leverages the higher likelihood of detecting contaminant sequences in negative controls compared to true samples. This approach uses a chi-square test on the presence-absence table of sequence features in true samples versus negative controls, with contaminants showing significantly higher prevalence in negative controls [75].
Specialized Algorithms for False Positive Reduction
Beyond general contaminant detection, specialized algorithms have been developed to address specific types of false positives in metagenomic profiling:
MAP2B (MetAgenomic Profiler based on type IIB restriction sites) addresses false-positive identifications that persist in metagenomic data despite quality filtering. Rather than using universal single-copy markers or whole microbial genomes as references, MAP2B leverages species-specific Type IIB restriction endonuclease digestion sites, which are evenly and abundantly distributed across microbial genomes [76]. This approach avoids common pitfalls like missing markers or multi-alignment of short reads that plague traditional methods.
MAP2B employs a sophisticated false-positive recognition model based on a feature set including genome coverage, sequence count, taxonomic count, and G-score [76]. The genome coverage metric (Ci = Ui/Ei) quantifies the ratio between observed distinct species-specific 2b tags (Ui) and the total number of species-specific 2b tags (Ei) in the reference database, providing a robust uniformity measure that helps distinguish true positives from false positives [76].
Table 2: Comparison of Bioinformatic Tools for Contamination and False Positive Mitigation
| Tool/Method | Approach | Data Requirements | Strengths | Limitations |
|---|---|---|---|---|
| decontam | Statistical classification based on frequency/prevalence patterns | Sample DNA concentration and/or negative control sequences | Identifies study-specific contaminants; easy integration with existing workflows | Not designed for cross-contamination; less effective for very low-biomass samples |
| MAP2B | Type IIB restriction site profiling | Whole metagenome sequencing data | Reduces false positives in species identification; superior precision across sequencing depths | Requires specific reference database construction |
| Relative Abundance Filtering | Removal of sequences below threshold | None beyond abundance data | Simple to implement | Removes rare true sequences; fails to remove abundant contaminants |
| Negative Control Subtraction | Removal of sequences appearing in controls | Sequenced negative controls | Intuitively simple | May remove true sequences that appear in controls due to cross-contamination |
Integrated Workflow for Comprehensive Contamination Control
Effective contamination control requires an integrated approach combining both laboratory and computational methods. The following workflow diagram illustrates a comprehensive strategy for mitigating contamination and false positives throughout the metagenomic analysis pipeline:
Implementing the Integrated Approach
The synergy between laboratory practices and bioinformatic filters creates a robust defense against contamination and false positives:
Design Phase: Plan for appropriate controls (extraction blanks, PCR negatives) during experimental design. Determine sample sizes with consideration for community complexity—simpler communities with dominant species enable more comprehensive genome recovery, while complex communities may only support gene-centric analyses [74].
Wet-Lab Phase: Implement sterile techniques, reagent verification, and workflow separation. For communities containing eukaryotes, consider physical separation methods or alternative approaches like metatranscriptomics to avoid challenges with large eukaryotic genomes [74].
Sequencing Phase: Select appropriate sequencing technology based on research questions. While Illumina platforms dominate metagenomic sequencing, alternative platforms like Oxford Nanopore offer advantages in speed and read length, though with different error profiles [73].
Bioinformatic Phase: Apply quality control, contaminant identification with tools like decontam, and false-positive reduction with methods like MAP2B. For mNGS data, remember that the vast majority of reads (>99%) typically derive from the human host in clinical samples, limiting analytical sensitivity for pathogen detection [73].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Metagenomic Studies
| Reagent/Material | Function | Considerations |
|---|---|---|
| DNA Extraction Kits | Isolation of microbial DNA from samples | Potential source of contamination; verify with extraction blanks |
| PCR Reagents | Amplification of target sequences | Source of contamination; use high-fidelity enzymes for reduced bias |
| Ultrapure Water | Solvent for molecular reactions | Common contamination source; use certified DNA-free grades |
| Type IIB Restriction Enzymes | Digestion for MAP2B profiling | Enable species-specific marker identification [76] |
| DNA Quantitation Standards | Measurement of DNA concentration | Essential for frequency-based contaminant identification [75] |
| Negative Control Materials | Contamination monitoring | Sterile water or buffer processed alongside samples |
| Positive Control Materials | Process verification | Mock communities with known composition |
| Library Preparation Kits | Sequencing library construction | Different kits may introduce varying levels of bias |
Mitigating contamination and false positives in metagenomic sequencing requires a multifaceted approach spanning both laboratory practices and bioinformatic analysis. Laboratory measures including careful experimental design, sterile technique, and comprehensive controls form the first line of defense against contamination. Bioinformatic tools like decontam and MAP2B provide powerful statistical frameworks for identifying and removing contaminant sequences that inevitably persist despite best laboratory practices.
The integration of these approaches throughout the entire metagenomic workflow—from sample collection to data interpretation—enables researchers to generate more accurate profiles of microbial communities. As metagenomic sequencing continues to evolve and find new applications in clinical diagnostics, environmental monitoring, and drug discovery, robust contamination control will remain essential for drawing valid biological conclusions from these powerful but technically challenging datasets.
Within the rapidly advancing field of bacterial metagenomics, the accuracy with which a microbial community can be characterized hinges on the quality of the sequenced library. Metagenomic sequencing captures the vast genetic diversity of microbiomes, providing an detailed characterization of intraspecific diversity essential for investigating bacterial evolution in nature [77]. However, this potential can only be realized with a high-quality sequencing library. Suboptimal library preparation, plagued by issues such as low yield, adapter dimer formation, and amplification bias, can introduce noise that obscures true biological signals, compromises species identification, and leads to false positives in evolutionary analysis [78]. This guide provides an in-depth troubleshooting framework for these three common obstacles, ensuring that your library prep data faithfully represents the original metagenomic sample.
Diagnosing Common Library Preparation Issues
The first step in troubleshooting is accurate diagnosis. Agilent Bioanalyzer or similar electrophoresis systems are indispensable for this, as they provide a visual "fingerprint" of your library's size distribution [79]. The table below summarizes the key characteristics and primary causes of common library issues.
Table 1: Diagnostic Guide to Common Library Preparation Issues
| Issue | Electropherogram Profile | Primary Causes |
|---|---|---|
| Low Library Yield | Low or no peak, or a peak below the required concentration. | • Degraded or low-quality input DNA/RNA [79]. • Inaccurate quantification of input DNA [80]. • Suboptimal amplification cycle number [80]. |
| Adapter Dimer Contamination | A sharp peak at ~70 bp (non-barcoded) or ~90 bp (barcoded) [80]. | • Improper clean-up and size selection post-ligation [80]. • Excess adapters added during ligation [79]. • Degraded starting material leading to excess short fragments [79]. |
| Amplification Bias | Asymmetric, "tailing," or "smearing" peaks; overamplification can also put the sample "above the dynamic range of detection" [80] [79]. | • Excessive PCR cycles during amplification [80] [79]. • High salt concentration in the reaction mix [79]. • Bias introduced in "AMP" cycles, which affects "evenness of coverage" [80]. |
Troubleshooting Low Library Yield
Low library yield can halt sequencing before it begins. The problem often originates from the input material or amplification efficiency.
Experimental Protocol: Optimizing for Low Yield
Verify Input DNA Quality and Quantity:
- Quantification: Use the TaqMan RNase P Detection Reagents Kit or similar probe-based qPCR methods for quantifying amplifiable DNA, as this is more accurate than fluorometry for assessing usability [80].
- Quality Assessment: Run input DNA on a gel or Bioanalyzer to confirm it is intact and not degraded.
Optimize Amplification:
- If using 50-100 ng of input DNA still gives low yield, add 1-3 cycles to the initial target amplification step. It is preferable to add cycles here rather than in a later enrichment PCR to avoid bias [80].
- Avoid over-amplification, as this "will introduce bias toward smaller fragments" [80]. It is better to repeat the amplification with more cycles than to over-amplify and dilute.
Ensure Efficient Purification:
- During bead-based clean-up, "mix the nucleic acid binding beads well before dispensing" [80].
- "Use fresh ethanol" for washes and "pre-wet pipette tips prior to transferring ethanol, as the volume is critical for size selection" [80].
- Thoroughly "remove residual ethanol before elution" to avoid inhibiting downstream reactions [80].
Eliminating Adapter Dimers
Adapter dimers are short fragments composed of ligated adapters that can preferentially cluster on flow cells, drastically reducing the yield of usable sequencing reads [80] [79]. If the short fragment area from adapter dimers exceeds 3% of the total library peak, the library may be rejected [79].
Experimental Protocol: Preventing and Removing Adapter Dimers
Optimize Adapter Ligation:
- Dilute adapters based on the input DNA amount to avoid overloading and prevent leftover, unligated adapters [79].
Perform Rigorous Size Selection:
- An additional clean-up step prior to template preparation is highly recommended to remove adapter dimers [80].
- Adjust the bead-to-sample ratio during SPRI bead clean-up to more stringently exclude short fragments. A higher ratio retains more small fragments, while a lower ratio excludes them more aggressively.
Use High-Quality Input:
- Use fresh, non-degraded samples. "Degraded samples – Fragmented or smeared inputs lead to more short junk," which can ligate to adapters and form dimers [79].
Mitigating Amplification Bias
Over-amplification during PCR can cause bias, skewing representation towards smaller fragments and creating smeared, tailing electropherograms [80] [79]. This bias can distort the apparent abundance of bacterial species in a metagenomic sample.
Experimental Protocol: Minimizing Amplification Artifacts
Minimize PCR Cycles:
- Use the minimum number of PCR cycles necessary to generate sufficient library. "It is better to repeat the amplification reaction to generate sufficient product than to overamplify and dilute" [80].
Optimize Reaction Conditions:
- "Remove residual salt" from previous steps, as high salt concentration can cause tailing and smearing [79].
- Ensure optimal primer concentrations to promote specific amplification and prevent non-specific products [79].
- Use the recommended seals and compression pads for your thermal cycler, and avoid using the outer wells (e.g., Rows A and H) if possible, as they can experience more evaporation [80].
The Scientist's Toolkit: Essential Reagents for Robust Library Prep
The following table details key reagents and their critical functions in ensuring successful library preparation for metagenomic studies.
Table 2: Research Reagent Solutions for Metagenomic Library Preparation
| Reagent / Kit | Function | Technical Notes |
|---|---|---|
| High-Quality Library Prep Kit (e.g., Yeasen 12927/12972 series) | Provides optimized, validated enzymes and buffers for fragmentation, ligation, and amplification to minimize common failure points [79]. | Choose kits designed for your input material (e.g., microbial DNA) and that deliver "smooth, symmetric, high-yield libraries" [79]. |
| Nucleic Acid Binding Beads | Used for post-reaction clean-up and fine size selection to remove unwanted reagents, salts, and short fragments like adapter dimers [80]. | Mix beads well before use. Pre-wet tips when transferring ethanol. Avoid over-drying or under-drying beads during elution [80]. |
| qPCR Quantification Kit (e.g., KAPA qPCR kits) | Selectively quantifies only full-length, amplifiable library fragments that contain both P5 and P7 adapter sequences [81]. | Preferable to fluorometric methods for pooling libraries, as it ignores adapter dimers and incomplete products. Use triplicates and include a standard curve [81]. |
| Fluorometric Assay (e.g., Qubit dsDNA HS Assay) | Selectively quantifies double-stranded DNA (dsDNA) in a sample, providing a more accurate measure of library mass than spectrophotometry [81] [79]. | Risks overestimating functional library concentration as it measures all dsDNA, including primer dimers and incomplete fragments [81]. |
| DNA Size Standard & Gel Matrix | For use with Bioanalyzer, TapeStation, or Fragment Analyzer to accurately determine library fragment size distribution [79]. | Critical for diagnosing adapter dimers, tailing, and broad peaks. Not recommended for quantifying libraries with broad size distributions [81]. |
In bacterial metagenomics, where the research goal is often to accurately identify species and investigate evolution, the integrity of the sequencing library is paramount. Issues of low yield, adapter dimers, and amplification bias are not merely technical inconveniences; they are sources of data distortion that can lead to inaccurate profiling of a microbial community. By adhering to the detailed protocols and best practices outlined here—emphasizing accurate quantification, meticulous size selection, and minimal, optimized amplification—researchers can produce high-fidelity libraries. A robust library preparation workflow ensures that the subsequent sequencing data truly reflects the complex biology of the microbiome, providing a solid foundation for reliable discovery and analysis.
Metagenomic next-generation sequencing (mNGS) has revolutionized microbial ecology and clinical diagnostics by enabling unbiased detection and characterization of bacterial communities directly from complex samples. This powerful technology allows researchers to identify rare, novel, or mixed infections without prior knowledge of the causative agents, providing a significant advantage over traditional culture-based or targeted molecular methods [82]. However, the accuracy and reliability of mNGS analyses are fundamentally dependent on the quality of the reference databases used for taxonomic classification. Unfortunately, these databases often contain systemic taxonomic errors and are vulnerable to sequence contamination, which can severely compromise downstream analyses and lead to erroneous biological conclusions.
Within the context of metagenomic sequencing for bacterial identification, reference databases serve as the foundational framework against which sequencing reads are compared and taxonomically annotated. When these databases contain errors—such as incorrect taxonomic assignments or contaminating sequences—these issues propagate through the entire analytical pipeline, potentially leading to misinterpretation of microbial community structures, false associations in ecological studies, or incorrect pathogen identification in clinical settings. The growing reliance on mNGS across research and clinical domains makes addressing these database quality issues an urgent priority for the field.
Understanding Database Limitations: Taxonomic Errors and Contamination
Taxonomic annotation errors represent a significant challenge in bioinformatics, occurring when sequences are assigned to incorrect taxonomic lineages in reference databases. These errors are particularly problematic in widely used databases like Greengenes, where systemic issues have been documented. A notable example discovered in Greengenes versions 135 and 138 involved the misclassification of entire bacterial families: 100% of sequences assigned to the Pseudoalteromonadaceae family were improperly placed within the Vibrionales order instead of the correct Alteromonadales order [83]. Furthermore, over 20% of these misclassified sequences were actually from Vibrio species that had been incorrectly assigned to the Pseudoalteromonadaceae family rather than their proper taxonomic home in Vibrionaceae [83].
The ramifications of such errors extend far beyond theoretical classification concerns. An analysis of the literature revealed 68 peer-reviewed papers published between 2013 and 2018 that likely included these erroneous annotations specifically related to Vibrionales and Pseudoalteromonadaceae, with 20 studies explicitly stating the incorrect taxonomy in their results [83]. Given the ecological and clinical importance of these taxa—including their roles as conditionally rare organisms, potential pathogens, and antagonists in marine systems—such misclassifications can lead to fundamentally flawed interpretations of microbial community dynamics and function.
Sequence Contamination in Reference Materials and Reagents
Contaminating DNA represents another critical challenge for reference databases and mNGS workflows. This contamination can originate from multiple sources, including laboratory reagents, DNA extraction kits, and the laboratory environment itself. Studies have demonstrated that commercial DNA extraction reagents from various brands contain distinct background microbiota profiles, including some containing common pathogenic species that could significantly affect clinical interpretation [84]. Perhaps more concerningly, these contamination patterns show significant variability between different manufacturing lots of the same reagent brand, highlighting the need for lot-specific microbiota profiling rather than assuming consistent contamination profiles across products [84].
The impact of contamination is particularly pronounced in low-microbial-biomass samples, where contaminating DNA can easily overwhelm the true biological signal. This problem affects not only clinical samples but also reference materials used to build and validate databases. Without proper contamination tracking and removal, these foreign sequences become incorporated into reference databases, perpetuating false positives in subsequent analyses.
Table 1: Common Types of Errors in Microbial Reference Databases
| Error Type | Description | Impact on Analysis |
|---|---|---|
| Taxonomic Misclassification | Sequences assigned to incorrect taxonomic lineages (e.g., wrong order or family) | Misrepresentation of microbial community structure; erroneous ecological inferences |
| Sequence Contamination | Non-target DNA from reagents, environment, or cross-sample contamination | False positive identifications; reduced specificity in pathogen detection |
| Incomplete Metadata | Missing or inaccurate contextual information about reference sequences | Limited ability to filter or validate database entries |
| Uneven Taxonomic Coverage | Overrepresentation of some taxa and underrepresentation of others | Biased taxonomic assignments; reduced sensitivity for rare taxa |
Strategies for Building and Curating High-Quality Reference Databases
Data Source Selection and Evaluation
Constructing a high-quality reference database begins with careful selection of source data from public repositories and specialized collections. The International Nucleotide Sequence Database Collaboration (INSDC), comprising GenBank, the European Nucleotide Archive (ENA), and the DNA Data Bank of Japan (DDBJ), serves as the primary source for most publicly available sequence data [82]. However, because these databases accept submissions from researchers worldwide with minimal curation, they contain significant variations in data quality, annotation accuracy, and completeness.
For critical applications, preference should be given to curated databases like RefSeq, which undergoes additional quality control and filtering [82]. Specialized resources such as the FDA-ARGOS (Database for Reference Grade Microbial Sequences) provide particularly valuable reference materials as they are specifically designed for diagnostic use and contain well-characterized, high-quality genomes [82]. The Global Catalogue of Type Strains (gcType) maintained by China's National Microbiology Data Center represents another excellent resource, having sequenced and assembled numerous prokaryotic type strains to fill gaps in public databases [82].
When building clinical databases, the Global Catalogue of Pathogens (gcPathogen) offers a comprehensive collection focused on human pathogens, integrating data from 509 bacterial species (1.1 million genomes), 407 fungal species (6,785 genomes), 226 viruses (90,000 genomes), and 174 parasites (670 genomes) [82]. This targeted approach helps ensure relevant coverage for clinical applications while maintaining quality standards.
Genome Data Quality Control and Curation
Robust quality control processes are essential for identifying and removing problematic sequences before their inclusion in reference databases. The following multi-layered approach represents best practices for database curation:
Taxonomic Information Assessment: Public database entries frequently contain classification errors due to submitter mistakes or limitations in historical classification methods. To address this, average nucleotide identity (ANI) calculations or phylogenetic tree construction should be performed to verify the taxonomic placement of each candidate genome [82]. Genomes that cluster with references from different taxa should be flagged for further investigation or exclusion.
Sequence Quality and Assembly Assessment: Genomes should be evaluated for completeness, fragmentation, and potential sequencing artifacts. Metrics such as N50 (median contig length), total assembly size, and gene content completeness provide valuable indicators of assembly quality [82]. Excessively fragmented genomes or those with abnormal size or GC content relative to their taxonomic group should be scrutinized more carefully.
Contamination Screening: All candidate sequences should undergo comprehensive contamination screening using tools specifically designed for this purpose. This process identifies sequences of foreign origin (e.g., vector sequences, adapter contamination, or DNA from other organisms) that may have been inadvertently incorporated during sequencing or assembly [82]. The presence of excessive contamination should disqualify a genome from inclusion.
Table 2: Quality Control Metrics for Reference Genome Selection
| Quality Dimension | Recommended Metrics | Acceptance Thresholds |
|---|---|---|
| Taxonomic Accuracy | Average Nucleotide Identity (ANI), phylogenetic consistency | >95% ANI with type strain; monophyletic with conspecifics |
| Assembly Completeness | Number of contigs, N50, presence of core genes | Varies by organism; check against expected genome size |
| Contamination Level | Proportion of foreign sequences, inconsistent marker genes | <5% contamination; species-specific thresholds for clinical use |
| Sequence Quality | Q scores, read depth coverage, error rates | Q30+ for sequencing reads; even coverage distribution |
| Annotation Quality | Presence of standard annotations, functional predictions | RNA genes identified; protein-coding genes with functional attribution |
Advanced Methodologies for Contamination Identification and Removal
Experimental Approaches for Contamination Control
Innovative experimental methods have emerged to address the challenge of distinguishing true biological signals from contamination in metagenomic studies. Sample-Intrinsic microbial DNA Found by Tagging and sequencing (SIFT-seq) represents a powerful approach that tags sample-intrinsic DNA directly in clinical samples (e.g., plasma, urine) before DNA isolation [85]. This method uses bisulfite salt-induced conversion of unmethylated cytosines to uracils to chemically label the DNA present in the original sample. Any contaminating DNA introduced after this tagging step lacks the conversion signature and can be bioinformatically identified and removed during analysis [85].
The effectiveness of SIFT-seq has been demonstrated across multiple sample types and clinical scenarios. In validation experiments, SIFT-seq achieved an average 99.8% reduction in molecules mapping to spiked-in contaminant species [85]. When applied to clinical samples, the method reduced reads from common contaminant genera by up to three orders of magnitude, with 77% of contaminant genera completely removed from all samples after bioinformatic filtering [85]. This dramatic reduction in background noise significantly improves the specificity of pathogen detection in challenging low-biomass clinical samples.
Bioinformatics Techniques for Contamination Detection
Complementary to experimental methods, sophisticated bioinformatics approaches provide powerful tools for identifying and removing contamination. Strain-resolved analysis has emerged as a particularly effective method for detecting cross-contamination between samples processed on the same extraction plate [86]. This approach leverages the high resolution of strain tracking to identify sharing patterns that indicate well-to-well contamination during sample processing.
In one case study, researchers analyzed 402 fecal samples from infant-mother pairs and identified clear patterns of cross-sample contamination by examining strain sharing in the context of extraction plate coordinates [86]. Their analysis revealed that nearby samples on the same extraction plate were significantly more likely to share strains than distant samples (p = 2.3e-3 and 4.7e-3 for two plates), indicating well-to-well contamination during DNA extraction [86]. This pattern was visualized by mapping strain sharing relationships onto the plate layout, clearly showing that contamination events predominantly occurred between adjacent wells.
The following workflow diagram illustrates the strain-resolved approach for contamination detection:
Best Practices for Database Implementation and Maintenance
Database Construction and Validation Framework
Building a high-quality reference database requires a systematic approach that incorporates multiple validation steps and quality checkpoints. The following workflow outlines the key stages in database development, from initial data collection through to final implementation:
Implementation of the final database should include comprehensive documentation detailing the sources of all sequences, quality metrics applied during filtering, and any known limitations or gaps in taxonomic coverage. Regular performance validation against known reference materials and well-characterized clinical samples provides essential quality assurance before deployment in production environments.
Ongoing Maintenance and Updates
Reference databases are not static resources but require continuous maintenance to remain effective. Systematic processes should be established for regular database updates, incorporating new reference genomes, taxonomic revisions, and corrections to existing entries. The rapid pace of microbial genome sequencing means that databases can quickly become outdated if not regularly refreshed.
A critical aspect of database maintenance is the establishment of feedback mechanisms allowing users to report potential errors or problematic sequences. These reports should be systematically investigated, and confirmed errors should be corrected in subsequent database releases. Version control is essential, with detailed changelogs documenting all modifications, additions, and deletions between versions.
Additionally, database performance should be continuously monitored against emerging taxonomic groups and newly discovered pathogens. Proactive sequencing efforts targeting underrepresented taxonomic groups, particularly those with clinical relevance, can help address coverage gaps. For example, despite over 400 fungal species with documented human infections, public databases contain genomic data for fewer than 300 of these species, leaving significant gaps that can affect diagnostic accuracy [82].
Essential Research Reagent Solutions for Contamination Control
Successful implementation of contamination-controlled metagenomic studies requires careful selection of reagents and materials specifically designed to minimize background DNA contamination. The following table summarizes key solutions for maintaining database integrity and reducing false positives:
Table 3: Research Reagent Solutions for Contamination Control
| Reagent Category | Specific Examples | Function and Importance |
|---|---|---|
| DNA Extraction Kits (Low Bioburden) | KAPA Hyper Prep Kit, PCR-free kits | Minimize introduction of microbial DNA during extraction; critical for low-biomass samples |
| Ultrapure Water Systems | Molecular-grade water certified for NGS | Ensure water used in reagents doesn't contain amplifiable microbial DNA |
| Negative Control Materials | ZymoBIOMICS Spike-in Controls, extraction blanks | Monitor contamination levels; validate reagent purity across lots |
| DNA Decontamination Reagents | DNase treatment solutions, DNA-excluding centrifugation filters | Remove contaminating DNA from reagents prior to use |
| Indexed Adapter Systems | Unique dual index (UDI) adapters | Prevent index hopping and cross-contamination during multiplexed sequencing |
Taxonomic errors and sequence contamination in reference databases represent significant challenges that can compromise the validity of metagenomic studies and clinical diagnostics. Addressing these issues requires a multi-faceted approach combining rigorous database curation, advanced experimental methods like SIFT-seq for contamination tracking, and sophisticated bioinformatic techniques such as strain-resolved analysis. Implementation of systematic quality control protocols throughout the database lifecycle—from initial genome selection through ongoing maintenance—is essential for producing reliable, reproducible results.
As metagenomic sequencing continues to expand into new research areas and clinical applications, the community must prioritize the development and adoption of standardized, high-quality reference databases. This will require collaborative efforts across institutions and disciplines to establish common standards, share resources, and implement validation frameworks. Only through such coordinated action can we fully realize the potential of metagenomic sequencing to advance our understanding of microbial communities and improve human health.
Metagenomic next-generation sequencing (mNGS) has emerged as a powerful, hypothesis-free tool for infectious disease diagnostics, capable of detecting bacteria, fungi, parasites, and viruses without a priori knowledge of a specific pathogen directly from clinical specimens [87]. This culture-independent methodology allows for the identification and genomic characterization of a vast array of microorganisms, potentially enabling the replacement of multiple targeted pathogen tests with a single universal assay [87]. However, a significant challenge impedes its clinical utility: the ability to accurately differentiate true pathogens from colonizing microorganisms or contaminants in the resulting complex datasets [88].
In clinical practice, the mere detection of microbial sequences does not equate to disease causation. The human body is a complex ecosystem hosting about 10^14 bacterial, fungal, and protozoan cells, representing thousands of microbial species known as the normal flora [89]. These microbes typically exist in harmony with the host, only causing disease if they gain access to normally sterile sites or if host immune defenses are compromised [89]. Furthermore, clinical specimens almost always contain host nucleic acid, often constituting over 99% of the sequenced material, and may also include nucleic acid from collection reagents, the environment, or laboratory contaminants [87] [90]. Therefore, a comprehensive framework for data interpretation is essential for clinicians and researchers to translate mNGS findings into accurate diagnoses and effective patient management strategies.
Key Concepts and Definitions
- Pathogen: A microorganism that has evolved specialized mechanisms for interacting with its host and can cause disease in an otherwise healthy host. Dedicated pathogens do not require that the host be immunocompromised or injured and possess virulence factors that enable colonization, niche acquisition, immune system subversion, replication using host resources, and transmission to a new host [89].
- Colonizer: A microorganism that is part of the normal flora and typically exists in a commensal relationship with the host at specific anatomical sites (e.g., skin, mouth, large intestine, vagina). These microbes only cause pathology if they translocate to sterile sites or the host becomes immunocompromised [89]. In mNGS studies, these are often reported as "normal microbial communities" [88].
- Contaminant: Nucleic acid not originating from the patient's infection, introduced during sample collection, processing, or sequencing. Sources can include collection tubes, laboratory reagents, or the environment, and are often identified through no-template control samples processed concurrently with clinical specimens [87] [88].
Quantitative Frameworks for Interpretation
The following tables summarize key quantitative metrics and clinical performance data essential for distinguishing pathogens from non-pathogens in mNGS results.
Table 1: mNGS Bioinformatics Thresholds for Pathogen Detection [88]
| Microorganism Category | Threshold Criteria | Rationale |
|---|---|---|
| Mycobacterium tuberculosis, Brucella, Nocardia | Stringently mapped read count ≥ 1 | Challenging DNA extraction, low contamination risk |
| Other Bacteria & Fungi | Minimum of 3 mapped reads | Mitigates false positives from low-level contamination |
| All Microorganisms | Reads per million (RPM) ≥ 10x no-template control | Filters reagent/environmental contaminants |
| Normal Microbial Communities | Relative abundance ≥ 1% | Identifies background flora/colonizers |
Table 2: Clinical Reclassification of mNGS Findings in Pulmonary Infection Study (n=97) [88]
| Initial mNGS Finding | Number of Strains | Reclassified as Colonizer/Flora | Percentage |
|---|---|---|---|
| All Potential Pathogens | 138 | 65 | 47.1% |
| Bacterial Strains | Not specified | 36 | Not specified |
| Fungal Strains | Not specified | 29 | Not specified |
| Oral Anaerobes (as Normal Flora) | Not specified | 1 (Reclassified as Pathogen) | Not specified |
Table 3: Diagnostic Performance of mNGS vs. Conventional Microbiological Tests (CMT) [88]
| Metric | mNGS | CMT | Clinical Context |
|---|---|---|---|
| Overall Detection Rate | 63.9% (62/97) | 27.8% (27/97) | Suspected pulmonary infections |
| Impact on Treatment | Antibiotics adjusted for 77.4% of mNGS-positive patients | N/A | Guided targeted therapy |
| Clinical Improvement | 93.5% of adjusted cases | N/A | Supports diagnostic accuracy |
| Key Pathogens Better Detected | Mycobacterium, fungal species, rare pathogens | Standard pathogens | Highlights mNGS fillable gaps |
Methodologies and Experimental Protocols
Wet-Lab Workflow and Host Depletion
A standardized protocol for mNGS of bronchoalveolar lavage fluid (BALF) exemplifies a robust methodological approach [88]:
- Sample Collection: BALF is collected via bronchoscopy, with the first 20 mL discarded to minimize contamination from the upper respiratory tract. The subsequent fluid is retained for testing.
- Sample Preprocessing: 500 µL of BALF is homogenized using dithiothreitol (DTT) to break down mucus.
- Cell Lysis: The sample is added to a tube containing zirconia beads and lysis buffer, followed by vortexing for 10 minutes to mechanically disrupt microbial cells.
- Nucleic Acid Extraction: DNA is extracted using the TIANamp Micro DNA Kit (Tiangen Biotech, China).
- Library Preparation: DNA libraries are constructed using the KAPA HyperPlus Kit (Roche), preparing the DNA for sequencing.
- Sequencing: Libraries are sequenced in single-end 50 bp mode on an Illumina NextSeq 550Dx platform, with a minimum depth of 20 million reads per sample.
A critical step for enhancing sensitivity is host DNA depletion. As clinical samples can contain over 99% human DNA, this host nucleic acid can mask microbial signals [90]. Depletion methods, such as those in the MolYsis kit series (Molzym), selectively remove human DNA, thereby increasing the relative abundance of microbial reads without requiring increased sequencing depth, which saves costs and improves the detection of low-abundance pathogens and antimicrobial resistance genes [90].
Essential Research Reagents and Tools
Table 4: Research Reagent Solutions for mNGS Workflows [90] [88]
| Item | Function | Example Product |
|---|---|---|
| Host DNA Depletion Kit | Selectively removes human DNA to increase microbial sequence yield | MolYsis Basic5/Complete5/Ultra-deep (Molzym) |
| Nucleic Acid Extraction Kit | Isolves total DNA from processed samples, crucial for yield and purity | TIANamp Micro DNA Kit (Tiangen Biotech) |
| DNA Library Prep Kit | Fragments and adds adapters to DNA for sequencing | KAPA HyperPlus Kit (Roche) |
| Sequencing Platform | High-throughput parallel sequencing of prepared libraries | Illumina NextSeq 550Dx; Oxford Nanopore Technologies |
| No-Template Control | Identifies contamination from reagents or laboratory processes | Nuclease-free water processed alongside clinical samples |
Critical Controls Across the mNGS Workflow
Implementing controls at every stage is vital for accurate data interpretation [90]:
- Sample Stage: Negative control (e.g., sample medium) to detect contaminants introduced during collection; positive control (e.g., external quality assurance samples) to verify method performance.
- DNA Extraction Stage: Internal extraction control to monitor extraction efficiency and reproducibility; negative control to identify contamination during extraction.
- Library Preparation Stage: Positive and negative controls to check kit functionality and detect "kitome" contamination (background contamination in reagents).
- Sequencing Stage: Positive and negative controls to confirm sequencing run performance.
- Bioinformatics Stage: In silico negative mock community to identify background signals; In silico positive mock community with known composition to validate the analysis pipeline.
An Integrated Framework for Clinical Interpretation
The diagram below outlines a systematic decision-making process for interpreting mNGS results, integrating technical metrics with clinical assessment.
Applying the Interpretation Framework
The decision pathway requires evaluating multiple lines of evidence:
- Technical Metrics: The initial filter requires the microbial signal to surpass predefined technical thresholds to minimize false positives from contamination [88].
- Clinical Plausibility: The clinician must determine if the microorganism is a known cause of the patient's specific clinical syndrome [87] [88].
- Specimen Type: Detection from a sterile site (e.g., CSF, tissue, normally sterile body fluid) provides stronger evidence for pathogenesis than detection from non-sterile sites (e.g., BALF, sputum) where colonization is common [89] [88].
- Host Immune Status: Underlying conditions and immune competence affect whether a colonizer might become an opportunistic pathogen [89].
- Corroborating Evidence: Final interpretation should integrate all available data, including clinical presentation, imaging findings, and results from other laboratory tests (culture, serology, PCR) [88].
Distinguishing pathogens from colonizers and contaminants is the cornerstone of effective clinical metagenomics. While mNGS provides unparalleled breadth in pathogen detection, its diagnostic value is fully realized only through rigorous, multi-faceted interpretation. This process demands the integration of quantitative bioinformatics thresholds, robust laboratory protocols with extensive controls, and careful clinical correlation. As the field advances, standardization of these interpretive frameworks, alongside the development of improved bioinformatics tools and databases, will be critical for translating the powerful technical capabilities of mNGS into improved patient outcomes. Future efforts are directed toward linking pathogen detection to the human immune response and leveraging machine learning to further refine diagnostic accuracy [90].
Evidence and Efficacy: Validating mNGS Performance Against Gold-Standard Methods
Metagenomic Next-Generation Sequencing (mNGS) is revolutionizing pathogen detection in clinical and research settings. This culture-independent technique allows for the unbiased sequencing of all nucleic acids in a sample, enabling the identification of bacteria, viruses, fungi, and parasites without prior knowledge of the causative organism [12]. As antimicrobial resistance continues to threaten global health and the limitations of conventional diagnostic methods become increasingly apparent, mNGS offers a powerful tool for comprehensive pathogen detection. This in-depth technical guide provides a systematic comparison of the diagnostic performance of mNGS against traditional methods—including microbial culture, polymerase chain reaction (PCR), and serological assays—within the broader context of advancing metagenomic sequencing for bacterial identification research. The analysis presented herein is intended to equip researchers, scientists, and drug development professionals with a clear understanding of the capabilities, limitations, and optimal applications of these technologies.
Performance Comparison Across Methodologies
Extensive clinical studies have directly compared the diagnostic performance of mNGS against conventional methods across various sample types and patient populations. The tables below summarize key performance metrics and characteristic profiles of each diagnostic approach.
Table 1: Comparative Diagnostic Performance of mNGS vs. Conventional Methods
| Diagnostic Method | Reported Sensitivity (Range) | Reported Specificity (Range) | Typical Turnaround Time | Key Advantages |
|---|---|---|---|---|
| Metagenomic NGS (mNGS) | 58.01% - 92.31% [19] [91] [92] | 85.40% - 100% [19] [91] [92] | 20 - 24 hours [93] [53] | Unbiased detection; identifies rare/novel pathogens; resistant to antibiotic pre-treatment [12] [19] |
| Microbial Culture | 21.65% - ~40% [19] [12] | ~99% [19] [94] | 2 - 5 days (weeks for mycobacteria) [92] [19] | Gold standard for viability; provides isolates for antibiotic susceptibility testing [19] |
| Real-Time PCR (RT-PCR) | ~90.38% (for MTB) [91] [92] | ~100% (for MTB) [91] [92] | Several hours | High sensitivity/specificity for targeted pathogens; rapid; quantitative (Ct values) [91] [92] |
| Serological Assays | Varies by pathogen | Varies by pathogen | Hours to days | Detects immune response; useful for historical exposure or non-cultivable pathogens |
Table 2: Characteristic Profiles and Application Suitability
| Parameter | mNGS | Conventional Culture | Targeted PCR/Serology |
|---|---|---|---|
| Pathogen Spectrum | Comprehensive, untargeted [12] | Limited to cultivable organisms [19] | Narrow, highly targeted |
| Impact of Prior Antibiotics | Low [95] [19] | High (reduces yield) [19] | Low |
| Ability to Detect Polymicrobial Infections | Excellent [95] [12] | Moderate (can be missed or overgrown) | Possible with multiplex panels |
| Quantification | Semi-quantitative (via read counts) [91] [92] | Quantitative (CFU) | Quantitative (Ct values) [91] |
| Ideal Use Case | Unexplained infections, immunocompromised hosts, rare pathogens [12] [96] | When antibiotic sensitivity testing is required, routine diagnostics | When a specific pathogen is suspected, high-throughput screening |
Analysis of Performance Data
The quantitative data reveals a consistent trend: mNGS demonstrates significantly higher sensitivity than traditional culture. A large study on febrile patients (n=368) reported mNGS sensitivity at 58.01% compared to 21.65% for culture [19]. This superior detection rate is particularly evident in challenging clinical scenarios, such as in periprosthetic joint infections (PJI) and lower respiratory tract infections (LRTI), where mNGS identified pathogens in 86.7% of LRTI cases versus 41.8% with traditional methods [12]. The key strength of mNGS lies in its ability to detect pathogens that are difficult to culture, including viruses, anaerobic bacteria, and slow-growing organisms like mycobacteria [12].
However, conventional culture maintains a critical advantage in specificity and, most importantly, its ability to provide a live isolate for antimicrobial susceptibility testing (AST), which is indispensable for guiding targeted therapy [19]. The performance of mNGS is also notably less affected by prior antibiotic administration, a major confounder for culture-based methods. Studies on PJI found that prior antibiotic use was a significant risk factor for discordant results where culture was negative but mNGS was positive [95].
When compared to molecular techniques like RT-PCR, mNGS and RT-PCR show high agreement in specific contexts, such as the detection of Mycobacterium tuberculosis (kappa = 0.896) [91] [92]. Their concordance is strongly influenced by microbial load, with higher agreement in samples with lower PCR cycle threshold (Ct) values, indicating a higher bacterial burden [91] [92]. While RT-PCR is excellent for detecting specific, known pathogens rapidly, mNGS provides a broader hypothesis-free approach.
Detailed Experimental Protocols
To ensure reproducible results, standardized protocols for sample processing, sequencing, and bioinformatic analysis are crucial. The following sections detail common experimental workflows.
Protocol for mNGS from Bronchoalveolar Lavage Fluid (BALF)
Sample Collection and Pre-processing:
- Collect 5-10 mL of BALF via bronchoscopy into a sterile container [93].
- For DNA-only mNGS, split the sample. For comprehensive detection, process the same sample for both DNA and RNA sequencing to identify DNA pathogens, RNA viruses, and actively transcribing organisms [93].
- Centrifuge the sample to remove human cells. Use the supernatant for cell-free DNA (cfDNA) extraction or the pellet for total nucleic acid extraction [97].
DNA/RNA Extraction and Library Preparation:
- Extract total DNA using a commercial kit (e.g., QIAamp UCP Pathogen DNA Kit) [93]. For RNA, use a viral RNA kit (e.g., QIAamp Viral RNA Kit) followed by ribosomal RNA depletion [93].
- For DNA libraries, fragment the DNA, perform end-repair, add adapters, and amplify via PCR. For RNA, perform reverse transcription to cDNA before library construction [93] [53].
- Assess the final library's concentration and quality using a fluorometer (e.g., Qubit) and bioanalyzer (e.g., Agilent 2100) [53] [97].
Sequencing and Bioinformatic Analysis:
- Sequence the library on a high-throughput platform (e.g., Illumina NextSeq 550, BGISEQ-50) to generate millions of single-end or paired-end reads [93] [53].
- Process raw data through a bioinformatic pipeline: (1) Remove low-quality reads and adapter sequences with tools like Fastp; (2) Subtract human host sequences by aligning to a reference genome (e.g., hg38) using Burrows-Wheeler Aligner (BWA) or SNAP; (3) Align the remaining non-host reads to comprehensive microbial databases (e.g., NCBI RefSeq) for taxonomic classification [93] [53].
Interpretation and Positive Criteria:
- A positive result is determined by specific thresholds. For common bacteria, criteria may include a top-10 genome coverage rank for that microbe type AND no detection in negative controls, or a RPM (Reads Per Million) sample/NTC (Non-Template Control) ratio >10 [97].
- For critical pathogens like Mycobacterium tuberculosis, even a single unique read mapped to the species may be considered positive if absent from the negative control [97].
Protocol for Conventional Culture from BALF
- Inoculate BALF sample onto appropriate solid media (e.g., blood agar, chocolate agar, Sabouraud dextrose agar) for bacteria and fungi [19].
- Incubate plates under suitable atmospheric conditions (aerobic, CO₂, anaerobic) at 35±1°C for 24-48 hours (longer for fungi and mycobacteria) [19].
- Identify resulting colonies using MALDI-TOF Mass Spectrometry [19].
- Perform antibiotic susceptibility testing (AST) on positive cultures using standardized methods like disk diffusion or automated systems (e.g., VITEK II) to determine Minimum Inhibitory Concentrations (MICs) according to CLSI guidelines [19].
Workflow Visualization
The following diagrams illustrate the core technical and logical workflows for mNGS and conventional diagnostics, highlighting the points of differentiation.
Diagram 1: The mNGS Diagnostic Workflow. This culture-independent process converts nucleic acids from a clinical sample directly into a diagnostic report through sequencing and computational analysis.
Diagram 2: Conventional Culture vs. Targeted PCR Workflows. Culture is a growth-based method that enables AST, while PCR is a rapid, targeted molecular test for specific pathogens.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of diagnostic methods relies on a suite of specific reagents and instruments. The following table details key solutions used in the featured experiments.
Table 3: Key Research Reagent Solutions for mNGS and Comparative Methods
| Item Name | Specific Function | Example Product/Citation |
|---|---|---|
| Nucleic Acid Extraction Kit | Isolation of total DNA/RNA or cfDNA from diverse clinical samples. | QIAamp UCP Pathogen DNA Kit, QIAamp DNA Micro Kit [93] [97] [19] |
| Library Preparation Kit | Construction of sequencing-ready libraries from extracted nucleic acids. | Ovation Ultralow System V2, PMseq RNA Infection Pathogen Detection Kit, QIAseq Ultralow Input Library Kit [93] [53] [19] |
| NGS Platform | High-throughput sequencing of prepared libraries. | Illumina NextSeq 550, BGISEQ-50/MGISEQ-2000 [93] [53] |
| Bioinformatic Tools | Data processing, host subtraction, and microbial classification. | Fastp (QC), BWA (host subtraction), BLASTN/SNAP (microbial alignment) [93] [97] |
| Automated PCR System | Automated nucleic acid extraction and real-time PCR amplification. | Sanity 2.0 System [92] |
| Microbial Identification System | Rapid identification of bacterial and fungal colonies from culture. | MALDI-TOF MS (Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry) [97] [19] |
| Automated Culture System | Automated monitoring of microbial growth in liquid cultures. | BD BACTEC FX system [97] |
Discussion and Clinical Utility
The integration of mNGS into diagnostic pathways has a direct and significant impact on clinical decision-making and patient management. Evidence shows that mNGS results lead to changes in antibiotic therapy in a substantial proportion of patients (up to 72.13% in one LRTI study), including de-escalation from broad-spectrum agents, initiation of targeted treatment, and discontinuation of unnecessary antibiotics [12] [19]. This is particularly valuable in complex cases involving immunocompromised hosts, where mNGS demonstrated a superior detection rate (98/146 patients) compared to conventional microbiological testing (50/146 patients) [96].
The choice between mNGS, culture, and PCR is not a matter of selecting a single superior technology but of understanding their complementary roles. A meta-analysis of PJI diagnostics concluded that mNGS has higher sensitivity while targeted NGS (tNGS) has higher specificity, and both can be clinically viable depending on the context [94]. mNGS is ideally suited for hypothesis-free diagnosis in complex cases, while targeted PCR or tNGS is more efficient and cost-effective for confirming specific suspected pathogens or when looking for resistance genes [93].
In conclusion, mNGS represents a transformative tool in the diagnostic arsenal, offering unparalleled breadth in pathogen detection. Its optimal use, however, lies in a synergistic approach with conventional methods. Culture remains essential for antimicrobial susceptibility testing, and targeted molecular methods provide rapid, sensitive confirmation for specific pathogens. Future developments in sequencing speed, cost reduction, and standardized bioinformatic pipelines will further solidify the role of mNGS in both clinical diagnostics and bacterial identification research.
The rapid and accurate identification of pathogens is a cornerstone of effective management for severe infections, yet it remains a significant challenge in clinical practice. Conventional microbiological testing (CMT) methods, including culture, serological assays, and targeted polymerase chain reaction (PCR), are often limited by turnaround times, low sensitivity, and a narrow scope of detectable pathogens [51]. These limitations are particularly pronounced in critically ill patients, such as those with severe pneumonia or sepsis in intensive care units (ICUs), where delayed or inaccurate etiological diagnosis can lead to inappropriate empirical antibiotic therapy and adversely affect patient outcomes [98]. Metagenomic next-generation sequencing (mNGS) represents a paradigm shift in infectious disease diagnostics. This culture-independent, high-throughput technology allows for the unbiased detection and identification of all nucleic acids (bacteria, fungi, viruses, and parasites) present in a clinical sample, offering the potential to revolutionize the diagnosis of severe infections [51]. This technical guide, framed within a broader thesis on the introduction of metagenomic sequencing for bacterial identification research, synthesizes recent real-world evidence to analyze the superior diagnostic performance of mNGS, detail its experimental protocols, and discuss its implications for research and clinical practice.
Comparative Diagnostic Performance: mNGS vs. Conventional Methods
Recent clinical studies conducted across diverse patient populations and sample types consistently demonstrate the superior sensitivity and etiological diagnosis rate of mNGS compared to CMT.
A large retrospective study of 323 ICU patients with suspected severe pneumonia found that the positivity rate of mNGS on bronchoalveolar lavage fluid (BALF) and blood samples was significantly higher than that of CMT (93.5% vs. 55.7%, p < 0.001) [98]. The sensitivity of mNGS was reported at 94.74%, drastically outperforming CMT's sensitivity of 57.24% (p < 0.001) [98]. This trend is confirmed by other studies: in a cohort of 180 patients with severe infections, the etiological diagnosis rate for mNGS was 78.89%, compared to just 20% for CMT (p < 0.001) [99]. Similarly, in patients with lower respiratory tract infections (LRTI), mNGS showed a positive rate of 86.7% versus 41.8% for traditional methods (p < 0.05) [12].
Table 1: Comparative Diagnostic Performance of mNGS versus Conventional Microbiology Testing (CMT)
| Study Population & Sample Size | Sample Types | mNGS Positivity Rate | CMT Positivity Rate | mNGS Sensitivity | CMT Sensitivity | Key Statistical Significance |
|---|---|---|---|---|---|---|
| 323 ICU patients with suspected severe pneumonia [98] | BALF, Blood | 93.5% | 55.7% | 94.74% | 57.24% | p < 0.001 |
| 180 patients with severe infections [99] | BALF, Blood | 78.89% (Diagnosis rate) | 20% (Diagnosis rate) | Not specified | Not specified | p < 0.001 |
| 165 patients with lower respiratory tract infections (LRTI) [12] | BALF, Blood, Tissue, Pleural Effusion | 86.7% | 41.8% | Not specified | Not specified | P < 0.05 |
| 163 patients with acute infection in ED [100] | Multiple (Sputum, BALF, etc.) | 71.4% | 40.8% | 92.9% | Not specified | p < 0.001 |
| 132 adult patients with severe pneumonia [101] | BALF | 82.58% (for bacteria) | 63.64% (for bacteria) | Significantly higher | Lower | P < 0.05 |
Pathogen Spectrum and Polymicrobial Infections
The unbiased nature of mNGS enables a much broader detection of pathogen spectra. In one study, mNGS identified 36 bacterial species, 14 fungal species, 7 viral species, and 1 Chlamydia species, whereas CMT detected only 21 bacterial and 9 fungal species [98]. This comprehensive coverage is crucial for identifying rare, fastidious, or atypical pathogens that are frequently missed by CMT, such as Mycobacterium tuberculosis complex, Legionella pneumophila, Chlamydia psittaci, and Pneumocystis jirovecii [101]. Furthermore, mNGS excels in diagnosing polymicrobial infections, which are common in severe pneumonia. The detection rate for mixed infections was significantly higher with mNGS than with CMT (62.8% vs. 18.3%, p < 0.001) [98]. Another study reported that bacterial-fungal co-infections were the most prevalent form of mixed infection, accounting for 77.3% of cases [100].
Specificity and Technical Considerations
While mNGS demonstrates superior sensitivity, its specificity is generally lower than that of culture, which remains the gold standard due to its high specificity. One analysis reported the specificity of mNGS at 26.32%, compared to 68.42% for CMT (p < 0.01) [98]. Another study found specificities of 75.9% for mNGS and 92.6% for culture [100]. This lower specificity is attributed to challenges in distinguishing true pathogens from environmental contaminants, colonizing organisms, or non-viable microbial DNA, necessitating careful interpretation of results within the clinical context [98] [51].
Table 2: Pathogen Profile and Detection of Mixed Infections
| Parameter | Findings from mNGS Studies | Comparison to CMT |
|---|---|---|
| Predominant Bacterial Pathogens | Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Staphylococcus aureus [98] [101] | Consistently detected by both methods, but mNGS identifies more species. |
| Predominant Fungal Pathogens | Candida albicans, Aspergillus species [101] [100] | mNGS shows comparable or superior detection rates. |
| Viral Pathogens | COVID-19, Influenza virus [101] | mNGS demonstrates a significant advantage (67.42% vs 37.88%) [101]. |
| Rare/Atypical Pathogens | Mycobacterium tuberculosis complex, Nontuberculous mycobacteria, Legionella pneumophila, Chlamydia psittaci [101] | Largely undetectable by routine CMT; a key advantage of mNGS. |
| Detection of Mixed Infections | mNGS detection rate: 62.8% [98]; Bacterial-fungal most common mixed type (77.3%) [100] | CMT detection rate: 18.3% (p < 0.001) [98] |
Detailed Experimental Protocols for mNGS
A standardized, robust experimental protocol is critical for generating reliable and reproducible mNGS data in a clinical research setting.
Sample Collection and Pre-processing
The choice of sample type depends on the clinical presentation. For severe respiratory infections, BALF is the preferred sample due to its proximity to the site of infection [98] [12]. BALF is collected via fiberoptic bronchoscopy, where a bronchoscope is inserted into the affected lung segment and lavaged with multiple aliquots of sterile saline; at least 40% of the instilled fluid should be aspirated and collected into a sterile container [98]. Other common sample types include tissue (e.g., FFPE), blood, sputum, and pleural effusion [12] [102]. For blood samples, research has compared whole-cell DNA (wcDNA) from the pellet versus cell-free DNA (cfDNA) from the plasma. One study found that wcDNA mNGS had a higher concordance with culture (63.33%) than cfDNA mNGS (46.67%) and was associated with a lower mean host DNA proportion (84% vs. 95%, p < 0.05), which can improve sequencing efficiency [103].
Nucleic Acid Extraction and Library Preparation
Nucleic acid extraction is performed using commercial kits, such as QIAGEN’s QIAamp Pathogen Kit, following the manufacturer's protocol to efficiently lyse cells and extract both DNA and RNA [98]. For DNA-only workflows, this step isolates total DNA. For comprehensive pathogen detection, RNA can also be extracted and reverse-transcribed to cDNA. The extracted nucleic acids then undergo library preparation, which involves fragmenting the DNA/cDNA, attaching universal adapters, and, in some cases, performing PCR amplification. This process can be accomplished using kits like the VAHTS Universal Pro DNA Library Prep Kit for Illumina [103]. A critical quality control step is the inclusion of negative controls (e.g., sterile water) in each batch to monitor for laboratory and reagent contamination, which is essential for accurate interpretation of results [103] [12].
Sequencing and Bioinformatic Analysis
Prepared libraries are sequenced on high-throughput platforms. The Illumina NextSeq 550DX and NovaSeq 6000 are widely used for this purpose, typically generating 20-50 million high-quality paired-end reads (e.g., 2x150 bp) per sample [98] [103]. The subsequent bioinformatic analysis is a multi-step process:
- Quality Control and Host Depletion: Raw sequencing reads are processed to remove low-quality sequences, adapter contaminants, and short reads. A crucial step involves aligning reads to a human reference genome (e.g., hg38) to subtract host-derived sequences, which can constitute over 95% of the total data in blood samples [98] [103].
- Microbial Identification: The remaining non-host reads are systematically aligned against comprehensive microbial genomic databases (e.g., NCBI RefSeq) to assign taxonomic classifications at various levels (species, genus, etc.).
- Criteria for Positivity: To minimize false positives, stringent criteria are applied. These may include: a minimum number of unique reads mapped to a specific pathogen (e.g., ≥3 for most bacteria, ≥1 for slow-growing mycobacteria), a minimum number of reads mapping to distinct genomic regions, and a significant statistical over-representation compared to negative controls (e.g., z-score > 3) [98] [103].
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of mNGS in a research setting relies on a suite of specific reagents and instruments.
Table 3: Key Research Reagent Solutions for mNGS Workflow
| Category | Item | Specific Example(s) | Function in Workflow |
|---|---|---|---|
| Sample Collection & Storage | Sterile specimen containers, RNA/DNA stabilization solutions | Not specified | Maintains sample integrity and nucleic acid stability from collection to processing. |
| Nucleic Acid Extraction | Pathogen DNA/RNA Kit | QIAGEN QIAamp Pathogen Kit [98] | Efficiently lyses a wide range of pathogens (bacterial, fungal, viral) and purifies nucleic acids. |
| Cell-free DNA Extraction | cfDNA Kit | VAHTS Free-Circulating DNA Maxi Kit [103] | Specifically extracts microbial cfDNA from plasma or other liquid supernatant. |
| Library Preparation | DNA Library Prep Kit | VAHTS Universal Pro DNA Library Prep Kit for Illumina [103] | Fragments DNA and attaches sequencing adapters for compatibility with the sequencer. |
| Sequencing Platform | NGS System | Illumina NextSeq 550DX, NovaSeq 6000 [98] [103] | Performs high-throughput, parallel sequencing of prepared libraries. |
| Bioinformatics | Reference Databases | NCBI Genomic Database [98] | Reference sequences for aligning non-host reads and assigning taxonomic identity. |
| Bioinformatics | Analysis Software/Pipeline | CLC Genomics Workbench, Pavian [103] [102] | Software suite for quality control, host depletion, microbial alignment, and statistical analysis. |
Discussion and Future Directions
The accumulation of real-world data solidifies the position of mNGS as a powerful diagnostic tool with superior sensitivity for the etiological diagnosis of severe infections. Its ability to rapidly identify a broad spectrum of pathogens, including rare and atypical organisms, and to detect polymicrobial infections makes it an invaluable supplement to conventional methods, particularly in complex, critical, or culture-negative cases [98] [12] [101]. The clinical impact is significant, with studies reporting that mNGS results led to adjustments in antibiotic therapy in a substantial proportion of patients (up to 72.13%), facilitating both the initiation of targeted treatment and the de-escalation of unnecessary broad-spectrum antibiotics [12].
Despite its advantages, challenges remain. The lower specificity of mNGS compared to culture requires careful clinical correlation to distinguish colonization from true infection [98] [51]. The high cost of the technology, the need for standardized wet-lab and bioinformatic protocols across laboratories, and the complexity of interpreting the massive datasets generated are ongoing hurdles to widespread adoption [51]. Future developments in the field will likely focus on streamlining and standardizing workflows, reducing costs through targeted sequencing panels, improving bioinformatic tools for resistance gene prediction and virulence factor analysis, and integrating host-response biomarkers to enhance the interpretation of results. As these advancements mature, mNGS is poised to become an even more integral component of the diagnostic arsenal for severe infections, ultimately guiding more precise and effective patient management.
Metagenomic Next-Generation Sequencing (mNGS) represents a paradigm shift in microbiological diagnostics, enabling the detection of a vast array of pathogens without prior assumptions about causative agents. This hypothesis-free approach stands in contrast to traditional culture-based and targeted molecular methods, which remain the diagnostic mainstay in clinical laboratories worldwide. Understanding the contexts in which these divergent diagnostic approaches yield concordant or discordant results is fundamental for advancing microbial identification research and optimizing diagnostic strategies. This technical guide synthesizes current evidence to elucidate the patterns of agreement and disagreement between mNGS and conventional methods, providing researchers and drug development professionals with a framework for interpreting results across diverse clinical and experimental scenarios.
The integration of mNGS into diagnostic pathways requires careful consideration of its complementary role alongside established techniques. While traditional culture offers the irreplaceable benefit of yielding live isolates for antimicrobial susceptibility testing and phylogenetic studies, mNGS provides unparalleled breadth in pathogen detection, particularly for fastidious, novel, or unexpected organisms [10]. This whitepaper examines the technological underpinnings of both approaches, analyzes their performance characteristics across various infection types, and provides methodological guidance for implementing integrated diagnostic protocols in research settings.
Performance Comparison Across Infection Types
The diagnostic concordance between mNGS and traditional methods varies significantly across different infection types and patient populations. Understanding these variations is crucial for appropriate test selection and interpretation in both clinical and research contexts.
Lower Respiratory Tract Infections (LRTI)
In LRTI, mNGS demonstrates significantly higher sensitivity compared to traditional culture-based methods. A 2025 comprehensive study of 165 patients with suspected LRTI found that mNGS identified microbial etiology in 86.7% of cases compared to 41.8% with traditional methods [12]. The concordance rate between methods was approximately 63% in another study focusing on COVID-19 patients with LRTI [27]. mNGS exhibited particular strength in detecting polymicrobial infections and rare pathogens, identifying 29 pathogen species missed by conventional methods, including non-tuberculous mycobacteria (NTM), Prevotella, anaerobic bacteria, Legionella gresilensis, Orientia tsugamushi, and various viruses [12].
Table 1: Diagnostic Performance in Lower Respiratory Tract Infections
| Parameter | mNGS | Traditional Methods | Study Details |
|---|---|---|---|
| Sensitivity | 86.7-95.35% | 41.8-81.08% | 165 patients with suspected LRTI [12]; 43 patients with LRTI (including COVID-19) [27] |
| Pathogen Coverage | Broad spectrum, including viruses, bacteria, fungi, rare pathogens | Limited to culturable bacteria/fungi; targeted pathogen panels | 29 pathogen species detected only by mNGS [12] |
| Polymicrobial Infection Detection | Enhanced | Limited | Additional pathogens identified in 21% of ventilated pneumonia patients [22] |
| Concordance Rate | 60-63% | N/A | 33 consecutive LRT samples [22]; 43 patient samples [27] |
| Impact on Antimicrobial Therapy | 72.1% of cases led to treatment changes | N/A | 54 patients (32.73%) had antibiotics reduced [12] |
Invasive Fungal Infections
For invasive pulmonary fungal infections (IPFI), both mNGS and targeted NGS (tNGS) demonstrate superior performance compared to conventional microbiological tests (CMTs). A 2025 study of 115 patients with probable pulmonary infection reported sensitivity of 95.08% for both mNGS and tNGS, with specificities of 90.74% and 85.19%, respectively [104]. The detection rates for Pneumocystis jirovecii (42.6% for mNGS, 45.9% for tNGS), Candida albicans (31.1% for mNGS, 34.4% for tNGS), and Aspergillus fumigatus (26.2% for mNGS, 24.6% for tNGS) were substantially higher than culture-based methods [104]. Both NGS methodologies significantly outperformed conventional methods in diagnosing mixed infections, detecting bacterial-fungal co-infections in 65 (mNGS) and 55 (tNGS) out of 115 cases, compared to only nine cases detected by culture [104].
Periprosthetic Joint Infections (PJI)
In PJI diagnosis, a 2025 meta-analysis of 23 studies found that mNGS demonstrated pooled sensitivity of 0.89 (95% CI: 0.84-0.93) and specificity of 0.92 (95% CI: 0.89-0.95), while targeted NGS showed sensitivity of 0.84 (95% CI: 0.74-0.91) and specificity of 0.97 (95% CI: 0.88-0.99) [94]. The areas under the summary receiver-operating characteristic curves (AUCs) were 0.935 for mNGS and 0.911 for tNGS, with no statistically significant differences in diagnostic odds ratios between the approaches [94]. A separate 2025 study of 167 patients with suspected PJI identified several factors contributing to discordance between mNGS and culture results, including prior antibiotic use, polymicrobial infections, infections caused by rare pathogens, and the use of intraoperative tissue specimens [105].
Sepsis and Bloodstream Infections
In critical care settings, mNGS has demonstrated significant utility for sepsis management. A 2025 retrospective cohort study of 303 septic patients in the ICU found that mNGS-guided antimicrobial therapy was associated with reduced 28-day mortality [106]. After propensity score matching, the mNGS group showed significantly higher rates of antibiotic adjustment and lower mortality compared to the non-mNGS group receiving only conventional diagnostics [106]. For bacterial bloodstream infections, nanopore sequencing has shown excellent concordance with mass spectrometry for species identification, correctly identifying 37 bacterial isolates in positive blood cultures while also detecting one mixed bacterial-fungal infection missed by conventional methods [107].
Table 2: Diagnostic Performance Across Various Infection Types
| Infection Type | Sensitivity (mNGS) | Specificity (mNGS) | Key Advantages of mNGS | Study |
|---|---|---|---|---|
| Invasive Pulmonary Fungal Infection | 95.08% | 90.74% | Superior detection of fungal species and mixed infections | [104] |
| Periprosthetic Joint Infection | 89% (84-93%) | 92% (89-95%) | Better detection in antibiotic-pretreated patients | [94] |
| Culture-negative Endocarditis | 90-95% | High | Detection of fastidious and rare pathogens | [108] |
| Bacterial Bloodstream Infection | 100% (species ID) | 100% (species ID) | Detection of mixed infections; AMR gene profiling | [107] |
Experimental Protocols and Methodologies
Standard mNGS Workflow for Respiratory Samples
The following protocol details a unified metagenomic method for simultaneous detection of DNA and RNA microorganisms in respiratory samples, adapted from a 2024 study published in Communications Medicine [22]:
Sample Preparation:
- Collect respiratory samples (BALF, sputum, or nasal/throat swabs) in sterile containers.
- Centrifuge at 1200g for 10 minutes to pellet human cells and debris.
- Transfer 500 μL of supernatant to a tube containing 1.4 mm zirconium-silicate spheres (Lysing Matrix D).
- Mechanically disrupt samples using a tissue lyser at 50 oscillations/second for 3 minutes.
Host DNA Depletion:
- Transfer 200 μL of homogenized sample to a 1.5 mL Eppendorf tube.
- Add 10 μL of HL-SAN nuclease (ArcticZymes Technologies) without buffer.
- Incubate at 37°C for 10 minutes at 1000 rpm on a thermomixer to digest released human nucleic acids.
- Process samples through automated nucleic acid extraction system (MagNA Pure 24, Roche) using total nucleic acid isolation kit with 200 μL input and 50 μL elution volume.
Nucleic Acid Processing:
- For cDNA synthesis, add 4 μL of LunaScript RT SuperMix Kit to 16 μL of nucleic acid extract.
- Incubate per manufacturer's conditions for reverse transcription.
- Perform double-strand DNA synthesis using Sequenase version 2.0: 2 μL of 5× Sequenase buffer, 0.9 μL of Sequenase dilution buffer, 0.6 μL of Sequenase, and 7.7 μL nuclease-free water added to 20 μL template.
- Incubate at 37°C for 8 minutes.
- Purify with AMPure XP beads (45 μL beads to 31.2 μL reaction), wash twice with 70% ethanol, and elute in 10 μL nuclease-free water.
Library Preparation and Sequencing:
- Prepare DNA for sequencing using Rapid PCR barcoding kit with increased PCR cycles (30 cycles).
- Sequence on Nanopore flowcells (R9.4.1) on GridION platform, multiplexing 3-10 samples per flowcell.
- Perform base-calling and demultiplexing using Guppy (version 6.1.5) within MinKNOW software.
- Filter reads with q-score <7 and length <100 bp.
This unified protocol decreases human DNA concentration by a median of eight Ct values while maintaining detection of a broad range of RNA and DNA viruses, bacteria (including atypical pathogens), and fungi, with the first automated reports generated after 30 minutes of sequencing in a 7-hour end-to-end workflow [22].
Targeted NGS for Fungal Detection
For specific detection of fungal pathogens, a targeted NGS approach can be employed using the following protocol adapted from a 2025 study on IPFI [104]:
Sample Processing:
- Add 650 μL of BALF sample to an equal volume of dithiothreitol (80 mmol/L) in a 1.5 mL centrifuge tube.
- Vortex for 15 seconds to homogenize.
- Extract total nucleic acid using MagPure Pathogen DNA/RNA Kit per manufacturer's instructions.
Library Construction for tNGS:
- Use Respiratory Pathogen Detection Kit with 198 pathogen-specific primers for ultra-multiplex PCR.
- Perform two rounds of PCR amplification to enrich target sequences.
- Purify PCR products with bead-based clean-up.
- Amplify with primers containing sequencing adapters and unique barcodes.
- Assess library quality using Qsep100 Bio-Fragment Analyzer and Qubit 4.0 fluorometer.
- Dilute library to 1 nmol/L for sequencing.
This targeted approach demonstrates sensitivity of 95.08% and specificity of 85.19% for diagnosing invasive pulmonary fungal infections [104].
Factors Influencing Diagnostic Concordance
Several technical and clinical factors significantly impact the agreement between mNGS and traditional diagnostic methods. Understanding these variables is essential for proper interpretation of discordant results.
Technical and Preanalytical Factors
The concordance between mNGS and traditional methods is highly dependent on specimen type, with consistency in specimen type identified as a protective factor against discordance (OR = 0.471, 95%CI=0.254-0.874, P = 0.017) [105]. Sample processing methodologies significantly impact results, particularly host DNA depletion efficiency, which can improve microbial signal detection in low-biomass samples [10] [22]. The sequencing platform and bioinformatic pipelines also contribute to variability, with different thresholds for pathogen identification affecting specificity [104] [107]. For instance, studies utilize various read count thresholds (RPM ratio ≥10 or pathogen-specific read counts) to distinguish true pathogens from background contamination [104].
Clinical and Biological Factors
Prior antibiotic exposure represents a major factor in diagnostic discordance, significantly increasing the likelihood of negative cultures despite positive mNGS findings (OR = 2.137, 95% CI = 1.069-4.272, P = 0.032) [105]. The microbial composition of infections also affects concordance, with polymicrobial infections (OR = 3.245, 95% CI = 1.278-8.243, P = 0.013) and infections caused by rare pathogens (OR = 2.735, 95% CI = 1.129-6.627, P = 0.026) more likely to yield discordant results [105]. Patient immune status further influences detection patterns, as pathogen spectra differ between immunocompetent and immunocompromised individuals, with the latter showing more diverse and opportunistic pathogens [12].
Visualization of Diagnostic Pathways
The following diagnostic workflow illustrates the integrated approach to resolving concordant and discordant results between mNGS and traditional methods:
Integrated Diagnostic Pathway
Research Reagent Solutions
The following essential materials and reagents represent critical components for implementing mNGS protocols in research settings:
Table 3: Essential Research Reagents for mNGS Workflows
| Reagent/Kit | Function | Application Note |
|---|---|---|
| Zirconium-silicate spheres (1.4 mm) | Mechanical lysis of human cells | Preserves diverse microorganisms while disrupting host cells [22] |
| HL-SAN nuclease | Digestion of free human nucleic acids | Works without buffer; digests DNA more efficiently than RNA [22] |
| QIAamp UCP Pathogen DNA/RNA Kits | Simultaneous extraction of DNA and RNA | Includes human DNA depletion steps [104] |
| LunaScript RT SuperMix Kit | cDNA synthesis from RNA pathogens | Essential for RNA virus detection [22] |
| Rapid PCR Barcoding Kit (ONT) | Library preparation for nanopore sequencing | Enables rapid turnaround with minimal hands-on time [22] [107] |
| Respiratory Pathogen Detection Kit | Targeted NGS for pathogen identification | Contains 198 pathogen-specific primers for comprehensive detection [104] |
| AMPure XP Beads | Nucleic acid purification and size selection | Critical for removing contaminants and concentrating targets [22] |
The relationship between mNGS and traditional diagnostic methods is characterized by both complementary strengths and instructive discordances. While mNGS demonstrates superior sensitivity and broader pathogen detection capacity, conventional methods retain irreplaceable value in providing viable isolates for antimicrobial susceptibility testing and downstream applications. The consistent observation that prior antibiotic exposure, fastidious organisms, and polymicrobial infections contribute to diagnostic discordance highlights the limitations of culture-dependent approaches while simultaneously validating the clinical utility of culture-independent mNGS.
For researchers and drug development professionals, these findings underscore the importance of implementing orthogonal diagnostic approaches that leverage the respective strengths of each technology. The integrated diagnostic pathway presented in this whitepaper provides a framework for reconciling discordant results through multidisciplinary correlation, ultimately leading to more precise pathogen identification and targeted therapeutic interventions. As methodological standardization improves and costs decrease, the strategic integration of mNGS with traditional microbiological methods will undoubtedly accelerate both clinical diagnostics and fundamental research in microbial pathogenesis and antimicrobial development.
The integration of metagenomic next-generation sequencing (mNGS) into clinical microbiology represents a paradigm shift in infectious disease diagnostics, offering hypothesis-free detection of bacteria, viruses, fungi, and parasites directly from clinical specimens [10]. Unlike traditional culture and targeted molecular assays, mNGS enables identification of novel, fastidious, and polymicrobial infections while simultaneously characterizing antimicrobial resistance (AMR) genes [10]. This transformative capability is particularly valuable in complex diagnostic scenarios such as pyrexia of unknown origin (PUO), sepsis, and infections in immunocompromised patients where conventional methods often fail [10] [109]. However, the advanced technological capabilities of mNGS introduce significant economic and operational challenges that clinical laboratories must navigate to ensure sustainable implementation.
Metagenomic sequencing operates within a dynamic financial landscape characterized by continuous volatility driven by both market forces and legislative actions [110]. Clinical laboratories face mounting pressures from regulatory changes, declining reimbursement rates, and technological advancements that require substantial capital investment [110]. The Protecting Access to Medicare Act (PAMA) has fundamentally altered the payment landscape by mandating that the Centers for Medicare & Medicaid Services (CMS) base payment rates on private payer data, frequently resulting in reductions to federally mandated fee schedules [110]. This regulatory environment necessitates that laboratories treat all expenses as variable and subject to immediate reduction through proactive cost control measures while simultaneously demonstrating clinical utility for reimbursement [110].
Table 1: Key Economic Pressures Affecting Clinical Laboratory Operations
| Pressure Category | Specific Challenges | Financial Impact |
|---|---|---|
| Regulatory Compliance | CLIA, CAP adherence; PAMA implementation; CMS payment adjustments | Increased fixed operational costs; reduced reimbursement rates |
| Technology Investment | Sequencing platform obsolescence; bioinformatics infrastructure; staff training | Significant capital outlay; ongoing maintenance costs |
| Supply Chain Management | Reagent costs; perishable inventory; group purchasing negotiations | Variable cost fluctuations; waste from expired materials |
| Reimbursement Landscape | Documentation requirements; medical necessity justification; coding accuracy | Claim denials; payment delays; revenue cycle disruption |
This technical guide provides a comprehensive cost-benefit analysis framework for clinical laboratories implementing metagenomic sequencing for bacterial identification. By examining direct and indirect costs, operational efficiencies, clinical benefits, and strategic implementation models, laboratories can develop data-driven approaches to maximize the value proposition of this transformative technology while maintaining fiscal sustainability.
Comprehensive Cost Analysis of Metagenomic Sequencing
Implementing mNGS in clinical laboratories requires careful consideration of both direct and indirect costs across the entire testing workflow. Understanding these cost components is essential for accurate financial modeling and resource allocation.
Direct Cost Components
The direct costs of mNGS testing encompass all expenses directly attributable to performing the test. Instrumentation and capital equipment represent significant initial investments, with Illumina sequencing platforms ranging from approximately $350,000 for the Sequel system to $985,000 for the NovaSeq 6000 [111]. These capital outlays must be amortized over the instrument's operational lifespan and factored into the cost per test. Consumables and reagents constitute recurring expenses that vary based on testing volume and platform selection. The ultra-rapid mNGS workflow described in recent literature utilizes specialized rapid reagent kits and cartridge-based point-of-care devices for automated nucleic acid extraction and library preparation [112]. Labor expenses account for the technical expertise required for complex workflows including sample preparation, library construction, sequencing operations, and bioinformatics analysis [10].
Table 2: Direct Cost Components for Metagenomic Sequencing Implementation
| Cost Category | Specific Components | Financial Considerations |
|---|---|---|
| Instrumentation | Sequencers; automated nucleic extraction systems; library preparation stations | High initial capital investment ($350,000-$985,000); service contracts; maintenance costs |
| Consumables & Reagents | Nucleic acid extraction kits; library preparation reagents; sequencing flow cells; purification beads | Volume-based pricing; group purchasing organization discounts; inventory carrying costs |
| Labor | Technical staff; bioinformaticians; molecular biologists; quality control personnel | Specialized expertise commands premium salaries; extensive training requirements; productivity metrics |
| Facility & Infrastructure | Dedicated laboratory space; climate control; uninterruptible power supply; data storage systems | Renovation costs for existing space; operational overhead allocation; computational infrastructure |
Recent studies demonstrate that strategic workflow modifications can significantly reduce direct costs. An ultra-rapid mNGS protocol implemented on the Illumina platform achieved a theoretical turnaround time of 7 hours through five key optimizations: (1) automation in nucleic acid extraction and library preparation using cartridge-based point-of-care devices; (2) PCR-free library preparation requiring only one nucleic acid purification step; (3) use of MiniSeq rapid reagent kits with reduced input requirements; (4) simplified sample pooling processes; and (5) optimized bioinformatics pipelines to reduce runtime [112]. This optimized workflow demonstrated a cost of approximately $100 per sample compared to $300 per sample for Nanopore-based mNGS, highlighting the significant cost savings possible through workflow optimization [112].
Indirect and Hidden Costs
Beyond direct expenses, laboratories must account for bioinformatics infrastructure and personnel costs, which include high-performance computing resources, data storage solutions, and specialized bioinformatics staff [10]. The volume of data generated by mNGS is substantial, with one human genome's sequencing resulting in approximately 743 terabytes of data as of 2017 [111]. Quality control and validation expenses encompass proficiency testing, validation studies, and ongoing quality monitoring required for Clinical Laboratory Improvement Amendments (CLIA) compliance [10] [110]. Administrative overhead includes test utilization management, billing and reimbursement activities, and regulatory compliance reporting [110].
Supply chain management represents another critical cost consideration, as materials typically constitute 15-40% of clinical laboratories' operational costs [113]. Effective inventory management of reagents, calibrators, and controls—many requiring specific environmental conditions like cold storage—is essential to minimize waste and prevent testing delays [113]. Laboratories must implement robust Logistic Management Information Systems (LMIS) to track material consumption, manage expiration dates, and optimize purchase orders [113].
Operational Efficiencies and Workflow Optimization
Strategic optimization of mNGS workflows can yield significant efficiencies that directly impact both operational costs and clinical utility. Laboratories can implement several evidence-based strategies to maximize throughput while minimizing resource utilization.
Turnaround Time Optimization
Reducing turnaround time (TAT) represents a critical efficiency target, particularly for severe infections where mortality increases by 7.6% for each hour of delay in appropriate antimicrobial therapy [112]. A landmark study demonstrated that an optimized ultra-rapid mNGS workflow achieved an average TAT of 10.53 hours (minimum 7.4 hours) compared to 97.72 hours for blood culture and 55.4 hours for routine mNGS [112]. This dramatic reduction was accomplished through a re-engineered workflow that incorporated automated nucleic acid extraction, PCR-free library preparation, rapid sequencing kits, and streamlined bioinformatics pipelines [112]. The operational benefits of reduced TAT extend beyond improved patient outcomes to include more efficient utilization of instrumentation, staff resources, and laboratory space.
Diagram 1: Ultra-Rapid mNGS Workflow (Theoretical TAT: 7 hours)
Test Utilization Management
Effective test utilization programs represent a crucial strategy for optimizing laboratory efficiency and controlling costs. Inappropriate testing has been documented in 43.9% of hospital laboratory tests at admission and 7.4% of subsequent testing [114]. Laboratories can establish Clinical Laboratory Utilization Committees comprising physicians, scientists, and IT specialists to govern test ordering patterns and eliminate unnecessary, obsolete, or duplicative testing [114]. Key utilization management strategies include: removing obsolete tests from laboratory menus; updating order sets to reflect current diagnostic best practices; implementing clinical decision support tools within electronic health records; and educating clinicians on appropriate test selection [114]. These approaches directly address the operational inefficiencies and resource waste associated with low-value testing.
Automation and Artificial Intelligence Integration
Laboratory automation and artificial intelligence (AI) present transformative opportunities for operational efficiency. Total laboratory automation (TLA) systems reduce labor costs, minimize human error, and standardize processing times [110]. Although requiring substantial initial investment, TLA delivers long-term gains in efficiency and reductions in TAT that justify the capital outlay [110]. AI-assisted metagenomic analysis leverages machine learning algorithms to enhance pathogen identification accuracy and speed while reducing bioinformatics personnel requirements [4]. The Taxon-aware Compositional Inference Network (TCINet), a deep learning model that processes sequencing reads to produce taxonomic embeddings, exemplifies how AI can improve analytical efficiency [4]. Potential AI use cases in clinical laboratories include: automated slide analysis in pathology; laboratory sample risk stratification; test result interpretation and reporting; equipment performance monitoring; and inventory management optimization [114].
Quantitative Cost-Benefit Analysis Framework
A rigorous cost-benefit analysis must quantify both the financial implications and clinical value of mNGS implementation to support informed decision-making.
Cost-Savings and Revenue Generation Models
Economic studies demonstrate that mNGS can generate significant cost savings through optimized antibiotic management. In a study of 36 ICU patients with sepsis, ultra-rapid mNGS testing resulted in antibiotic changes in 83% of cases, with a net reduction of 10,909.52 Chinese Yuan (~$1,558.50) across the cohort [112]. This reduction primarily resulted from de-escalation or discontinuation of unnecessary antibiotics, though some cases warranted additional antibiotics targeting identified pathogens not covered by empirical therapy [112]. The same study demonstrated that when mNGS validated empirical antibiotic therapy (39% of cases), the 30-day survival rate was 90%, significantly higher than for patients whose therapy was modified based on mNGS results [112].
Table 3: Antibiotic Cost Analysis Before and After Ultra-Rapid mNGS Implementation
| Cost Category | Pre-mNGS Implementation | Post-mNGS Implementation | Net Change |
|---|---|---|---|
| Empirical Antibiotic Costs | 15,322.64 CNY | 12,413.12 CNY | -2,909.52 CNY |
| Targeted Antibiotic Costs | Not applicable | 4,826.24 CNY | +4,826.24 CNY |
| Overall Antibiotic Expenditure | 15,322.64 CNY | 17,239.36 CNY | +1,916.72 CNY |
| Cases with Cost Reduction | Not applicable | 15 cases (41.7%) | -10,909.52 CNY total |
| Cases with Cost Increase | Not applicable | 5 cases (13.9%) | +1,413.12 CNY total |
A comprehensive cost-benefit analysis of mNGS for pyrexia of unknown origin (PUO) employed decision tree modeling to compare standard diagnostic workflows against strategies incorporating first-line or second-line mNGS testing [109]. This study concluded that mNGS as a second-line investigation was "effectively dominated" from a cost perspective, while first-line use required higher detection rates or lower costs than currently available to be justifiable as a pure cost-saving measure [109]. The analysis emphasized that mNGS should serve as a "supplement to rather than a replacement for careful clinical judgement" in specific contexts rather than widespread deployment [109].
Clinical Benefits and Operational Impact
The clinical benefits of mNGS extend beyond direct cost savings to encompass valuable but difficult-to-quantify operational improvements. Reduced length of stay represents a significant financial benefit, particularly for critically ill patients where diagnostic delays directly increase ICU days [114]. Improved antibiotic stewardship enhances patient outcomes while reducing the incidence of antimicrobial resistance and associated treatment costs [112] [10]. Outbreak management capabilities through rapid pathogen identification and transmission tracking prevent widespread healthcare-associated infections with their attendant costs [10]. Laboratories should develop metrics to capture these operational benefits, including time to appropriate therapy, antibiotic spectrum index, and test result impact on treatment decisions.
Implementation Roadmap and Strategic Considerations
Successful mNGS implementation requires a phased, strategic approach that aligns technological capabilities with clinical and operational needs.
Technology Selection and Validation
Laboratories must carefully evaluate sequencing platforms based on intended application volumes, performance requirements, and available expertise. Short-read technologies (Illumina) offer higher accuracy and lower per-sample costs ($100) for high-volume applications [112] [111]. Long-read technologies (Oxford Nanopore, PacBio) provide rapid turnaround times (6 hours) and portability at higher costs (~$300 per sample) [112] [10]. Implementation begins with analytical validation per CLIA and CAP requirements, establishing performance characteristics for precision, accuracy, reportable range, reference range, and sensitivity/specificity [10] [110]. Verification studies should use clinical samples with established comparator testing (culture, PCR, serology) across the intended specimen types and pathogen targets [27].
Financial Modeling and Reimbursement Strategy
Robust financial modeling must project operational costs, test volumes, and reimbursement rates under various adoption scenarios. Laboratories should analyze payer mix and reimbursement policies, as Medicare and private insurers increasingly link payment to demonstrated medical necessity and clinical utility [110]. Documentation requirements necessitate close collaboration with ordering physicians to ensure appropriate ICD-10 coding and supporting clinical information [110]. Claims management requires meticulous attention to CPT/HCPCS code assignment, local coverage determinations (LCDs), and denial management processes [110]. Proactive engagement with payers regarding the clinical and economic value proposition of mNGS for specific indications can facilitate appropriate coverage policies.
Diagram 2: mNGS Implementation Roadmap
Strategic Partnerships and Outsourcing Considerations
For many laboratories, a hybrid approach combining in-house testing with strategic outsourcing represents the most viable implementation model. Esoteric testing reference laboratories offer expertise for low-volume, complex analyses that may not justify full in-house implementation [114]. Bioinformatics partnerships with specialized providers can overcome computational infrastructure and personnel challenges [10]. Research collaborations with academic institutions facilitate access to emerging technologies and expertise while distributing development costs [115]. Laboratories should conduct make-versus-buy analyses based on test volumes, available expertise, and capital resources to determine the optimal implementation model.
Essential Research Reagents and Materials
The successful implementation of mNGS for bacterial identification requires specific research-grade reagents and materials that ensure reproducibility, accuracy, and compliance with regulatory standards.
Table 4: Essential Research Reagent Solutions for Metagenomic Sequencing
| Reagent Category | Specific Examples | Function and Importance |
|---|---|---|
| Nucleic Acid Extraction Kits | Automated cartridge-based systems; magnetic bead-based purification | Ensure representative recovery of microbial DNA; minimize contamination; maintain nucleic acid integrity for sequencing [112] |
| Library Preparation Reagents | PCR-free library kits; enzymatic fragmentation mixes; end repair, dA-tailing, and adaptor ligation modules | Create sequencing libraries while maintaining quantitative microbial representation; reduce bias from amplification [112] [10] |
| Sequencing Consumables | MiniSeq rapid reagent kits; flow cells; buffer solutions | Enable high-throughput sequencing; impact read length, accuracy, and overall data quality [112] |
| Quality Control Materials | Quantitative standards (Qubit); fragment analyzers (Bioanalyzer); internal control pathogens | Verify nucleic acid quantity, library size distribution, and process efficiency; ensure analytical sensitivity [27] |
| Bioinformatics Tools | Kraken2; MetaPhlAn; PathoScope; One Codex; custom AI algorithms | Perform taxonomic classification, antimicrobial resistance detection, and phylogenetic analysis [10] [4] |
Metagenomic sequencing represents a transformative diagnostic technology with the potential to revolutionize infectious disease diagnosis and management. However, its economic viability depends on rigorous cost-benefit analysis and strategic implementation that aligns with clinical needs and operational realities. Laboratories must consider the total cost of ownership, including direct expenses, infrastructure requirements, and personnel costs, while accurately quantifying the clinical and operational benefits through improved patient outcomes, antibiotic stewardship, and outbreak management. A phased implementation approach with careful attention to test utilization, workflow optimization, and reimbursement strategy provides the framework for sustainable integration of this powerful technology into clinical practice. As sequencing costs continue to decline and bioinformatics tools become more sophisticated and accessible, metagenomic sequencing is poised to transition from specialized reference testing to routine clinical application, fundamentally enhancing our ability to diagnose and manage infectious diseases.
The accurate identification of bacterial pathogens is a cornerstone of effective infectious disease management. Metagenomic next-generation sequencing (mNGS) has emerged as a transformative, hypothesis-free tool that enables simultaneous detection of a broad array of pathogens—including bacteria, viruses, fungi, and parasites—directly from clinical specimens such as cerebrospinal fluid, blood, and bronchoalveolar lavage fluid [10]. Unlike traditional culture and targeted molecular assays, mNGS serves as a powerful complementary approach, capable of identifying novel, fastidious, and polymicrobial infections while also characterizing antimicrobial resistance genes [10]. These advantages are particularly relevant in diagnostically challenging scenarios, such as infections in immunocompromised patients, sepsis, and culture-negative cases.
Within this context, understanding the performance characteristics of mNGS and related diagnostic methods requires a firm grasp of sensitivity, specificity, and predictive values. These metrics provide the statistical foundation for evaluating diagnostic tests and guide appropriate clinical interpretation [116] [117]. Sensitivity represents the proportion of true positives a test correctly identifies from all patients with a condition, while specificity indicates the proportion of true negatives correctly identified from all patients without the condition [116]. For clinical researchers working with mNGS data, properly calculating and interpreting these parameters is essential for validating methods, comparing technological approaches, and translating findings into clinically actionable results.
Foundational Principles of Sensitivity and Specificity
Definitions and Calculations
Sensitivity and specificity are essential indicators of test accuracy that allow healthcare providers and researchers to determine the appropriateness of a diagnostic tool [116]. These metrics are defined according to standard formulas based on a 2x2 contingency table that compares test results against a reference standard:
- Sensitivity = True Positives / (True Positives + False Negatives)
- Specificity = True Negatives / (True Negatives + False Positives) [116]
Sensitivity reflects a test's ability to correctly identify individuals who have a disease, while specificity indicates its ability to correctly identify those who do not have the disease [117]. In practical terms, a highly sensitive test is valuable for ruling out disease when negative (often summarized as "SnNout"), whereas a highly specific test is valuable for ruling in disease when positive ("SpPin") [116].
Relationship to Predictive Values
While sensitivity and specificity describe inherent test characteristics, positive and negative predictive values (PPV and NPV) indicate the probability that a test result correctly reflects the true disease status in a specific population [117]. These metrics are calculated as follows:
- Positive Predictive Value (PPV) = True Positives / (True Positives + False Positives)
- Negative Predictive Value (NPV) = True Negatives / (True Negatives + False Negatives) [116]
A critical distinction is that predictive values are strongly influenced by disease prevalence in the population being tested, whereas sensitivity and specificity are generally considered stable test characteristics [118]. As disease prevalence increases, PPV increases while NPV decreases, meaning the same test will perform differently in primary care settings (lower prevalence) versus hospital settings (higher prevalence) [119] [118].
Visualizing Diagnostic Test Accuracy Relationships
The following diagram illustrates the logical relationships between the core concepts of diagnostic test accuracy and how they are derived from a 2x2 contingency table:
Performance Variation Across Healthcare Settings
Meta-Epidemiological Evidence
Diagnostic test accuracy may vary substantially among healthcare settings, which among other reasons may be due to referral from primary to secondary care [119]. A recent meta-epidemiological study analyzing nine systematic reviews evaluating thirteen different diagnostic tests found that sensitivity and specificity vary in both direction and magnitude between nonreferred and referred settings, depending on the test and target condition, with no universal patterns governing performance differences [119].
For signs and symptoms (seven tests), the differences in sensitivity and specificity between settings ranged from +0.03 to +0.30 and from -0.12 to +0.03, respectively. For biomarkers (four tests), differences in sensitivity ranged from -0.11 to +0.21 and specificity from -0.01 to -0.19. Differences in sensitivity and specificity for one questionnaire test were +0.1 and -0.07 respectively, and for one imaging test were -0.22 and -0.07 [119]. These findings highlight the importance of considering the clinical setting when interpreting diagnostic accuracy studies.
Implications for Test Selection and Interpretation
The variation in test performance across settings has important implications for both research and clinical practice. Differences in sensitivity were generally larger than those in specificity, suggesting that setting-specific factors may particularly affect a test's ability to detect true cases [119]. Sensitivity analyses limited to countries with gatekeeping health care systems produced similar results, indicating that these patterns are robust across different healthcare organizational structures [119].
The following diagram illustrates how diagnostic test performance varies across clinical settings and impacts interpretation:
Comparative Performance of Metagenomic Sequencing Technologies
Methodologies for Lower Respiratory Infection Diagnostics
Recent advances in next-generation sequencing have created both opportunities and challenges for clinical diagnostics, as numerous platforms and approaches are now available. A 2025 study directly compared the diagnostic performance of metagenomic NGS (mNGS) and two targeted NGS (tNGS) approaches—amplification-based tNGS and capture-based tNGS—for lower respiratory tract infections [93]. The study included 205 patients with suspected lower respiratory tract infections from the department of respiratory and critical care medicine, and collected their lower respiratory tract samples for parallel testing using all three methods.
The methodological approaches for each technology were as follows:
mNGS: DNA was extracted from 1 mL BALF samples using a QIAamp UCP Pathogen DNA Kit with human DNA removal using Benzonase and Tween20. RNA was extracted using the QIAamp Viral RNA Kit, with ribosomal RNA removed using a Ribo-Zero rRNA Removal Kit. Following library construction using Ovation Ultralow System V2, sequencing was executed on Illumina Nextseq 550Dx with 75-bp single-end reads, generating approximately 20 million reads per sample [93].
Amplification-based tNGS: Used the Respiratory Pathogen Detection Kit with a set of 198 microorganism-specific primers selected for ultra-multiplex PCR amplification to enrich target pathogen sequences. The library was sequenced on an Illumina MiniSeq platform with each library yielding approximately 0.1 million reads of single-end 100 bp length [93].
Capture-based tNGS: Employed probe capture techniques to enrich specific genetic targets, with sequencing performed to identify pathogens along with genotypes, antimicrobial resistance genes, and virulence factors [93].
Quantitative Performance Comparison
Table 1: Comparative Performance of NGS Methodologies in Lower Respiratory Infection Diagnosis
| Performance Metric | mNGS | Amplification-based tNGS | Capture-based tNGS |
|---|---|---|---|
| Cost per sample | $840 | Not specified | Not specified |
| Turnaround time | 20 hours | Not specified | Not specified |
| Number of species identified | 80 species | 65 species | 71 species |
| Accuracy | Not specified | Not specified | 93.17% |
| Sensitivity | Not specified | Not specified | 99.43% |
| Specificity for DNA viruses | Not specified | 98.25% | 74.78% |
| Sensitivity for gram-positive bacteria | Not specified | 40.23% | Not specified |
| Sensitivity for gram-negative bacteria | Not specified | 71.74% | Not specified |
The performance data reveal distinct strengths and limitations for each approach. The capture-based tNGS demonstrated significantly higher diagnostic performance than the other two NGS methods, with an accuracy of 93.17% and a sensitivity of 99.43% when benchmarked against comprehensive clinical diagnosis [93]. However, it showed lower specificity compared to the amplification-based tNGS in identifying DNA viruses (74.78% vs. 98.25%) [93]. The amplification-based tNGS exhibited poor sensitivity for both gram-positive (40.23%) and gram-negative bacteria (71.74%) [93].
Performance in Strain-Level Characterization
Moving beyond species identification, strain-level characterization of bacterial pathogens has emerged as a critical requirement for understanding virulence and antimicrobial resistance profiles. A 2025 study evaluating strain-level characterization of bacterial pathogens using metagenomic sequencing for patients with pneumonia demonstrated that mNGS could achieve strain-level resolution comparable to culture-based methods [120]. The research found that co-infections at the clonal complex level were detected in 5.40% of Acinetobacter baumannii-positive and 19.55% of Klebsiella pneumoniae-positive bronchoalveolar lavage fluid specimens [120]. Antimicrobial resistance profiles remained constant for patients with single infections but varied for those with co-infection, highlighting the clinical importance of strain-level differentiation [120].
Benchmarking Metagenomic Tools for Pathogen Detection
Experimental Design for Tool Evaluation
Robust benchmarking of bioinformatic tools is essential for establishing reliable metagenomic workflows. A recent study evaluated the performance of four metagenomic classification tools—Kraken2, Kraken2/Bracken, MetaPhlAn4, and Centrifuge—for detecting foodborne pathogens in simulated microbial communities representing three food products [121]. The experimental protocol involved:
- Sample Preparation: Metagenomes were simulated to include specific pathogens (Campylobacter jejuni, Cronobacter sakazakii, and Listeria monocytogenes) at defined relative abundance levels (0%-control, 0.01%, 0.1%, 1%, and 30%) within food-specific microbiomes.
- Matrix Variation: Three different food matrices (chicken meat, dried food, and milk products) were evaluated to assess performance across different microbial backgrounds.
- Performance Metrics: Tools were evaluated based on classification accuracy and F1-scores (which balance precision and recall) across the various abundance levels and food matrices [121].
Comparative Tool Performance
Table 2: Performance Benchmarking of Metagenomic Classification Tools
| Tool | Overall Accuracy | Detection Limit | Strengths | Limitations |
|---|---|---|---|---|
| Kraken2/Bracken | Highest classification accuracy, consistently high F1-scores across all food metagenomes | 0.01% | Broadest detection range, effective across diverse matrices | Not specified |
| Kraken2 | High performance | 0.01% | Broad detection range | Slightly lower accuracy than Kraken2/Bracken |
| MetaPhlAn4 | Good performance | Limited at 0.01% level | Valuable for specific applications, well-suited for C. sakazakii in dried food | Limited detection at lowest abundance level (0.01%) |
| Centrifuge | Weakest performance | Higher limit of detection | Not specified | Underperformed across food matrices and abundance levels |
The benchmarking results demonstrated that Kraken2/Bracken achieved the highest classification accuracy, with consistently higher F1-scores across all food metagenomes, whereas Centrifuge exhibited the weakest performance [121]. Kraken2/Bracken and Kraken2 exhibited the broadest detection range, correctly identifying pathogen sequence reads down to the 0.01% level, whereas MetaPhlAn4 and Centrifuge had higher limits of detection [121]. These findings provide crucial insights for selecting appropriate metagenomic tools based on required sensitivity and the expected abundance of target pathogens in specific clinical or public health applications.
Essential Research Reagents and Materials
The implementation of metagenomic sequencing workflows requires specific research reagents and materials that are critical for achieving optimal sensitivity and specificity. The following table details key components used in the featured studies:
Table 3: Essential Research Reagent Solutions for Metagenomic Sequencing
| Reagent/Material | Function | Example Products |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of microbial DNA/RNA from clinical samples | QIAamp UCP Pathogen DNA Kit, MagPure Pathogen DNA/RNA Kit, Tiangen NG550 kit |
| Host DNA Depletion Reagents | Reduce human background to improve pathogen detection sensitivity | Benzonase, Tween20, GensKey Host DNA Depletion Kit, saponin-based differential lysis |
| Library Preparation Kits | Prepare nucleic acids for sequencing by adding adapters and barcodes | Ovation Ultrolow System V2, ONT Rapid PCR Barcoding Kit |
| Target Enrichment Systems | Enrich pathogen sequences in tNGS approaches | Respiratory Pathogen Detection Kit (amplification-based), Probe capture panels |
| Sequencing Platforms | Generate sequence data from prepared libraries | Illumina NextSeq 550Dx, Illumina MiniSeq, Oxford Nanopore GridION X5 |
| Bioinformatic Tools | Analyze sequence data for pathogen identification and characterization | Kraken2/Bracken, MetaPhlAn4, Centrifuge, MIST software, PathoScope, One Codex |
| Reference Databases | Provide taxonomic framework for classifying sequences | NCBI nt and RefSeq, CARD (Comprehensive Antibiotic Resistance Database), FDA-ARGOS |
Sensitivity and specificity metrics provide essential frameworks for evaluating the performance of metagenomic sequencing technologies in bacterial identification research. The evidence demonstrates that test accuracy varies substantially across healthcare settings, with differences in both direction and magnitude depending on the specific test and target condition [119]. Recent comparative studies of mNGS and tNGS methods reveal distinct performance profiles, with capture-based tNGS offering superior sensitivity (99.43%) and overall accuracy (93.17%) for routine diagnostic testing, while amplification-based tNGS provides higher specificity for DNA viruses (98.25%), and mNGS remains valuable for detecting rare pathogens [93].
For researchers implementing these technologies, careful selection of bioinformatic tools is crucial, with benchmarking studies indicating that Kraken2/Bracken achieves the highest classification accuracy for pathogen detection [121]. As the field advances toward strain-level resolution, proper interpretation of sensitivity and specificity data will continue to play a vital role in validating new methodologies and translating mNGS into improved patient care across diverse clinical settings.
Conclusion
Metagenomic next-generation sequencing represents a paradigm shift in bacterial identification, offering unprecedented breadth and speed for pathogen detection. By moving beyond the limitations of culture, mNGS empowers researchers and drug developers to uncover complex polymicrobial infections, detect elusive pathogens, and rapidly characterize antimicrobial resistance profiles. While challenges in standardization, cost, and data interpretation persist, ongoing advancements in host depletion, bioinformatics, and portable sequencing technologies are paving the way for its integration into routine clinical practice. The future of mNGS lies in its convergence with artificial intelligence for automated analysis, its application in real-time outbreak surveillance, and its role in guiding targeted antibiotic therapies, ultimately contributing to improved patient outcomes and strengthened antimicrobial stewardship on a global scale.
References
- 1. Application of metagenomic next-generation sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11604630/]
- 2. Metagenomic Next Generation Sequencing: How Does It ... [https://asm.org/articles/2019/november/metagenomic-next-generation-sequencing-how-does-it]
- 3. Clinical metagenomic sequencing [https://en.wikipedia.org/wiki/Clinical_metagenomic_sequencing]
- 4. Enhancing pathogen identification through AI-assisted ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1634194/full]
- 5. Metagenomic Next-Generation Sequencing in Infectious ... [https://pubmed.ncbi.nlm.nih.gov/40870843/]
- 6. Metagenomic Next-Generation Sequencing - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/metagenomic-next-generation-sequencing]
- 7. Recommendations for the introduction of metagenomic ... [https://www.sciencedirect.com/science/article/pii/S1386653220304339]
- 8. Application of metagenomic next-generation sequencing ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1439472/full]
- 9. Genome-resolved metagenomics: a game changer for ... [https://www.nature.com/articles/s12276-024-01262-7]
- 10. Metagenomic Next-Generation Sequencing in Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384723/]
- 11. Metagenomics Next Generation Sequencing (mNGS) [https://pmc.ncbi.nlm.nih.gov/articles/PMC9699264/]
- 12. Diagnostic value of metagenomic next-generation ... [https://www.nature.com/articles/s41598-025-23695-4]
- 13. How Pathogen MNGS Detection Works — In One Simple ... [https://www.linkedin.com/pulse/how-pathogen-mngs-detection-works-one-simple-flow-2025-qokac]
- 14. Metagenomic next-generation sequencing for concurrent ... [https://www.nature.com/articles/s41598-025-18812-2]
- 15. Rapid metagenomic sequencing for surveillance of ... [https://nanoporetech.com/document/rapid-sequencing-metagenomics-sqk-rpb114-24]
- 16. Guide to mNGS Data Analysis [https://chanzuckerberg.zendesk.com/hc/en-us/articles/13770737266196-Guide-to-mNGS-Data-Analysis]
- 17. Metagenomics: Application of Genomics to Uncultured ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC539003/]
- 18. Shotgun Metagenomic Sequencing [https://www.illumina.com/areas-of-interest/microbiology/microbial-sequencing-methods/shotgun-metagenomic-sequencing.html]
- 19. Comparison of metagenomic next-generation sequencing and ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09236-w]
- 20. Advantages and challenges of metagenomic sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9527156/]
- 21. Metagenomic applications in exploration and development ... [https://www.sciencedirect.com/science/article/pii/S1687157X23005607]
- 22. Unified metagenomic method for rapid detection of ... [https://www.nature.com/articles/s43856-024-00554-3]
- 23. Metagenomics-enabled microbial surveillance [https://www.nature.com/articles/s41564-022-01089-w]
- 24. A 'Culture' Shift: Application of Molecular Techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6447436/]
- 25. Polymicrobial Infections: A Comprehensive Review on ... [https://www.mdpi.com/2813-9054/70/4/39]
- 26. Application of metagenomic next-generation sequencing ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1382635/full]
- 27. Metagenomic next-generation sequencing reveals ... [https://www.nature.com/articles/s41598-025-21722-y]
- 28. 16S and ITS rRNA Sequencing | Identify bacteria & fungi ... [https://www.illumina.com/areas-of-interest/microbiology/microbial-sequencing-methods/16s-rrna-sequencing.html]
- 29. Taxonomic Profiling and Visualization of Metagenomic Data [https://training.galaxyproject.org/training-material/topics/microbiome/tutorials/taxonomic-profiling/tutorial.html]
- 30. Polymicrobial infections and microbial patterns in infected ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-05386-9]
- 31. Microbial Sequencing | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/sequencing/dna-sequencing/microbial-sequencing.html]
- 32. MiSeq Sequencing System specifications [https://www.illumina.com/systems/sequencing-platforms/miseq/specifications.html]
- 33. NovaSeq 6000 Sequencing System specifications [https://www.illumina.com/systems/sequencing-platforms/novaseq/specifications.html]
- 34. Sequencing Platforms | Illumina NGS platforms [https://www.illumina.com/systems/sequencing-platforms.html]
- 35. Nanopore sequencing accuracy [https://nanoporetech.com/platform/accuracy]
- 36. Data analysis [https://nanoporetech.com/document/data-analysis]
- 37. Technology Platforms - BGI Americas [https://bgiamericas.com/technologies/technology-platforms/]
- 38. Workflow overview: pathogen metagenomics [https://nanoporetech.com/resource-centre/workflow-pathogen-metagenomics]
- 39. Wet Lab Protocols Matter: Choice of DNA Extraction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550470/]
- 40. Adaptive sampling: redefining targeted sequencing [https://nanoporetech.com/blog/adaptive-sampling-redefining-targeted-sequencing]
- 41. Benchmarking Metagenomics Tools for Taxonomic Classification - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6716367/]
- 42. Data Processing and Visualization for Metagenomics [https://gwu-libraries.github.io/metagenomics-analysis/aio/index.html]
- 43. Metagenomic Sequencing: Strategies for Host DNA Removal [https://www.cd-genomics.com/microbioseq/resource-metagenomic-sequencing-host-dna-removal.html]
- 44. Sequence analysis / Quality Control / Hands-on [https://training.galaxyproject.org/training-material/topics/sequence-analysis/tutorials/quality-control/tutorial.html]
- 45. How-to: NGS Quality Control [https://frontlinegenomics.com/how-to-ngs-quality-control/]
- 46. Whole Genome Sequencing (WGS) Quality Control (QC) ... [https://www.ga4gh.org/news_item/whole-genome-sequencing-wgs-quality-control-qc-standards-approved-as-an-official-ga4gh-product/]
- 47. HoCoRT: host contamination removal tool | BMC Bioinformatics [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05492-w]
- 48. Pangenome databases improve host removal and mycobacteria classification from clinical metagenomic data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10993716/]
- 49. Benchmarking bacterial taxonomic classification using ... [https://www.nature.com/articles/s41597-024-03672-8]
- 50. CCMetagen: comprehensive and accurate identification of eukaryotes and prokaryotes in metagenomic data | Genome Biology | Full Text [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-020-02014-2]
- 51. Clinical applications of metagenomics next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11199093/]
- 52. Clinical metagenomics | Nature Reviews Genetics [https://www.nature.com/articles/s41576-019-0113-7]
- 53. Diagnostic performance and clinical utility of metagenomic ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1612628/full]
- 54. Distribution Patterns of Pathogens Causing Lower ... [https://pubmed.ncbi.nlm.nih.gov/37840830]
- 55. Clinical utility of metagenomic next-generation sequencing ... [https://www.nature.com/articles/s41598-025-03564-w]
- 56. Nanopore targeted sequencing in lower respiratory infections [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634536/]
- 57. The prospects and challenge of pathogen diagnosis ... [https://www.pneumon.org/The-prospects-and-challenge-of-pathogen-diagnosis-nof-lower-respiratory-tract-infections,207844,0,2.html]
- 58. Beyond the Resistome: Molecular Insights, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561093/]
- 59. Metagenomics as a Transformative Tool for Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939754/]
- 60. Metagenomic Approaches to Analyze Antimicrobial ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.575592/full]
- 61. Beyond clinical genomics: addressing critical gaps in One ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1596720/full]
- 62. Metagenomic insights into resistance trends related to ... [https://www.nature.com/articles/s41598-025-06125-3]
- 63. Benefits and challenges of host depletion methods in ... [https://www.nature.com/articles/s41522-025-00762-2]
- 64. Host DNA depletion on frozen human respiratory samples ... [https://www.nature.com/articles/s42003-024-07290-3]
- 65. Improving saliva shotgun metagenomics by chemical host ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-018-0426-3]
- 66. Human and Extracellular DNA Depletion for Metagenomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6435281/]
- 67. Optimization of Metagenomic Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436562/]
- 68. Advances in Host Depletion and Pathogen Enrichment ... [https://www.sciencedirect.com/science/article/pii/S1525157824001284]
- 69. Get to know Novogene's Metagenomics Host DNA ... [https://www.rapidmicrobiology.com/news/learn-about-novogene-s-metagenomics-host-dna-removal-service]
- 70. Host DNA depletion assisted metagenomic sequencing of ... [https://ann-clinmicrob.biomedcentral.com/articles/10.1186/s12941-025-00782-y]
- 71. Evaluating urine volume and host depletion methods to ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-025-02191-x]
- 72. Host DNA depletion methods and genome-centric ... [https://pubmed.ncbi.nlm.nih.gov/38054728/]
- 73. Clinical Metagenomic Next-Generation Sequencing for Pathogen Detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6345613/]
- 74. A Bioinformatician's Guide to Metagenomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2593568/]
- 75. Simple statistical identification and removal of contaminant sequences in marker-gene and metagenomics data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6298009/]
- 76. Removal of false positives in metagenomics-based taxonomy profiling via targeting Type IIB restriction sites | Nature Communications [https://www.nature.com/articles/s41467-023-41099-8]
- 77. Investigating bacterial evolution in nature with metagenomics [https://www.sciencedirect.com/science/article/pii/S1369527425000761]
- 78. MetaBIDx: a new computational approach to bacteria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11149084/]
- 79. Rescuing Your Failed Libraries: A Guide to Ugly Electropherograms and What They Mean [https://www.yeasenbio.com/blogs/ngs/rescuing-your-failed-libraries-a-guide-to-ugly-electropherograms-and-what-they-mean]
- 80. NGS Library Preparation Support—Troubleshooting | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-library-preparation-support/ngs-library-preparation-support-troubleshooting.html]
- 81. Best practices for library quantification [https://knowledge.illumina.com/library-preparation/general/library-preparation-general-reference_material-list/000003750]
- 82. 高质量临床微生物基因组参考数据库构建的思考 [http://m.anytesting.com/news/1947514.html]
- 83. Taxonomic annotation errors incorrectly assign the family ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6044269/]
- 84. Deciphering the impact of contaminating microbiota in DNA ... [https://pubmed.ncbi.nlm.nih.gov/40833093/]
- 85. A metagenomic DNA sequencing assay that is robust ... [https://www.nature.com/articles/s41467-022-31654-0]
- 86. Using strain-resolved analysis to identify contamination in ... [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-023-01477-2]
- 87. Understanding the Promises and Hurdles of Metagenomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7108102/]
- 88. Experience of implementing metagenomic next-generation ... [https://www.nature.com/articles/s41598-025-94840-2]
- 89. Introduction to Pathogens - Molecular Biology of the Cell - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK26917/]
- 90. Key Insights from ESCMID 2025: Advancing Metagenomic ... [https://www.vhbio.com/escmid-2025-advancing-metagenomic-sequencing-clinical-practice/]
- 91. Comparison and evaluation of metagenomic next- ... [https://pubmed.ncbi.nlm.nih.gov/41278471/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1la0KilYwPOIHwB56heywdlTzelVn0d6mssNYq6ylj3TKxDMFC&fc=None&ff=20251124145530&v=2.18.0.post22+67771e2]
- 92. Comparison and evaluation of metagenomic next- ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1694179/full]
- 93. Comparative diagnostic performance of metagenomic and ... [https://www.nature.com/articles/s41598-025-11834-w]
- 94. Comparative Diagnostic Accuracy of Metagenomic Next ... [https://www.sciencedirect.com/science/article/pii/S0163445325002610]
- 95. Microbial culture vs. mNGS: diagnostic variations in ... [https://pubmed.ncbi.nlm.nih.gov/41230408/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=10MSL6XygFtCE0XpaQpog-pEt8342fXkY9lzrR7q6H0wVRyEa2&fc=None&ff=20251113222640&v=2.18.0.post22+67771e2]
- 96. Diagnostic value of metagenomic next generation ... [https://pubmed.ncbi.nlm.nih.gov/41036230/]
- 97. Comparison of pathogen detection performance between ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1563962/full]
- 98. Clinical application of metagenomic next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631761/]
- 99. A retrospective analysis comparing metagenomic next- ... [https://pubmed.ncbi.nlm.nih.gov/40264936/]
- 100. Clinical diagnostic value of metagenomic next-generation ... [https://www.sciencedirect.com/science/article/pii/S2405844024118336]
- 101. Clinical application of metagenomic next-generation ... [https://pubmed.ncbi.nlm.nih.gov/40357399/]
- 102. Unbiased DNA pathogen detection in tissues: Real-world ... [https://www.sciencedirect.com/science/article/pii/S0023683725001643]
- 103. Comparative analysis of metagenomic next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934473/]
- 104. Comparative of metagenomic and targeted next-generation ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1534519/full]
- 105. Microbial culture vs. mNGS: diagnostic variations in ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1611332/full]
- 106. Metagenomic next-generation sequencing (mNGS) guides ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570565/]
- 107. Metagenomic identification of pathogens and antimicrobial- ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2023.1283094/full]
- 108. Unveiling the Future of Infective Endocarditis Diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373624/]
- 109. Cost-benefit analysis of introducing next-generation ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0194648]
- 110. Cost Control and Reimbursement Challenges in Clinical ... [https://www.labmanager.com/cost-control-and-reimbursement-challenges-in-clinical-labs-34599]
- 111. Metagenomic Sequencing Market Size 2025 to 2034 [https://www.precedenceresearch.com/metagenomic-sequencing-market]
- 112. Clinical and cost analysis of an ultra-rapid metagenomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077567/]
- 113. Role of Supply Chain Management in Clinical Laboratory [https://pmc.ncbi.nlm.nih.gov/articles/PMC10784235/]
- 114. A Roadmap to Improving Efficiencies and Removing Costs ... [https://www.vizientinc.com/insights/blogs/2023/a-roadmap-to-improving-efficiencies-and-removing-costs-at-hospital-labs]
- 115. Metagenomics Global Market Research Report 2025-2030 [https://www.globenewswire.com/news-release/2025/11/03/3179165/28124/en/Metagenomics-Global-Market-Research-Report-2025-2030-New-Diagnostic-Approaches-Aging-Populations-Advancements-in-Known-and-Emerging-Biomarkers-and-Accelerated-Research-Growth.html]
- 116. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 117. , Sensitivity , and Predictive Values: Foundations... Specificity [https://pmc.ncbi.nlm.nih.gov/articles/PMC5701930/]
- 118. Making Sense of Sensitivity , Specificity and Predictive Value... [https://blogs.imperial.ac.uk/medical-centre/2023/10/10/making-sense-of-sensitivity-specificity-and-predictive-value-a-guide-for-patients-clinicians-and-policymakers/]
- 119. Variation in sensitivity and specificity of diverse diagnostic ... [https://www.sciencedirect.com/science/article/pii/S0895435625001490]
- 120. Strain-level characterization of bacterial pathogens using ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07134-6]
- 121. Benchmarking Metagenomic Pipelines for the Detection of ... [https://www.sciencedirect.com/science/article/pii/S0362028X25001358]