From Bacterial Defense to Genetic Scalpel: The Complete History and Clinical Transformation of CRISPR
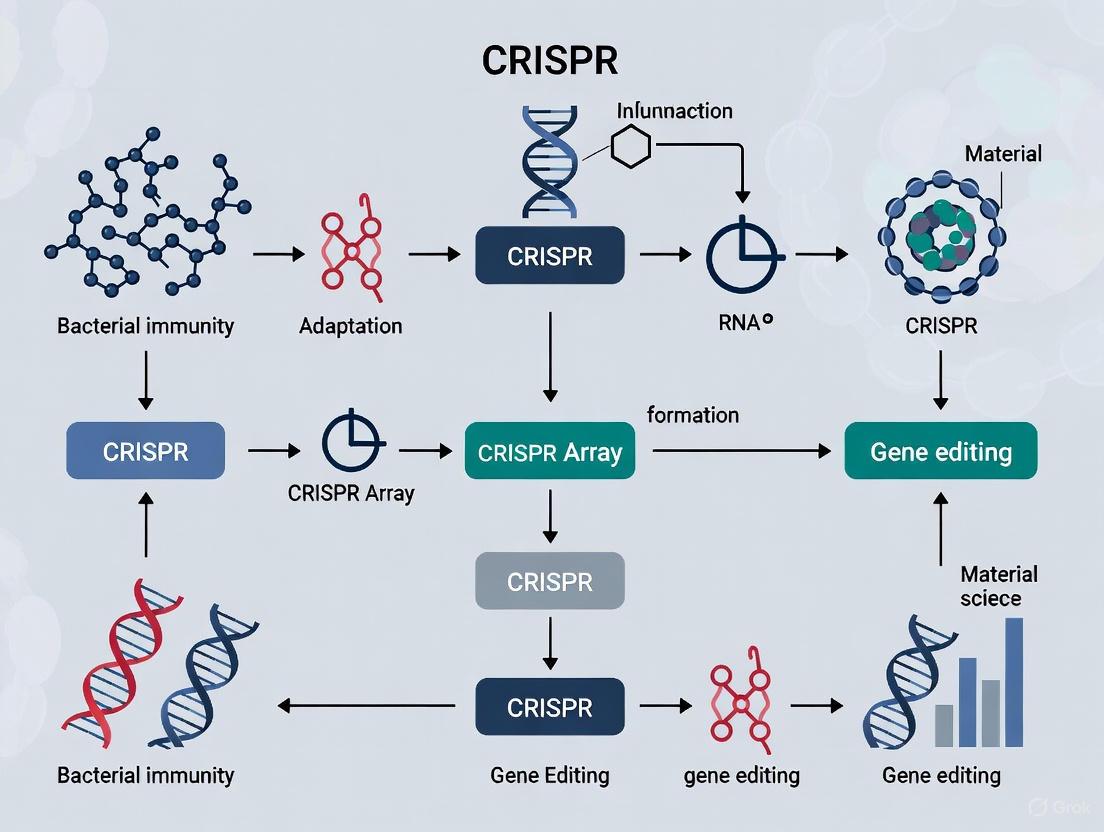
This article traces the remarkable journey of CRISPR-Cas systems from their initial discovery as a bacterial immune mechanism to their current status as a transformative technology in biomedicine.
From Bacterial Defense to Genetic Scalpel: The Complete History and Clinical Transformation of CRISPR
Abstract
This article traces the remarkable journey of CRISPR-Cas systems from their initial discovery as a bacterial immune mechanism to their current status as a transformative technology in biomedicine. We explore the foundational biology of CRISPR, detailing key discoveries from 1987 to the 2012 demonstration of programmable DNA cleavage. The review then examines the methodological leap to therapeutic applications, including the first FDA-approved CRISPR therapy and over 150 active clinical trials as of 2025. Critical analysis addresses persistent challenges like off-target effects and structural variations, while comparing CRISPR to alternative editing platforms. Designed for researchers and drug development professionals, this synthesis provides a comprehensive resource on the evolution, current landscape, and future trajectory of genome editing.
The Natural Blueprint: Decoding CRISPR as a Prokaryotic Immune System
In the mid-1980s, a fundamental research project on bacterial metabolism unexpectedly led to the first documented encounter with what would later be recognized as the CRISPR-Cas system. This discovery occurred not through targeted investigation of immune mechanisms, but rather during routine analysis of the iap gene (involved in isozyme conversion of alkaline phosphatase) in Escherichia coli [1] [2]. Yoshizumi Ishino and his team at Osaka University, while sequencing a 1.7-kbp DNA fragment spanning the iap gene region, stumbled upon an unusual set of repeated sequences in the 3' flanking region of the gene [1] [3] [2]. At the time, the scientific significance of these repeats was not understood, and their function remained enigmatic for nearly two decades. This initial finding marked the beginning of a long scientific journey that would ultimately revolutionize the field of genetics and genome engineering. The mysterious repeated sequence represented the first glimpse of a sophisticated adaptive immune system in prokaryotes, though its full implications would not be realized until the genomics era provided the necessary context and tools for functional analysis.
The 1987 Discovery: Technical Breakdown
Experimental Methodology and Technical Challenges
The discovery was made using the dideoxy sequencing method (Sanger sequencing), which was state-of-the-art in the mid-1980s [1]. The technical process involved several complex steps that presented significant challenges:
- Template Preparation: The target DNA fragment had to be cloned into M13 vectors to produce single-stranded template DNA for sequencing reactions [1].
- Sequencing Reaction: The chain termination reaction was performed using the Klenow fragment of E. coli polymerase I at 37°C, with reaction products labeled by incorporation of [α32P]dATP [1].
- Sequence Analysis: Sequence ladder images were obtained through autoradiography, requiring manual reading and interpretation [1].
The palindromic nature of the repeated sequences caused particular difficulties. The secondary structure formation led to nonspecific termination of the dideoxynucleotide incorporation reactions, making precise sequence reading exceptionally challenging [1]. This technical hurdle required months of painstaking work to precisely determine the sequence of what we now recognize as the CRISPR region—a task that contemporary technology can accomplish in a single day [1].
Structural Characteristics of the Discovered Repeats
Ishino and colleagues documented a unique arrangement of five highly homologous sequences of 29 nucleotides, arranged as direct repeats and separated by non-repetitive spacer sequences of 32 nucleotides [1] [2]. The key structural features included:
Table 1: Structural Characteristics of the Discovered Repeats in E. coli
| Feature | Description | Significance |
|---|---|---|
| Repeat Length | 29 nucleotides | Unusual length for repetitive sequences |
| Spacer Length | 32 nucleotides | Variable sequences between repeats |
| Arrangement | 5 direct repeats with regular spacing | Distinct from typical tandem repeats |
| Palindromic Nature | Dyad symmetry within repeats | Potential for secondary structure formation |
| Genomic Location | 3' flanking region of iap gene | Located in intergenic space |
The researchers noted that these sequences showed no similarity to previously identified Repetitive Extragenic Palindromic (REP) sequences, indicating they had encountered a fundamentally new type of genetic element [1]. The repeats contained a dyad symmetry of 14 bp, suggesting potential to form stable secondary structures that might have functional significance [1].
Research Reagent Solutions
Table 2: Key Research Reagents and Methods in the 1987 Discovery
| Reagent/Method | Function/Application | Context in 1987 Study |
|---|---|---|
| M13 Vectors (mp18/mp19) | Production of single-stranded DNA templates | Essential for dideoxy sequencing methodology |
| Klenow Fragment | DNA polymerase for dideoxy sequencing | Catalyzed chain termination reactions |
| [α32P]dATP | Radioactive labeling of DNA | Enabled visualization of sequence ladders |
| Alkaline Phosphatase (iap) Gene | Target gene for initial study | Served as reference point for unexpected discovery |
| Subcloning Techniques | Isolation of short DNA fragments | Required for sequencing manageable segments |
The Broader Historical Context and Significance
Connection to Subsequent CRISPR Research
The 1987 discovery remained an isolated curiosity for several years until similar sequences were identified in other organisms. In 1993, researchers observed comparable clustered repeats in the archaeon Haloferax mediterranei, which were initially termed Short Regularly Spaced Repeats (SRSRs) [1] [4]. Francisco Mojica at the University of Alicante played a pivotal role in recognizing that these disparate findings in bacteria and archaea represented the same phenomenon [5] [3]. By 2000, Mojica had identified similar repeat clusters in 20 microbial species, confirming they belonged to a common family [3]. The term CRISPR was formally proposed in 2002 by Ruud Jansen et al. to standardize the nomenclature [1] [3].
The functional understanding of CRISPR began to emerge in 2005 when three independent research groups recognized that the spacer sequences between repeats matched fragments of bacteriophage DNA and plasmids [1] [5] [3]. This critical insight led to the hypothesis that CRISPR constitutes an adaptive immune system in prokaryotes [5]. Experimental validation followed in 2007 when Barrangou et al. demonstrated that Streptococcus thermophilus could acquire new spacers from infecting bacteriophages and thereby develop resistance to subsequent infections [5] [3].
Methodological Evolution in CRISPR Research
The transition from initial discovery to functional characterization required significant advances in research methods:
CRISPR Research Methodology Evolution
The flow of methodological advances shows how the field progressed from basic observation to sophisticated manipulation of the CRISPR system. The automation of sequencing and development of bioinformatics tools were particularly crucial for recognizing the widespread distribution and common features of CRISPR loci across diverse microorganisms [1].
Timeline of Key Discoveries
Table 3: Major Milestones from Initial Discovery to Genome Editing Application
| Year | Discovery | Key Researchers | Significance |
|---|---|---|---|
| 1987 | Unusual repeats in E. coli | Ishino et al. | First documentation of CRISPR sequences |
| 1993-2000 | SRSRs in archaea and other bacteria | Mojica et al. | Recognition of common family of repeats |
| 2002 | cas genes identified | Jansen et al. | Discovery of genes associated with CRISPR |
| 2005 | Spacers match foreign DNA | Three independent groups | Hypothesis of adaptive immune function |
| 2007 | Experimental proof of adaptive immunity | Barrangou et al. | Demonstration of phage resistance mechanism |
| 2012 | CRISPR-Cas9 as programmable tool | Doudna, Charpentier, Siksnys | Development into genome editing technology |
The accidental discovery of unusual DNA repeats in E. coli in 1987 exemplifies how fundamental, curiosity-driven research can ultimately lead to transformative scientific breakthroughs. While the initial publication could only describe the unusual structure without understanding its function, it provided the essential foundation for deciphering the CRISPR-Cas system [1]. This discovery trajectory—from mysterious sequences to comprehensive understanding of an adaptive immune system and finally to revolutionary genome-editing technology—spanned nearly three decades and involved contributions from researchers worldwide [5].
The technological limitations of 1987, which made sequencing these repetitive regions so challenging, highlight how methodological advances can unlock the potential of earlier observations. Modern CRISPR-based technologies, including CRISPR-Cas9 genome editing, base editing, and gene regulation tools, all trace their origins to this initial characterization of unusual repeats in E. coli [6] [7]. The journey from the first observation to the Nobel Prize-winning application of CRISPR-Cas9 in 2020 demonstrates the unpredictable but profound impact of basic scientific research on biological understanding and technological capability [8].
{Abstract} The transformative journey of CRISPR from a curious genetic sequence in prokaryotes to a revolutionary genome-editing technology is a cornerstone of modern biotechnology. This whitepaper examines the pivotal role of Francisco Mojica, who first identified CRISPR as a prokaryotic adaptive immune system. His crucial insight provided the foundational hypothesis that redirected CRISPR research from a biological curiosity to a focused investigation of a microbial defense mechanism, ultimately enabling the development of CRISPR-Cas9 gene editing. This document details the experimental evidence that validated Mojica's hypothesis, the molecular mechanisms of CRISPR adaptive immunity, and the key reagents that facilitated these discoveries, providing a comprehensive technical guide for researchers and drug development professionals.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) locus was first observed in 1987 in Escherichia coli but its function remained enigmatic for years [9] [3]. These peculiar genetic elements, characterized by direct repeats interspaced with variable sequences, were noted in various bacterial and archaeal genomes without a clear understanding of their biological significance [8]. The pivotal turning point came through the persistent work of Francisco Mojica at the University of Alicante, who throughout the 1990s studied these repetitive sequences in archaeal organisms such as Haloferax mediterranei [5].
By 2000, Mojica had recognized that these disparate repeat sequences shared common features across species and coined the term CRISPR through correspondence with Ruud Jansen, who first used the term in print in 2002 [5] [3]. The critical breakthrough occurred in 2005 when Mojica and colleagues performed a comprehensive bioinformatic analysis demonstrating that the variable spacer sequences between CRISPR repeats were derived from viral and plasmid DNA [5] [3]. This led Mojica to hypothesize, correctly, that CRISPR constitutes an adaptive immune system in prokaryotes [5]. Concurrently, similar findings were reported by two other groups, but it was Mojica who first recognized the widespread nature and potential immunological function of these sequences [5] [3]. This hypothesis represented a paradigm shift in understanding prokaryotic defense mechanisms and set the stage for all subsequent CRISPR-based technologies.
Molecular Architecture of the CRISPR-Cas System
The CRISPR-Cas system consists of two fundamental genetic components: the CRISPR array and the cas (CRISPR-associated) genes [9] [10]. The CRISPR array is composed of an AT-rich leader sequence followed by short, partially palindromic repeats (typically 28-37 base pairs) separated by variable spacers of similar length (typically 32-38 bp) [9] [3]. These spacers originate from previously encountered foreign genetic elements and serve as a genetic memory of past infections [9] [10].
Flanking the CRISPR array are the cas genes, which encode the protein machinery responsible for the three stages of CRISPR-mediated immunity: adaptation, expression and biogenesis, and interference [9] [10]. While there is considerable diversity in CRISPR-Cas systems, classified into 2 classes, 6 types, and numerous subtypes, the universal presence of cas1 and cas2 across all types highlights their fundamental role in the adaptive immune function [9] [8]. The protein Cas1, in particular, is hypothesized to play a central role in the acquisition of new spacers, working in conjunction with other Cas proteins and potentially non-Cas cellular factors [10].
Table 1: Core Components of the CRISPR-Cas System
| Component | Structure/Composition | Biological Function |
|---|---|---|
| CRISPR Array | Leader sequence + repeats (28-37 bp) + spacers (32-38 bp) [9] [3] | Genomic record of past infections; template for crRNA production |
| Spacers | Variable sequences derived from viruses/plasmids [9] [10] | Immunological memory; guides Cas proteins to complementary invader sequences |
| Repeats | Short, partially palindromic DNA sequences [9] | Form hairpin structures in RNA; processing signals during crRNA biogenesis |
| cas Genes | cas1, cas2 (universal); signature genes (cas3, cas9, cas10 for Types I, II, III) [9] [8] | Encode protein machinery for adaptation, crRNA processing, and target interference |
| Leader Sequence | AT-rich region upstream of CRISPR array [10] | Promoter for transcription; site for integration of new spacers |
Experimental Validation of Mojica's Adaptive Immunity Hypothesis
Key Evidence fromStreptococcus thermophilusResearch
The first experimental validation of Mojica's hypothesis came in 2007 from researchers at Danisco France SAS, who demonstrated that the CRISPR-Cas system in S. thermophilus provides acquired resistance against bacteriophages [9] [5]. This seminal study, led by Rodolphe Barrangou and Philippe Horvath, provided direct evidence that CRISPR is an adaptive immune system by showing that:
- Exposure to bacteriophages led to the acquisition of new spacers derived from the infecting phage genome into the CRISPR locus [9] [5].
- These newly acquired spacers were integrated at the leader end of the CRISPR array, creating a chronological record of infections [9].
- The presence of these spacers conferred specific, heritable immunity against subsequent infections by phages containing matching sequences [9] [10].
- The removal of these spacers eliminated the immunity, confirming their essential role in the defensive mechanism [3].
This research also highlighted that only a subpopulation of bacteria successfully acquired new spacers and became immunized, but this subpopulation gained a high level of specific resistance [9]. The study further established that the system could target various regions of the viral genome, including both DNA strands and both coding and non-coding sequences [9].
Elucidating the Mechanism: From DNA Targeting to RNA-Guided Cleavage
Following the validation of adaptive immunity, subsequent research focused on unraveling the molecular mechanism. Key experiments included:
- 2008 - CRISPR arrays are transcribed and processed into guide RNAs: John van der Oost's group demonstrated that the CRISPR locus is transcribed into a long precursor RNA, which is then processed into small CRISPR RNAs (crRNAs) that guide Cas proteins to the target DNA [5] [3].
- 2008 - DNA is the molecular target: Luciano Marraffini and Erik Sontheimer confirmed that the CRISPR system targets and cleaves DNA, not RNA, establishing its potential as a DNA-editing tool [5] [3].
- 2010 - Cas9 is the sole nuclease required for cleavage: Sylvain Moineau's team provided biochemical evidence that the Cas9 protein creates double-stranded breaks in target DNA at precise positions, a defining feature of Type II CRISPR systems [5].
- 2011 - Discovery of tracrRNA: Emmanuelle Charpentier's group identified a second, essential RNA molecule, trans-activating CRISPR RNA (tracrRNA), which forms a duplex with crRNA to guide Cas9 [5].
Table 2: Key Experiments Validating CRISPR as an Adaptive Immune System
| Year | Lead Researcher(s) | Experimental System | Key Finding | Significance |
|---|---|---|---|---|
| 2005 | Francisco Mojica [5] | Computational analysis of multiple genomes | Spacers derive from viral/plasmid DNA | Formulated adaptive immunity hypothesis |
| 2007 | Rodolphe Barrangou, Philippe Horvath [9] [5] | Streptococcus thermophilus & phage challenge | Acquisition of phage-derived spacers confers specific immunity | First experimental proof of adaptive immunity |
| 2008 | John van der Oost [5] [3] | E. coli | CRISPR transcripts processed into small guide crRNAs | Elucidated the RNA-guided nature of the system |
| 2008 | Luciano Marraffini, Erik Sontheimer [5] [3] | Staphylococcus epidermidis | CRISPR system prevents plasmid conjugation by targeting DNA | Established DNA as the target molecule |
| 2010 | Sylvain Moineau [5] | S. thermophilus | Cas9 creates double-stranded breaks in target DNA | Identified the specific nuclease and its mechanism |
| 2011 | Emmanuelle Charpentier [5] | Streptococcus pyogenes | tracrRNA essential for crRNA maturation and Cas9 function | Completed the picture of the Cas9 guidance complex |
Diagram 1: CRISPR Adaptive Immunity Pathway and Key Discoveries
The Scientist's Toolkit: Essential Research Reagents and Methodologies
The experimental breakthroughs in characterizing CRISPR relied on specific biological tools and reagents. The following table details key resources that were instrumental in these foundational studies.
Table 3: Essential Research Reagents for Foundational CRISPR Research
| Research Reagent / Tool | Function in CRISPR Research | Application in Key Experiments |
|---|---|---|
| Bacterial Strains\newline(S. thermophilus, E. coli) | Model organisms for studying CRISPR function [9] [5] | Phage challenge experiments (Barrangou 2007); Heterologous system validation (Siksnys 2011) [5] |
| Bacteriophages & Plasmids | Sources of exogenous DNA (protospacers) to challenge the CRISPR system [9] [10] | Trigger spacer acquisition; test immunization specificity and efficiency [9] |
| CRISPR Locus Clones | Defined genetic constructs for functional studies in heterologous hosts [5] | Demonstrated CRISPR systems are self-contained units (Sapranauskas et al., 2011) [5] |
| Cas Protein Purification Kits | Isolation of active Cas enzymes for biochemical characterization [5] | In vitro cleavage assays to define Cas9 mechanism (Gasiunas et al., 2012; Jinek et al., 2012) [5] |
| RNA Sequencing Reagents | Identification and characterization of small CRISPR-derived RNAs (crRNA, tracrRNA) [5] | Discovery of crRNA (van der Oost 2008) and tracrRNA (Charpentier 2011) [5] |
The Bridge to Genome Editing: How an Immunity Mechanism Became a Tool
The characterization of CRISPR as an adaptive immune system directly enabled its repurposing into a programmable genome-editing tool. Understanding that crRNAs guide Cas proteins to specific DNA sequences for cleavage provided the conceptual framework for engineering this system [9] [5]. The critical technical leap was the simplification of the dual-RNA (crRNA and tracrRNA) structure into a single-guide RNA (sgRNA), creating a two-component system where a customizable sgRNA directs Cas9 to any DNA sequence adjacent to a Protospacer Adjacent Motif (PAM) [5] [11].
This reprogrammability was demonstrated in 2012-2013, when multiple groups showed that engineered CRISPR-Cas9 systems could edit genomes in human cells [5] [11]. The technology has since evolved beyond the original Cas9, with the discovery of other effectors like Cas12a (which targets DNA and has a different PAM requirement) and Cas13a (which targets RNA), further expanding the toolbox for basic research and therapeutic development [3]. The first FDA-approved CRISPR-based therapy, Casgevy for sickle cell disease and beta-thalassemia, marks the clinical realization of a technology that began with Mojica's crucial insight into a bacterial immune system [12] [11].
Francisco Mojica's recognition of CRISPR as a prokaryotic adaptive immune system represents one of the most consequential biological insights of the early 21st century. His hypothesis, built on astute bioinformatic analysis, provided the necessary framework that guided subsequent experimental research to validate and characterize the system's mechanisms. The collaborative work of scientists worldwide transformed this fundamental biological discovery into the precise and programmable CRISPR-Cas9 technology, ushering in a new era of genome engineering. Today, this technology is driving advances across biomedical research, with applications ranging from functional genomics and disease modeling to groundbreaking gene therapies, all stemming from the initial effort to understand an ancient form of microbial immunity.
The 2007 study by Barrangou, Horvath, and colleagues at Danisco marked a paradigm shift in molecular biology by providing the first experimental validation that the CRISPR-Cas system serves as an adaptive immune system in prokaryotes. Working with Streptococcus thermophilus, a bacterium crucial for yogurt and cheese production, the team demonstrated that bacteria acquire new spacers from invading bacteriophages and integrate these sequences into their CRISPR loci, conferring specific resistance against subsequent viral attacks. This foundational research not only elucidated a fundamental microbial defense mechanism but also paved the way for the development of CRISPR-Cas9 into a revolutionary genome-editing tool. This whitepaper details the experimental methodologies, quantitative findings, and conceptual breakthroughs of the 2007 study, framing it within the broader history of CRISPR research from bacterial immunity to gene editing applications.
Prior to 2007, the function of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) remained largely enigmatic despite several key discoveries.
- Initial Discoveries: Unusual repetitive sequences were first reported in E. coli in 1987 [3], and were later characterized in archaea and numerous bacteria by Francisco Mojica, who also coined the CRISPR acronym [8] [5].
- Emerging Hypothesis: By 2005, bioinformatic analyses by Mojica and others revealed that the "spacer" sequences between CRISPR repeats often matched sequences from bacteriophages and plasmids [13] [8]. This led to the hypothesis that CRISPR, along with its associated cas genes, might function as a prokaryotic immune system [7] [3].
- The Critical Unresolved Question: While the hypothesis was compelling, direct experimental evidence was lacking. The scientific community required definitive proof that bacteria could acquire new immunity by incorporating viral DNA into their genomes and that this process was specific and heritable. The 2007 study was designed to fill this critical knowledge gap, driven by a practical need in the dairy industry to protect bacterial cultures from viral contamination [13].
Experimental System and Methodology
The research team employed a straightforward yet powerful model system to test the adaptive immunity hypothesis.
Research Reagent Solutions
Table 1: Key research materials and their functions in the 2007 study.
| Research Material | Function in the Experiment |
|---|---|
| Streptococcus thermophilus | Model bacterium; primary subject for studying CRISPR-mediated immunity. |
| Bacteriophages | Viral pathogens used to challenge bacteria and trigger immune response. |
| CRISPR-Spacer Specific Primers | Oligonucleotides for PCR amplification and sequencing of CRISPR loci to monitor spacer acquisition. |
| Cas Gene Inactivation Constructs | Genetic tools to disrupt specific cas genes (e.g., cas5, cas7) to determine their functional roles. |
Core Experimental Workflow
The experimental design followed a logical progression from observation to manipulation, as outlined below.
Diagram 1: Core experimental workflow for validating adaptive immunity.
Key Experiments and Quantitative Results
The study provided conclusive evidence through a series of interlinked experiments.
Spacer Acquisition and Phage Resistance
The team first infected a phage-sensitive strain of S. thermophilus with two different bacteriophages and analyzed the CRISPR loci in surviving daughter strains [13].
Table 2: Observed spacer acquisition and resulting phage resistance.
| Experimental Condition | Change in CRISPR Array | Resistance Phenotype After Re-challenge |
|---|---|---|
| Infection with Phage 1 | Gain of 1-4 new spacers | Resistant to Phage 1 |
| Infection with Phage 2 | Gain of 1-4 new spacers | Resistant to Phage 2 |
| Co-infection with Phage 1 & 2 | Gain of up to 4 spacers (mix from both phages) | Resistant to both Phage 1 and Phage 2 |
| No Phage Challenge (Control) | No change in CRISPR array | Remained phage-sensitive |
The DNA sequences of the newly acquired spacers were a perfect match to the genomes of the infecting phages, providing a molecular record of the infection history [13] [5]. Furthermore, the resistance was highly specific; bacteria were only immune to phages whose DNA matched the spacers they had acquired [13].
Direct Causation via Spacer Manipulation
To move beyond correlation, the researchers directly manipulated spacer content.
- Spacer Deletion: They removed a specific spacer from a virus-resistant bacterial strain. This modification rendered the bacteria susceptible to the virus again, demonstrating that the spacer was necessary for immunity [13].
- Spacer Addition: They introduced a spacer specific to a particular virus into a previously susceptible bacterial strain. This engineered strain gained resistance to that virus, proving that the spacer was sufficient to confer immunity [13] [7].
Functional Analysis of Cas Proteins
The role of Cas proteins was investigated by inactivating specific cas genes in virus-resistant bacteria [13].
Table 3: Impact of Cas gene inactivation on bacterial immunity.
| Inactivated Gene | Known/Predicted Function | Effect on Phage Resistance | Functional Implication |
|---|---|---|---|
| cas5 | DNA-cutting enzyme (nuclease) | Loss of resistance | Essential for interfering with and inactivating viral DNA. |
| cas7 | Unknown at the time | Resistance maintained | Likely involved in the acquisition of new spacers, not interference. |
Discussion: Mechanistic Insight and Historical Impact
The Mechanism of CRISPR-Cas Adaptive Immunity
The 2007 study allowed Horvath and colleagues to propose a coherent model for CRISPR-Cas function, which subsequent research would elaborate on.
Diagram 2: Model of the adaptive immune process in bacteria.
Bridging Bacterial Immunity to Gene Editing Technology
The 2007 discovery was the crucial link that transformed CRISPR from a biological curiosity into a technological platform.
- Foundation for Gene Editing Tools: The demonstration that Cas9 was the sole nuclease required for interference [5] focused research efforts on this particular protein. The understanding that the system could be re-targeted simply by changing the spacer sequence was the fundamental insight that enabled its engineering for gene editing [13] [7].
- Direct Line to Nobel Prize: The work by Horvath and Barrangou established the functional principle. Subsequent research, including the characterization of the dual-RNA structure (crRNA and tracrRNA) by Charpentier, its simplification into a single-guide RNA (sgRNA) by Doudna and Charpentier, and its adaptation for use in eukaryotic cells by Zhang and Church, built directly upon this foundation [8] [5] [14]. This collective effort culminated in the award of the 2020 Nobel Prize in Chemistry to Charpentier and Doudna.
The 2007 yogurt bacterium study served as the critical experimental validation that propelled the CRISPR field forward. By rigorously demonstrating that the CRISPR-Cas system provides heritable, sequence-specific adaptive immunity in bacteria, Barrangou, Horvath, and their team unlocked a new era in molecular biology. Their work, rooted in solving an industrial problem, provided the mechanistic blueprint that allowed other scientists to repurpose bacterial defense machinery into the versatile, precise, and powerful CRISPR-Cas9 gene-editing tool. This tool is now revolutionizing basic research, therapeutic development, and biotechnology, illustrating how fundamental discovery research can have transformative and unforeseen impacts.
The transformation of the CRISPR-Cas system from a fundamental prokaryotic immune mechanism to a revolutionary genome-editing technology hinges on the discovery and understanding of its core molecular components: the Cas proteins, CRISPR RNA (crRNA), and the trans-activating crRNA (tracrRNA). These elements constitute the central machinery that allows bacteria and archaea to adaptively defend against invading genetic elements and provide researchers with a programmable platform for precise DNA manipulation. Within the broader history of CRISPR, the elucidation of these components represents the critical bridge between the observation of a natural bacterial immunity and the engineering of a versatile technological tool. This whitepaper provides an in-depth technical examination of the discovery, function, and interplay of these core components, framing them within the scientific journey that has reshaped modern biological research and therapeutic development.
Historical Context: From Bacterial Repeats to an Adaptive Immune System
The understanding of CRISPR evolved from the observation of curious genetic repeats to the realization of a sophisticated, adaptive immune system. Table 1 summarizes the key historical milestones that led to the identification of the central machinery.
Table 1: Historical Timeline of Key Discoveries of Core CRISPR Components
| Year | Discovery | Key Researchers/Team | Significance |
|---|---|---|---|
| 1987 | Identification of unusual repetitive sequences in E. coli | Ishino et al. [8] | Initial discovery of what would later be known as CRISPR. |
| 2000 | Recognition of common features in disparate repeat sequences; coinage of "CRISPR" | Francisco Mojica [5] | Unified disparate observations and provided a defining name for the phenomenon. |
| 2002 | Identification of Cas (CRISPR-associated) genes | Ruud Jansen et al. [8] | Found genes consistently located near CRISPR loci, suggesting a functional relationship. |
| 2005 | Hypothesis of CRISPR as an adaptive immune system; spacer origins in phage genes | Mojica et al.; Pourcel et al. [5] | Proposed the biological function and noted spacer sequences matched viral or plasmid DNA. |
| 2005 | Discovery of Cas9 and the Protospacer Adjacent Motif (PAM) | Alexander Bolotin et al. [8] [5] | Identified the key effector nuclease and the essential targeting motif. |
| 2007 | Experimental demonstration of adaptive immunity | Rodolphe Barrangou, Philippe Horvath et al. [8] [5] | Showed bacteria integrate new spacers upon phage exposure, conferring resistance. |
| 2008 | Identification of crRNAs as guides for interference | John van der Oost et al. [5] | Revealed that spacers are processed into small RNAs that guide targeting. |
| 2011 | Discovery of the essential tracrRNA | Emmanuelle Charpentier et al. [8] [15] [5] | Identified the second RNA component required for Cas9-mediated crRNA processing and DNA cleavage. |
The journey began in 1987 with the identification of unusual repetitive sequences in the E. coli genome, though their function remained unknown [8]. For years, Francisco Mojica was a central figure, recognizing these sequences as a distinct class and, in 2000, naming them CRISPR [5]. His critical insight in 2005, concurrently with another group, that the "spacer" sequences between repeats matched viral DNA, led to the correct hypothesis that CRISPR functions as an adaptive immune system [5]. That same year, Alexander Bolotin's discovery of the Cas9 gene and the PAM sequence provided essential clues about the specific machinery of the Type II CRISPR system [8] [5]. The system's adaptive nature was proven experimentally in 2007, and the mechanism was further clarified with the discovery that spacer sequences are transcribed into guide RNAs (crRNAs) [5]. The final, pivotal piece was the 2011 discovery of tracrRNA by Emmanuelle Charpentier, which completed the picture of the core machinery [8] [15] [5].
The Core Molecular Components
The functional unit of the Type II CRISPR-Cas system is composed of three core elements: the Cas protein effector, the crRNA, and the tracrRNA.
Cas Proteins: The Effector Enzymes
Cas proteins are the enzymes that execute the functions of the CRISPR system. The Cas9 nuclease is the hallmark effector of the Type II system.
- Function: Cas9 is a dual-RNA-guided DNA endonuclease that introduces double-stranded breaks (DSBs) in target DNA [7]. It contains two nuclease domains: an HNH domain that cleaves the DNA strand complementary to the crRNA guide, and a RuvC-like domain that cleaves the non-complementary strand [5].
- Discovery: Cas9 was first described in connection with CRISPR repeats in 2005 by Bolotin et al., who noted its novel nuclease motifs and its association with a specific sequence pattern adjacent to spacer targets (the PAM) [8].
- PAM Requirement: Cas9 requires a short Protospacer Adjacent Motif (PAM) sequence immediately following the target DNA region complementary to the crRNA. This requirement is critical for self versus non-self discrimination, preventing the Cas9 complex from attacking the bacterial genome's own CRISPR array [8] [5].
crRNA and tracrRNA: The Guidance System
The RNA components work in concert to direct Cas9 to its specific DNA target.
- crRNA (CRISPR RNA): The crRNA is processed from a long precursor transcript (pre-crRNA) of the entire CRISPR array. Each mature crRNA contains a spacer sequence (typically 20 nucleotides in engineered systems) that is complementary to the target DNA, serving as the guide [8] [15].
- tracrRNA (trans-activating crRNA): The tracrRNA is a small, non-coding RNA that is essential for crRNA maturation and Cas9 function. It is partially complementary to the repeat regions in the pre-crRNA.
- Discovery: Identified in 2011 by Charpentier et al. using high-throughput sequencing in Streptococcus pyogenes, it was one of the most abundant small RNAs in the cell [15] [5].
- Function: The tracrRNA base-pairs with the pre-crRNA repeats, forming a double-stranded RNA (dsRNA) structure. This duplex is a substrate for the host enzyme RNase III, which cleaves the pre-crRNA into individual, mature crRNAs [8] [15]. Furthermore, the mature tracrRNA remains associated with the crRNA and Cas9, forming the active ribonucleoprotein complex that surveils DNA [15].
Table 2: Core Molecular Components of the Type II CRISPR-Cas System
| Component | Type | Primary Function | Key Characteristics |
|---|---|---|---|
| Cas9 | Protein (Nuclease) | Effector enzyme; cleaves target DNA | Dual nuclease activity (HNH & RuvC domains); requires PAM for target recognition [8] [5]. |
| crRNA | RNA (Guide) | Specifies DNA target sequence | Contains the ~20 nt spacer sequence; processed from pre-crRNA; forms a duplex with tracrRNA [8] [15]. |
| tracrRNA | RNA (Trans-activating) | Facilitates crRNA maturation and Cas9 function | Base-pairs with crRNA repeat regions; essential for RNase III processing; part of the active complex [15] [5]. |
| PAM | DNA Motif | Self vs. non-self discrimination | Short (2-5 bp) DNA sequence adjacent to the target; required for Cas9 to initiate DNA unwinding and cleavage [8] [5]. |
The Single-Guide RNA (sgRNA) Engineering Breakthrough
A pivotal moment in the transition from biological mechanism to biotechnological tool was the engineering of the single-guide RNA (sgRNA). In 2012, researchers led by Charpentier and Doudna demonstrated that the two essential RNA components, the crRNA and tracrRNA, could be fused into a single chimeric molecule via a synthetic loop [15] [5]. This sgRNA recapitulates the function of the natural dual-RNA complex but greatly simplifies the system for experimental and therapeutic use, as only one RNA molecule needs to be designed and delivered to program Cas9 [15].
Molecular Mechanism and Key Experimental Protocols
The functional interplay between the core components follows a precise sequence of events, from crRNA biogenesis to target cleavage.
The crRNA Biogenesis and DNA Interference Pathway
Diagram 1: crRNA biogenesis and DNA interference pathway. This workflow illustrates the natural process from RNA transcription to target DNA cleavage in the Type II CRISPR-Cas system.
Detailed Methodologies for Key Experiments
The elucidation of this pathway relied on several foundational experiments.
Experiment 1: Demonstrating the Role of tracrRNA in crRNA Processing (2011)
- Objective: To identify and characterize the function of tracrRNA in the Type II CRISPR system of Streptococcus pyogenes.
- Protocol:
- Identification: Perform dRNA-seq (differential RNA sequencing) on S. pyogenes to catalog all primary transcripts and processed small RNAs [15].
- Localization: Map abundant small RNAs to the genome, identifying tracrRNA adjacent to the cas9 gene and noting its complementarity to CRISPR repeats [15].
- Genetic Knockdown: Use a conditional knockout to deplete tracrRNA and analyze the CRISPR array transcript via Northern blot. Result: Accumulation of unprocessed pre-crRNA, demonstrating tracrRNA is essential for maturation [15].
- In Vitro Reconstitution: Purify Cas9, RNase III, pre-crRNA, and tracrRNA. Incubate components and analyze products by gel electrophoresis. Result: Cleavage of pre-crRNA into mature crRNAs only occurs when all components are present [15].
Experiment 2: In Vitro Reconstitution of DNA Cleavage (2012)
- Objective: To demonstrate that Cas9, crRNA, and tracrRNA are sufficient for programmable DNA cleavage.
- Protocol:
- Component Purification: Recombinantly express and purify Cas9 protein. Chemically synthesize or in vitro transcribe crRNA and tracrRNA (or a fused sgRNA) [5].
- Ribonucleoprotein (RNP) Complex Formation: Pre-incubate Cas9 with the guide RNAs to form the active complex.
- Cleavage Assay: Incubate the RNP complex with a target DNA plasmid containing a complementary target site and the correct PAM.
- Analysis: Analyze the reaction products by agarose gel electrophoresis. The successful introduction of a double-strand break will linearize a supercoiled plasmid, resulting in a distinct band shift [5].
Table 3: The Scientist's Toolkit: Key Research Reagents for CRISPR Core Machinery Studies
| Reagent / Material | Function in Research | Specific Example / Note |
|---|---|---|
| Cas9 Expression Vector | Provides the genetic template for expressing the Cas9 nuclease in heterologous systems (e.g., E. coli or human cells). | The initial work by Siksnys et al. (2011) cloned the entire S. thermophilus CRISPR-Cas locus into E. coli to demonstrate it was a self-contained unit [5]. |
| Guide RNA Cloning Backbone | Plasmid vector (often with a U6 promoter) for expressing sgRNA or the separate crRNA and tracrRNA components. | Vectors are designed for easy insertion of a 20-nt guide sequence to target any locus of interest [16]. |
| RNase III | Host endoribonuclease used in vitro to study the natural crRNA biogenesis pathway. | Used in Charpentier et al. (2011) to demonstrate its essential role in processing the pre-crRNA:tracrRNA duplex [15]. |
| Synthetic crRNA & tracrRNA | Chemically synthesized RNAs for in vitro biochemical assays and formation of RNP complexes for direct delivery. | Allows for precise control over RNA sequence and chemical modifications; essential for the foundational in vitro cleavage assays [5]. |
| Target DNA Plasmid (with PAM) | A substrate for in vitro cleavage assays to validate the activity and specificity of the assembled CRISPR complex. | Typically contains a supercoiled plasmid with a target sequence matching the guide spacer and the required PAM sequence [5]. |
From Natural Machinery to Programmable Tool
The complete understanding of the core machinery enabled its repurposing into a revolutionary technology. The key steps were:
- Heterologous Function: The demonstration that the CRISPR-Cas system from S. thermophilus could function in E. coli proved it was a portable, self-contained unit [5].
- Biochemical Characterization: Work from the Siksnys lab (2012) and the Charpentier/Doudna collaboration (2012) purified the Cas9-crRNA-tracrRNA complex and definitively showed it could be reprogrammed to cut any DNA target of choice simply by changing the 20-nt guide sequence within the crRNA [5].
- sgRNA Engineering: The fusion of crRNA and tracrRNA into a single-guide RNA (sgRNA) dramatically simplified the system for widespread adoption [15] [5].
- Eukaryotic Genome Editing: The final leap was made in 2013 when multiple groups, including Feng Zhang and George Church, successfully adapted CRISPR-Cas9 for precise genome editing in human and mouse cells [5].
The Cleavage Mechanism of Cas9
Diagram 2: Cas9 DNA cleavage mechanism. The Cas9-sgRNA complex recognizes the target site via PAM binding and complementary base pairing. The HNH nuclease domain cleaves the target strand (complementary to the sgRNA), while the RuvC domain cleaves the non-target strand, resulting in a blunt-ended double-strand break.
Frontiers and Future Directions
The exploration of the central CRISPR machinery continues to advance rapidly. Current research focuses on overcoming initial limitations and expanding functionality:
- Enhancing Specificity: Engineering high-fidelity Cas9 variants (e.g., SpCas9-HF, eSpCas9) with reduced off-target effects through rational mutagenesis [7].
- Expanding the Toolbox: Discovery and characterization of novel Cas effectors beyond Cas9 (e.g., Cas12, Cas13) with different properties, PAM requirements, and the ability to target RNA [7] [17].
- Precision Editing: Development of "base editors" and "prime editors" that directly convert one base to another without causing a DSB, offering greater precision and safety for therapeutic applications [7] [18].
- AI-Driven Design: The use of large language models (LMs) to design novel, highly functional CRISPR-Cas proteins that do not exist in nature. A 2025 study demonstrated the AI-generated editor "OpenCRISPR-1," which is highly active and specific despite being 400 mutations away from any known natural Cas9 [19]. This represents a move from mining natural diversity to de novo computational creation of core machinery.
The discovery and functional characterization of the central machinery—Cas proteins, crRNA, and the essential tracrRNA—unlocked the true potential of the CRISPR system. What began as a fundamental inquiry into a bacterial immune mechanism has yielded a programmable platform that is simple, efficient, and versatile. The ongoing refinement and expansion of this core toolbox, from high-fidelity variants to AI-designed editors, continues to drive progress across basic research, therapeutic development, and biotechnology, solidifying its role as one of the most transformative technologies in modern science.
The protospacer adjacent motif (PAM) represents a fundamental genetic signature that enables CRISPR-Cas systems to distinguish between self and non-self DNA, thereby driving the function of bacterial adaptive immunity. This technical guide examines Alexander Bolotin's seminal 2005 discovery of the PAM sequence and its pivotal role in CRISPR target recognition. We explore the mechanistic basis of PAM function, its necessity in CRISPR experiment design, and the evolving landscape of PAM utilization from natural systems to engineered variants with expanded targeting capabilities. Within the broader context of CRISPR history, Bolotin's identification of this essential motif provided the critical missing link that ultimately enabled the development of precise genome editing technologies now revolutionizing basic research and therapeutic development.
The CRISPR-Cas system represents a remarkable example of how fundamental bacterial microbiology can yield transformative technological applications. The journey from observing unusual genetic repeats in prokaryotes to programming precise genome editors hinges on understanding molecular recognition mechanisms. Central to this story is the protospacer adjacent motif (PAM)—a short, specific DNA sequence that must flank CRISPR target sites for successful recognition and cleavage by Cas nucleases [20] [21].
The significance of the PAM extends far beyond its biochemical role; it represents the system's security mechanism for distinguishing invading viral DNA from the bacterium's own genetic material [20]. This self versus non-self discrimination capability proved to be the critical feature that allowed researchers to harness CRISPR as a programmable genome engineering tool rather than merely an interesting bacterial immunity phenomenon.
Alexander Bolotin's key finding emerged from his 2005 study of Streptococcus thermophilus at the French National Institute for Agricultural Research (INRA) [22] [5]. While examining a newly sequenced CRISPR locus, Bolotin and colleagues noted not only novel Cas genes (including what would become known as Cas9) but also made a crucial observation: the spacers, which shared homology with viral genes, all contained a common sequence at one end [22] [5]. This conserved motif, later termed the protospacer adjacent motif, would prove essential for target recognition in CRISPR systems.
Historical Context: Bolotin's Key Discovery
The Research Landscape in 2005
By 2005, Francisco Mojica had already established that CRISPR sequences matched snippets from bacteriophage genomes, correctly hypothesizing that CRISPR functions as an adaptive immune system [22] [8] [5]. However, a fundamental question remained: how could bacterial cells maintain a library of viral DNA sequences without triggering self-destruction? The solution to this paradox emerged from Bolotin's analysis of Streptococcus thermophilus strain LMD-9.
Bolotin's key contribution was recognizing that while spacers in the bacterial CRISPR array lacked specific flanking sequences, the matching viral protospacers consistently contained a conserved nucleotide motif at one end [5]. This observation revealed the PAM's function as a "non-self" identifier—the bacterial genome lacked PAM sequences adjacent to stored spacers, thereby preventing autoimmune cleavage [20] [21].
Experimental Basis for PAM Identification
Bolotin's discovery emerged from computational analysis of spacer-protospacer alignments, a methodology that would become foundational for PAM characterization [23]. His team analyzed the S. thermophilus CRISPR locus and observed that:
- Spacer Origin: Spacers derived from extrachromosomal elements, primarily viruses
- Conserved Flanking Sequence: All protospacers shared a common adjacent motif
- Novel Cas Genes: The locus contained previously uncharacterized genes, including one encoding a large protein with predicted nuclease activity (later named Cas9)
This bioinformatic approach revealed that the PAM sequence was consistently present in viral DNA but absent from the bacterial CRISPR array, providing the first clue to its role in self/non-self discrimination [22] [5].
The Molecular Mechanism of PAM Function
Self Versus Non-Self Discrimination
The PAM sequence solves a critical security challenge for the CRISPR system: how to identify invading DNA while ignoring the bacterial genome's own CRISPR arrays. The mechanism is elegant in its simplicity:
- Invading DNA: Contains target sequence (protospacer) with adjacent PAM → cleavage occurs
- Bacterial CRISPR DNA: Contains spacer sequence without adjacent PAM → no cleavage [20] [21]
This discrimination occurs because Cas nucleases first search for PAM sequences before unwinding DNA to check for guide RNA complementarity [20] [23]. When Cas identifies the correct PAM, it undergoes conformational changes that enable DNA unwinding and subsequent guide RNA matching. Without PAM recognition, the interrogation process does not initiate, regardless of target sequence complementarity.
Structural Basis of PAM Recognition
Structural studies have revealed that Cas proteins contain specialized PAM-interacting domains that physically recognize specific DNA sequences [23]. For the commonly used Streptococcus pyogenes Cas9 (SpCas9), the PAM interaction domain recognizes 5'-NGG-3' sequences through a combination of base-specific contacts and DNA distortion mechanisms. This specific protein-DNA interaction triggers conformational changes in Cas9 that facilitate:
- Local DNA melting to create a DNA "bubble"
- RNA-DNA hybridization between the guide RNA and target strand
- Nuclease activation and double-strand break formation 3-4 nucleotides upstream of the PAM [20]
Table 1: PAM Sequences for Commonly Used CRISPR Nucleases
| CRISPR Nuclease | Organism Isolated From | PAM Sequence (5' to 3') |
|---|---|---|
| SpCas9 | Streptococcus pyogenes | NGG |
| SaCas9 | Staphylococcus aureus | NNGRRT or NNGRRN |
| NmeCas9 | Neisseria meningitidis | NNNNGATT |
| CjCas9 | Campylobacter jejuni | NNNNRYAC |
| LbCas12a (Cpf1) | Lachnospiraceae bacterium | TTTV |
| AacCas12b | Alicyclobacillus acidiphilus | TTN |
| hfCas12Max | Engineered from Cas12i | TN and/or TNN |
Figure 1: PAM-Mediated Target Recognition Cascade. The PAM sequence initiates a sequential process where (1) Cas9 recognizes the PAM, (2) unwinds adjacent DNA, (3) enables guide RNA complementarity checking, and (4) triggers DNA cleavage if matching occurs.
PAM Requirements in CRISPR Experiment Design
Target Site Selection Constraints
The PAM sequence imposes the primary constraint on CRISPR target site selection, as editing can only occur at genomic locations containing the appropriate nuclease-specific PAM [20]. For the most commonly used SpCas9, this means any target site must be followed by 5'-NGG-3' (where N is any nucleotide). This requirement fundamentally influences guide RNA design and experimental planning.
Several strategies have emerged to overcome PAM-imposed limitations:
- Nuclease Selection: Choosing alternative Cas proteins with different PAM requirements (see Table 1)
- PAM Engineering: Using engineered Cas variants with altered PAM specificities
- Target Locus Analysis: Identifying available PAM sequences near the desired edit site [20]
Experimental Determination of PAM Specificity
Several methodologies have been developed to characterize PAM requirements for novel or engineered Cas nucleases:
Plasmid Depletion Assay
This in vivo approach involves transforming a host expressing the CRISPR-Cas system with a plasmid library containing randomized DNA adjacent to a target sequence. Plasmids with functional PAM sequences are depleted, while those with non-functional PAMs are retained and quantified via next-generation sequencing [23].
Protocol:
- Clone a target sequence followed by a randomized NNNN region into a plasmid
- Transform the plasmid library into cells expressing the Cas nuclease and guide RNA
- Harvest plasmids after selection and sequence the randomized region
- Compare sequence abundance to the initial library to identify depleted PAMs
PAM-SCANR (PAM Screen Achieved by NOT-gate Repression)
This high-throughput method uses a catalytically dead Cas variant (dCas9) coupled to a transcriptional repressor. When dCas9 binds to a functional PAM, it represses GFP expression, enabling fluorescence-activated cell sorting to isolate and sequence functional PAM sequences [23].
Protocol:
- Create a target library with randomized PAM regions upstream of a GFP reporter
- Express dCas9-repressor fusion and guide RNA in host cells
- Sort low-GFP populations via FACS
- Isolate and sequence plasmids to identify functional PAM motifs
In Vitro Cleavage Selection
This biochemical approach incubates purified Cas nuclease with a DNA library containing randomized PAM regions, followed by sequencing of cleaved products to identify functional PAMs [23].
Protocol:
- Synthesize double-stranded DNA library with target sequence and randomized PAM region
- Incubate with purified Cas nuclease and guide RNA
- Isolate cleaved DNA fragments
- Sequence to determine PAM preferences
Table 2: PAM Identification Methods Comparison
| Method | Principle | Throughput | Required Resources | Key Advantage |
|---|---|---|---|---|
| Plasmid Depletion | Survival of non-targeted plasmids | Medium | Expression system, NGS | Works in living cells |
| PAM-SCANR | Transcriptional repression of reporter | High | FACS, dCas9-repressor | Quantitative results |
| In Vitro Cleavage | Direct sequencing of cleaved DNA | High | Purified proteins, NGS | Controlled conditions |
| Bioinformatic Analysis | Protospacer alignment | Highest | Sequencing databases | Identifies natural PAMs |
PAM Diversity and Engineering
Natural PAM Diversity Across CRISPR Systems
The diversity of naturally occurring CRISPR systems provides researchers with an extensive toolkit of Cas nucleases with varying PAM requirements. This natural variation reflects evolutionary adaptation to different viral environments and enables targeting of distinct genomic regions [20] [23].
Class 2 CRISPR systems (including Cas9 and Cas12 proteins) demonstrate remarkable PAM diversity:
- Type II systems (Cas9): Typically recognize short PAM sequences (2-5 bp) adjacent to the target
- Type V systems (Cas12): Often recognize T-rich PAM sequences located upstream of the target
- Type VI systems (Cas13): Target RNA and utilize protospacer flanking sites (PFS) rather than PAMs [23]
Engineered Cas Variants with Altered PAM Specificity
Protein engineering approaches have generated Cas variants with expanded or altered PAM recognition, dramatically increasing targeting scope:
- xCas9: Recognizes NG, GAA, and GAT PAMs, broadening targeting range
- SpCas9-NG: Engineered to recognize NG PAMs instead of NGG
- SpRY: Near-PAMless variant recognizing NRN and to some extent NYN PAMs
- Engineered Cas12 variants: Such as hfCas12Max with simplified TN PAM requirement [20]
These engineered variants employ directed evolution and structure-based design to modify PAM-interacting domains while maintaining nuclease activity, enabling targeting of previously inaccessible genomic regions.
The Research Toolkit: Essential Reagents and Methods
Table 3: Essential Research Reagents for PAM Studies
| Reagent/Method | Function | Application Examples |
|---|---|---|
| Cas Nuclease Expression Vector | Expresses Cas protein in target cells | SpCas9, SaCas9, LbCas12a |
| Guide RNA Cloning System | Enables programmable target recognition | sgRNA scaffold, crRNA expression |
| PAM Library Constructs | Randomized DNA sequences for PAM characterization | Plasmid depletion assays |
| dCas9-Repressor Fusions | Binds DNA without cleavage for PAM-SCANR | KRAB-dCas9, dCas9-Mxi1 |
| NGS Library Prep Kits | Sequences PAM regions after selection | Illumina-compatible kits |
| Fluorescent Reporter Systems | Reports Cas binding via fluorescence | GFP under constitutive promoter |
| Cell Sorting Capability | Separates cells based on PAM activity | FACS with GFP detection |
| Cas1-Cas2 Complex | Studies spacer acquisition preferences | In vitro adaptation assays |
Clinical Applications and Therapeutic Implications
PAM Considerations in Therapeutic Development
The transition of CRISPR technology from research tool to clinical application introduces additional PAM-related considerations. Therapeutic efficacy depends on targeting specific genomic loci, which may be constrained by PAM availability [12]. Key developments include:
- CASGEVY (exagamglogene autotemcel): The first FDA-approved CRISPR therapy for sickle cell disease and transfusion-dependent beta thalassemia utilizes ex vivo editing where PAM availability is carefully mapped near the BCL11A enhancer target [12]
- In Vivo Therapies: Intellia Therapeutics' NTLA-2001 for hereditary transthyretin amyloidosis demonstrates systemic CRISPR delivery, requiring comprehensive PAM analysis at the TTR gene [12]
- Personalized Therapies: The first bespoke in vivo CRISPR treatment for CPS1 deficiency highlights how PAM mapping enables rapid therapeutic development for ultra-rare diseases [12]
PAM-Dependent Safety Considerations
PAM recognition contributes to CRISPR specificity but doesn't eliminate off-target concerns. Advanced therapeutic development employs:
- PAM Blocking Mutations: Engineering Cas variants that require longer or more specific PAMs to reduce off-target effects
- Computational Prediction: Identifying potential off-target sites with similar sequences and NGG PAMs
- GUIDE-Seq: Unbiased identification of off-target sites in clinical applications [21]
Figure 2: Evolution of PAM Understanding from Basic Research to Clinical Application. The timeline shows how PAM knowledge progressed from Bolotin's initial discovery through mechanistic understanding and protein engineering to current clinical applications.
Alexander Bolotin's identification of the PAM sequence provided the crucial missing piece in understanding CRISPR immune function—the mechanism for self versus non-self discrimination. This fundamental insight enabled the reprogramming of CRISPR systems into precise genome editing tools that have revolutionized biological research and therapeutic development.
Future directions in PAM research and application include:
- PAMless Editors: Continued development of truly PAM-independent nucleases for unrestricted targeting
- Disease-Specific Variants: Engineering Cas proteins with PAM preferences matching therapeutic target sites
- Multiplexed Editing: Utilizing Cas proteins with different PAM requirements for simultaneous editing at multiple loci
- Delivery Optimization: Matching PAM requirements with delivery constraints for in vivo applications
The evolution from Bolotin's initial observation to sophisticated clinical applications exemplifies how fundamental microbiological research can drive transformative technological advances. As CRISPR technology continues to mature, the PAM sequence remains central to expanding targeting capabilities while maintaining specificity—the delicate balance that will define the next generation of genome editing therapeutics.
The journey of CRISPR-Cas9 from a curious bacterial repeat sequence to a revolutionary gene-editing tool is a landmark in biotechnology. Initially identified as a component of the adaptive immune system in prokaryotes, which provides heritable immunity against mobile genetic elements by incorporating spacers from foreign DNA into CRISPR loci, the system was repurposed into a highly programmable DNA cleavage tool following the key discovery that the Cas9 nuclease activity is guided by a complex of crRNA and tracrRNA, later simplified to a single-guide RNA (sgRNA) [8]. This historical foundation sets the stage for the critical biochemical interrogation of Cas9: to fully harness its potential and safely translate it into therapies, a rigorous, quantitative understanding of its enzymatic behavior is the essential final puzzle piece. This guide details the core experiments and methodologies that define the biochemical character of Cas9-mediated DNA cleavage, providing a resource for researchers driving the next wave of precision medicine.
Core Principles of Cas9-DNA Interaction
The Cas9-sgRNA complex performs target recognition and cleavage through a multi-step mechanism. The protospacer adjacent motif (PAM), a short nucleotide sequence adjacent to the target DNA site, serves as the initial anchor point for Cas9 binding. Following PAM recognition, the sgRNA unwinds the DNA duplex and base-pairs with the target strand (protospacer), forming an R-loop structure that positions the nuclease domains (HNH and RuvC) for cleavage of the complementary and non-complementary DNA strands, respectively [8] [24]. This process is sensitive to allosteric regulation and structural remodeling, which can be influenced by factors such as temperature and the presence of non-specific competitors [25] [26].
The following diagram illustrates the sequential mechanism of DNA recognition and cleavage by the Cas9-sgRNA complex.
Quantitative Characterization of Cleavage Kinetics and Specificity
Biochemical characterization yields critical quantitative parameters that predict Cas9 behavior in complex cellular environments. The data below summarize key performance metrics related to editing efficiency, kinetics, and specificity.
Table 1: Key Quantitative Parameters of CRISPR-Cas9 Activity
| Parameter | Description | Experimental Value | Significance / Impact |
|---|---|---|---|
| Homologous Recombination Efficiency [27] | Efficiency of inserting a large (~45 kb) donor fragment via HDR in mouse ESCs with CRISPR facilitation. | 11% - 16% | Demonstrates significant enhancement of HDR over traditional methods (0.05% efficiency), enabling large-scale genomic engineering. |
| Off-Target Mismatch Tolerance [28] [29] | Number of base pair mismatches between sgRNA and DNA that Cas9 can tolerate while still causing cleavage. | 3 - 5 bp | Underpins the primary risk of off-target editing; a key driver for developing high-fidelity variants. |
| sgRNA Assembly Kinetics [25] | The rate at which Cas9 and sgRNA form an active effector complex, delayed by non-specific RNA competitors. | Sensitive to RNA competitors | Complex formation rate, not just stability, can be a limiting factor in cells, influencing editing efficiency. |
| sgRNA Affinity (Kd) [25] | Equilibrium dissociation constant for Cas9 binding to a truncated sgRNA (lacking stem loops 2 & 3). | ~1 nM | Truncated guides retain high affinity, but their in vivo activity is lower, suggesting kinetics and stability are critical. |
Table 2: PAM Sequence Requirements for Different Cas9 Orthologues
Understanding PAM requirements is essential for determining targetable sites in a genome. The following table summarizes known PAM preferences for several characterized Cas9 proteins.
| Cas9 Orthologue | Source Organism | Protospacer Adjacent Motif (PAM) | Implications for Targetable Sequence Space |
|---|---|---|---|
| Spy Cas9 [24] | Streptococcus pyogenes | NGG | The most commonly used variant; targets a site every ~8 bp on average in the human genome. |
| Sth1 Cas9 [24] | Streptococcus thermophilus (CRISPR1) | NNAGAAW (W = A or T) | Requires a longer, more specific PAM, drastically reducing potential target sites but increasing intrinsic specificity. |
| Sth3 Cas9 [24] | Streptococcus thermophilus (CRISPR3) | NGGNG | A relaxed PAM compared to Sth1, but still more constrained than Spy Cas9. |
| Blat Cas9 [24] | Brevibacillus laterosporus | NNNCNDD (D = A, G, or T) | Showcases the diversity of natural PAM sequences, expanding the toolbox for orthogonal genome editing. |
Essential Experimental Protocols for Biochemical Characterization
Temperature-Dependent DNA Cleavage Assay
This protocol, adapted from established methods, is crucial for characterizing Cas9 enzymes from extremophiles or engineering variants with altered thermal stability [26]. It allows for qualitative and quantitative assessment of DNA cleavage efficiency across a broad temperature range.
Graphical Overview of Temperature-Dependent Cleavage Assay
Detailed Protocol Steps
- Ribonucleoprotein (RNP) Complex Formation: Incubate purified recombinant Cas9 protein with a molar excess of in vitro transcribed or synthetic sgRNA in a suitable binding buffer (e.g., 20 mM Tris-HCl pH 7.5, 120 mM NaCl, 5% glycerol, 0.1 mM DTT, 1 mM MgCl₂). A typical reaction uses 3 nM Cas9 and 5 nM sgRNA [25].
- Thermocycling: Subject the RNP mixture to a brief thermocycling protocol (e.g., 37°C for 10 min, followed by a slow ramp-down to room temperature) to facilitate proper complex formation.
- Temperature-Dependent Cleavage Reaction:
- Prepare reaction mixtures containing the pre-formed RNP complex and target DNA (e.g., a PCR-amplified fragment or plasmid containing the target protospacer and PAM).
- Distribute the mixture into separate PCR tubes and incubate them at different temperatures (e.g., from 25°C to 75°C) for a fixed duration (e.g., 30-60 minutes). The 5× reaction buffer final concentrations are 100 mM Tris-HCl (pH 7.5), 500 mM KCl, 25 mM MgCl₂, 5 mM DTT, and 25% (w/v) glycerol [26].
- Reaction Termination: Stop the cleavage reaction by adding Proteinase K (e.g., 20 mg/mL stock) and incubating at 56°C for 15-30 minutes to digest the Cas9 protein.
- Analysis by Gel Electrophoresis:
- Purify the DNA and resolve the products using agarose gel electrophoresis.
- Visualize the DNA bands with a fluorescent nucleic acid stain (e.g., GelRed). The intact supercoiled/linear DNA substrate and the smaller cleaved products will be separated, allowing for quantification of the cleavage efficiency via densitometry.
In Vitro Determination of Protospacer Adjacent Motif (PAM) Requirements
Empirically defining the PAM sequence is a prerequisite for deploying any novel Cas9 orthologue. This method uses a randomized plasmid library to directly identify sequences that support Cas9 cleavage [24].
Workflow for Empirical PAM Determination
Detailed Protocol Steps
- Randomized PAM Library Construction: Clone a DNA oligonucleotide containing a fixed protospacer sequence (complementary to the sgRNA spacer) followed by a stretch of fully randomized nucleotides (e.g., 5-7 bp) into a plasmid vector. Transform into E. coli to generate a comprehensive library of potential PAM sequences [24].
- In Vitro Digestion: Isolate the plasmid library and digest it with purified Cas9 pre-loaded with the corresponding sgRNA. Use a range of Cas9 concentrations to assess cleavage efficiency in a dose-dependent manner.
- Capture of Cleaved Products: Ligate specific adapters to the blunt ends generated by Cas9 cleavage. To increase ligation efficiency, the ends can be tailed with a single dA nucleotide, and the adapters can contain a complementary dT overhang.
- PCR Enrichment and Sequencing: Amplify the cleaved (and now adapter-ligated) plasmid fragments using a primer binding to the adapter and another primer adjacent to the randomized PAM region. Subject the resulting PCR amplicons to deep sequencing.
- Bioinformatic Analysis: Identify the PAM sequences by extracting the randomized region from sequencing reads that perfectly match the flanks of the protospacer. Generate a position frequency matrix (PFM) and sequence logo to visualize the PAM consensus [24].
The Scientist's Toolkit: Key Reagents and Materials
Successful biochemical characterization relies on high-quality, well-defined reagents. The following table lists essential components for the experiments described in this guide.
Table 3: Essential Research Reagents for Cas9 Biochemical Assays
| Reagent / Material | Function / Role | Key Considerations |
|---|---|---|
| Recombinant Cas9 Protein | The core effector enzyme. Can be wild-type (wtCas9), catalytically dead (dCas9), or high-fidelity variants (e.g., SpCas9-HF1). | Requires high purity (>95%). Purification often involves affinity tags (e.g., His-tag). Source (mesophile vs. thermophile) determines optimal assay temperature [25] [26]. |
| In Vitro Transcribed or Synthetic sgRNA | Guides Cas9 to the specific DNA target. | Full-length sgRNAs (with all 3 stem loops) show superior performance and stability in vivo. Chemically modified synthetic sgRNAs (e.g., with 2'-O-Me, PS bonds) can enhance stability and reduce off-target effects [25] [29]. |
| Target DNA Substrate | The molecule to be cleaved. Can be a short double-stranded DNA oligo (e.g., "Cas9 beacon"), a PCR amplicon, or a plasmid. | Must contain the target protospacer and a functional PAM. Plasmid-based substrates are common for initial validation and PAM determination assays [25] [24]. |
| 5× In Vitro Cleavage Buffer [26] | Provides optimal ionic and pH conditions for Cas9 activity. | A typical recipe includes: 100 mM Tris-HCl (pH 7.5), 500 mM KCl, 25 mM MgCl₂, 5 mM DTT, and 25% glycerol. DTT should be added fresh. |
| Proteinase K | Terminates the cleavage reaction by digesting the Cas9 protein. | Prevents further cleavage during downstream analysis steps like gel loading [26]. |
| Cas9 Beacon / FRET Probes [25] | Fluorophore-quencher labeled dsDNA probes for real-time kinetic measurements of RNP assembly and DNA binding. | Allows for rapid quantification of binding kinetics and inhibition without gel electrophoresis. The signal increases upon Cas9 binding and strand displacement. |
Addressing the Critical Challenge of Off-Target Effects
A primary safety concern in therapeutic applications is off-target editing, where Cas9 cleaves unintended genomic sites with sequence similarity to the sgRNA. Biochemical studies have shown that wild-type Cas9 can tolerate up to 3-5 base pair mismatches between the sgRNA and DNA, depending on their position and distribution [28] [29].
Multiple strategies have been developed to mitigate this risk, informed by biochemical characterization:
- High-Fidelity Cas9 Variants: Engineered mutants (e.g., eSpCas9, SpCas9-HF1) with redesigned protein-DNA interfaces to reduce tolerance for mismatches.
- Optimized sgRNA Design: Careful selection of sgRNAs with high predicted on-target activity and minimal homology to other genomic sites using in silico tools (e.g., CRISPOR). Guides with higher GC content and specific lengths (17-20 nt) can improve specificity [29].
- Alternative CRISPR Systems: Using Cas9 orthologues with longer or more complex PAM requirements (e.g., Sth1 Cas9) naturally reduces the number of potential off-target sites in the genome [24].
- RNP Delivery: The use of pre-assembled Cas9 protein-sgRNA ribonucleoprotein (RNP) complexes, as opposed to plasmid DNA encoding the components, shortens the cellular exposure time to the nuclease, thereby reducing off-target activity [29].
- Advanced Detection Methods: Unbiased methods like GUIDE-seq, CIRCLE-seq, and whole-genome sequencing (WGS) are employed to empirically identify off-target sites in relevant cell models, moving beyond purely computational prediction [28] [30] [29].
The Engineering Leap: Reprogramming CRISPR for Biomedical Applications
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and their associated Cas proteins originated from the study of an adaptive immune system in prokaryotes. This system allows bacteria and archaea to defend themselves against mobile genetic elements, such as viruses, by integrating short snippets of foreign DNA (spacers) into their own genome. These spacers, transcribed into short RNA molecules, then guide Cas nucleases to cleave complementary invading DNA sequences in a sequence-specific manner [8] [31]. The journey from this fundamental biological discovery to a revolutionary genome-editing tool was marked by key breakthroughs. A critical simplification came in 2012 when Jinek et al. demonstrated that the dual RNA components of the native system—the CRISPR RNA (crRNA) and the trans-activating crRNA (tracrRNA)—could be fused into a single-guide RNA (sgRNA) [8] [5]. This created a two-component system where the Cas9 nuclease could be programmed with a single RNA molecule to cut any DNA sequence complementary to the guide and adjacent to a short Protospacer Adjacent Motif (PAM) [32]. While this work established a programmable DNA-cutting enzyme in vitro, the pivotal paradigm shift occurred in early 2013, when multiple research groups independently demonstrated that this engineered CRISPR-Cas9 system could be harnessed to edit the genomes of eukaryotic cells [5] [32].
The Eukaryotic Breakthrough: Key Experimental Demonstrations
The successful adaptation of CRISPR-Cas9 for eukaryotic genome editing was a watershed moment, transforming the system from a powerful biochemical tool into a transformative technology for genetic research and therapy. The key challenge was to demonstrate that the bacterial Cas9-sgRNA complex could function within the more complex environment of a eukaryotic cell, which includes navigating the cytoplasm and entering the nucleus.
Landmark Publications of January 2013
Within a week in January 2013, two seminal papers were published that conclusively showed CRISPR-Cas9 could mediate genome editing in human and mouse cells.
Zhang Lab (Broad Institute/MIT): On January 3, a team led by Feng Zhang published the first report demonstrating CRISPR-Cas9 genome editing in eukaryotic cells [5] [33]. Their work, published in Science, showed that the system could be used for targeted gene disruption and homology-directed repair (HDR) in human and mouse cells [5] [32]. A critical technical hurdle they overcame was the adaptation of the bacterial Cas9 for expression and function in mammalian cells. This involved codon-optimizing the Cas9 gene from Streptococcus pyogenes to enhance its expression in human cells and appending a nuclear localization signal (NLS) to the protein to ensure its transport into the nucleus [33]. They also developed expression strategies for the sgRNA using a U6 polymerase III promoter, which is efficient for producing small RNAs in mammalian cells [33] [32].
Church Lab (Harvard University): In the same issue of Science, a team led by George Church reported similar success, showing targeted genome editing in human cells [5]. This concurrent publication provided immediate, independent validation of the CRISPR-Cas9 system's functionality and versatility in eukaryotes, a critical factor for its rapid adoption by the scientific community.
The following table summarizes the core methodological details from these foundational studies:
Table 1: Key Experimental Parameters from Landmark 2013 Eukaryotic CRISPR Studies
| Experimental Parameter | Zhang Lab (Cong et al.) | Church Lab (Mali et al.) |
|---|---|---|
| Cell Lines Tested | Human (HEK293) & Mouse (N2a) cells | Human (HEK293) cells |
| Target Genes | EMX1, PVALB (human); Th (mouse) | EMX1, PVALB |
| Cas9 Source | Streptococcus pyogenes (SpCas9) | Streptococcus pyogenes (SpCas9) |
| Key Adaptations | Codon-optimized Cas9; Nuclear Localization Signal (NLS) | Codon-optimized Cas9; Nuclear Localization Signal (NLS) |
| Delivery Method | Plasmid transfection | Plasmid transfection |
| Editing Demonstrated | Multiplex gene editing; Homology-Directed Repair (HDR) | Gene disruption; HDR |
| Efficiency Reported | HDR efficiency of up to 38% (varies by locus) | Indel formation of 2% to 38% (varies by locus) |
Technical Hurdles and Innovative Solutions
The transition from a prokaryotic immune system to a eukaryotic editing tool required solving several key problems, as outlined in the workflow below. The teams led by Zhang and Church developed similar and critical solutions to enable this paradigm shift.
Diagram 1: Overcoming Technical Hurdles for Eukaryotic CRISPR
The Scientist's Toolkit: Core Reagents for Early Eukaryotic CRISPR
The initial demonstrations of CRISPR in eukaryotic cells relied on a core set of engineered reagents that became the foundation for all subsequent applications. These components solved the critical problems of expression, localization, and function within a mammalian cellular environment.
Table 2: Essential Research Reagent Solutions for Eukaryotic CRISPR-Cas9
| Reagent / Solution | Function & Description | Role in Eukaryotic Adaptation |
|---|---|---|
| Codon-Optimized Cas9 | A version of the Cas9 gene where the nucleotide sequence is altered to match the codon usage bias of the target organism (e.g., human) without changing the amino acid sequence. | Dramatically improves the efficiency of Cas9 protein expression in mammalian cells [33] [32]. |
| Nuclear Localization Signal (NLS) | A short amino acid sequence fused to the Cas9 protein, which acts as a "molecular zip code" to direct the protein through nuclear pores and into the nucleus. | Essential for targeting the Cas9 nuclease to the genomic DNA within the nucleus [33] [32]. |
| sgRNA Expression Cassette | A DNA construct, typically using the U6 small nuclear RNA promoter, to drive high-level expression of the single-guide RNA within the nucleus of mammalian cells. | Ensures robust production of the guide RNA component in the correct cellular compartment [33] [32]. |
| Delivery Vectors (Plasmids) | Engineered DNA plasmids designed to carry both the codon-optimized Cas9-NLS gene and the sgRNA expression cassette into mammalian cells via transfection. | Provides a versatile and accessible method for introducing the CRISPR-Cas9 system into a wide range of eukaryotic cells [5] [32]. |
Quantitative Analysis of Early Editing Efficiency
A key metric for the success of any genome-editing technology is its efficiency—the frequency with which it introduces the desired change at the target locus. The initial 2013 studies reported highly promising and variable efficiencies, which were influenced by the specific genomic target and the type of edit being measured.
The data below summarizes the range of editing efficiencies reported for different types of edits in the foundational 2013 papers. The efficiency of introducing small insertions or deletions (indels) via the Non-Homologous End Joining (NHEJ) repair pathway was often higher than the efficiency of precise Homology-Directed Repair (HDR).
Diagram 2: CRISPR Repair Pathways and 2013 Efficiencies
Table 3: Comparison of Early CRISPR-Cas9 Editing Efficiencies
| Type of Genomic Modification | Cellular Repair Pathway Utilized | Reported Efficiency Range (2013) | Key Factors Influencing Efficiency |
|---|---|---|---|
| Gene Disruption (Knockout) | Non-Homologous End Joining (NHEJ) | 2% to 38% of alleles [32] | Target site accessibility, sgRNA design, chromatin state, cell cycle. |
| Precise Gene Editing (Knock-in) | Homology-Directed Repair (HDR) | Generally lower than NHEJ; up to 38% at specific loci with optimized donor template [32] | Cell cycle stage (preferable in S/G2 phases), design and delivery of the donor DNA template. |
| Multiplex Gene Editing | Concurrent NHEJ and/or HDR at multiple sites | Demonstrated for 2-5 targets simultaneously with high efficiency per target [5] [32] | Efficiency can be similar to single-target editing, but requires careful co-expression of multiple sgRNAs. |
The successful demonstration of CRISPR-Cas9-mediated genome editing in human and mouse cells in early 2013 marked the culmination of a journey from a fundamental observation in bacterial immunity to a transformative biotechnology. The critical innovations of codon-optimization, nuclear localization, and efficient guide RNA expression provided the essential toolkit that allowed researchers to harness this system within the complex environment of the eukaryotic cell. The publication of robust protocols and the immediate validation by multiple groups catalyzed an explosion in adoption and further development across the life sciences. This paradigm shift, firmly established between 2012 and 2013, laid the direct groundwork for the current applications of CRISPR in functional genomics, disease modeling, and the development of groundbreaking gene therapies for once-incurable genetic diseases [34] [35] [32].
Historical Context: From Bacterial Immunity to Genome Engineering
The journey of CRISPR-Cas9 from a bacterial immune mechanism to a revolutionary genome-editing tool began with seminal discoveries spanning three decades. In 1987, unusual repetitive sequences were first observed in Escherichia coli, but their function remained mysterious for years [8]. The pivotal breakthrough came from Francisco Mojica at the University of Alicante, who, by 2005, recognized that these Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and their associated (Cas) genes constituted an adaptive immune system in prokaryotes [8] [5]. He discovered that spacer sequences within CRISPR loci matched viral DNA, suggesting a mechanism for recording and targeting past infections [5].
Parallel research by Alexander Bolotin at the French National Institute for Agricultural Research (INRA) on Streptococcus thermophilus identified a novel Cas protein, Cas9, and noted a consistent sequence motif adjacent to the viral sequences in the genome, later termed the Protospacer Adjacent Motif (PAM) [5]. The functional validation of this adaptive immunity came in 2007 from Rodolphe Barrangou and Philippe Horvath at Danisco, who demonstrated that S. thermophilus could integrate new spacers into its CRISPR array upon phage attack, conferring resistance to future infection [5].
The transformation of this system into a programmable gene-editing tool was propelled by elucidating its molecular mechanism. John van der Oost's group revealed that spacers are transcribed into small CRISPR RNAs (crRNAs) that guide the immune response [8] [5]. In 2011, Emmanuelle Charpentier discovered an essential second RNA, the trans-activating crRNA (tracrRNA), which forms a duplex with crRNA to direct Cas9 [8] [5]. Charpentier, in collaboration with Jennifer Doudna, subsequently simplified the system by fusing crRNA and tracrRNA into a single guide RNA (sgRNA) [5]. This paved the way for the landmark 2013 demonstrations by Feng Zhang and George Church's labs, which successfully harnessed the CRISPR-Cas9 system for precise genome editing in eukaryotic cells [5].
Core Mechanism: sgRNA-Guided DNA Targeting by Cas9
The CRISPR-Cas9 system functions as a programmable DNA-endonuclease complex. The core effector is the Cas9 protein complexed with a designed sgRNA. The sgRNA, through its ~20-nucleotide guide sequence at the 5' end, confers programmability by directing Cas9 to a specific genomic locus via Watson-Crick base pairing [5] [36].
The mechanism proceeds through two critical checkpoints:
- PAM Recognition: Cas9 first scans the DNA for a short Protospacer Adjacent Motif (PAM). For the most commonly used Streptococcus pyogenes Cas9, the PAM is 5'-NGG-3', where 'N' is any nucleotide [5] [36]. PAM binding is essential for initiating the DNA targeting process.
- DNA Melting and R-loop Formation: Upon PAM recognition, Cas9 melts the DNA duplex upstream of the PAM. The sgRNA's guide sequence then invades the DNA duplex to hybridize with the target strand (complementary strand), displacing the non-target strand and forming a structure known as an R-loop [36].
High-speed atomic force microscopy (HS-AFM) studies have visualized the real-time dynamics of this process, showing that the Cas9-sgRNA complex adopts a stable bilobed architecture and interrogates DNA via three-dimensional diffusion [36]. The formation of the R-loop induces a major conformational change in Cas9, activating its nuclease domains.
DNA Cleavage and Nuclease Domains
Cas9 contains two distinct nuclease domains that cleave opposite strands of the target DNA:
- The HNH nuclease domain cleaves the DNA strand that is complementary to the sgRNA (the target strand).
- The RuvC-like nuclease domain cleaves the non-complementary strand (the non-target strand) [5] [36].
These dual cleavages result in a double-strand break (DSB) precisely 3-4 nucleotides upstream of the PAM [5]. The DSB is the foundational event that triggers the cell's endogenous DNA repair machinery, leading to the desired genetic outcomes.
Cellular Repair Pathways: NHEJ and HDR
The double-strand break generated by Cas9 is primarily repaired by one of two competing endogenous cellular pathways: Non-Homologous End Joining (NHEJ) or Homology-Directed Repair (HDR). The balance between these pathways determines the final editing outcome [37] [38].
Non-Homologous End Joining (NHEJ)
NHEJ is an error-prone, template-independent repair pathway that is active throughout the cell cycle and often dominates the repair process [37] [38].
- Mechanism: The broken DNA ends are directly ligated without a homologous template.
- Outcome: This process frequently results in small random insertions or deletions (indels) at the cleavage site. When these indels occur within a protein-coding exon, they can cause a frameshift mutation, leading to a gene knockout [38].
- Applications: NHEJ is ideally suited for experiments where the goal is to disrupt gene function.
Homology-Directed Repair (HDR)
HDR is a precise, template-dependent repair pathway that is primarily active in the S and G2 phases of the cell cycle [38].
- Mechanism: HDR uses a homologous DNA template to accurately repair the break. Researchers can exploit this by co-delivering a donor DNA template containing the desired modification (e.g., a point mutation, tag, or reporter gene) flanked by homology arms.
- Outcome: The genetic information from the donor template is copied into the genomic locus, resulting in a precise edit.
- Applications: HDR is used for precise gene knock-ins, specific nucleotide substitutions, and the creation of reporter cell lines [38].
A third pathway, Microhomology-Mediated End Joining (MMEJ), can also be engaged, particularly under certain conditions. MMEJ relies on short microhomology sequences (5-25 bp) flanking the DSB and typically results in larger, more predictable deletions [37].
Table 1: Key Characteristics of DNA Double-Strand Break Repair Pathways
| Feature | Non-Homologous End Joining (NHEJ) | Homology-Directed Repair (HDR) | Microhomology-Mediated End Joining (MMEJ) |
|---|---|---|---|
| Template | Not required | Required (donor DNA with homology arms) | Uses microhomology regions flanking the DSB |
| Fidelity | Error-prone (generates indels) | High-fidelity, precise | Imprecise (generates predictable deletions) |
| Primary Outcome | Gene knockout | Precise gene editing (knock-in, point mutations) | Larger, specific deletions |
| Cell Cycle Phase | Active throughout | Primarily S/G2 phases | Not well defined |
| Dominance | Dominant in most contexts | Typically less frequent | Can be promoted by specific Cas9 variants [37] |
Advanced Engineering: Biasing Repair Outcomes
A significant challenge in CRISPR-mediated genome editing is the inherent competition between repair pathways, where NHEJ is often dominant. Recent research has focused on strategies to bias this engagement toward more precise outcomes [37].
A groundbreaking approach involves engineering the Cas9 protein itself to alter the fundamental nature of the DNA break it creates. It was discovered that the structure of the DNA break (blunt vs. staggered ends) is a critical determinant of which repair pathway is engaged [37].
Engineered Cas9 Variants (e.g., vCas9)
By mutating specific residues at the Cas9-DNA interface (e.g., R976 and K1003), researchers have created variants that no longer produce blunt-end DSBs. Instead, these engineered nucleases, such as the quadruple mutant vCas9 (S55R-R976A-K1003A-T1314R), produce staggered DNA breaks with 5' overhangs of 6 base pairs or more [37].
- Mechanism: This altered break structure suppresses the classical NHEJ pathway.
- Outcome: It instead favors repair through pathways that utilize homologous sequences, specifically MMEJ and HDR. Consequently, vCas9 enables efficient precise editing while significantly suppressing imprecise indels caused by NHEJ, a finding demonstrated in both dividing and non-dividing cells [37].
This establishes a new paradigm of "custom-designed" nucleases intrinsically biased toward specific mutational applications, moving beyond reliance on external manipulation of cellular states [37].
Table 2: Comparison of Wild-Type and Engineered vCas9
| Parameter | Wild-Type Cas9 | Engineered vCas9 |
|---|---|---|
| DNA Break Structure | Blunt ends | Staggered ends (≥6 bp 5' overhangs) |
| Dominant Repair Pathway | Non-Homologous End Joining (NHEJ) | MMEJ and HDR |
| Primary Editing Outcome | High frequency of indels | Enhanced precise editing, suppressed indels |
| Total Editing Activity | High | Can be lower, but rescued in active variants (e.g., vCas9) [37] |
| Therapeutic Application | Gene disruption (knockout) | Precise gene correction (knock-in) |
The Scientist's Toolkit: Essential Reagents and Methodologies
Research Reagent Solutions
Table 3: Essential Reagents for CRISPR-Cas9 Experiments
| Reagent / Material | Function and Application |
|---|---|
| Cas9 Nuclease | The effector protein that creates the double-strand break. Can be wild-type for general editing, or engineered variants like vCas9 for biased repair outcomes [37]. |
| sgRNA Expression Construct | A plasmid or synthetic RNA that encodes the single-guide RNA, providing both targeting specificity (via the 20-nt guide) and scaffold structure for Cas9 binding. |
| HDR Donor Template | A DNA molecule (single-stranded oligodeoxynucleotide - ssODN, or double-stranded plasmid) containing the desired edit flanked by homology arms. Essential for introducing precise mutations via HDR [38]. |
| Delivery Vehicle (e.g., Lentivirus, Electroporation System) | Methods to introduce CRISPR components into target cells. The choice depends on cell type (e.g., dividing, non-dividing, primary cells) and efficiency requirements. |
| NHEJ Inhibitors (e.g., Scr7) | Small molecules that can be used to transiently inhibit the NHEJ pathway, thereby relatively increasing the frequency of HDR. An external method to bias repair [37]. |
Protocol: Assessing DNA Break Structure and Repair Bias
This methodology, adapted from [37], allows for the empirical determination of DNA break structures generated by different Cas9 variants and their consequent impact on repair pathway engagement.
Dual DSB Induction:
- Design two sgRNAs targeting nearby sites (e.g., within 50-100 bp) at a model locus (e.g., EMX1 or CXCR4 in HEK293T cells).
- Co-transfect cells with plasmids expressing the Cas9 variant of interest (e.g., wild-type, R976A, vCas9) and the two sgRNAs.
Junction Analysis:
- After 48-72 hours, harvest genomic DNA and amplify the target region via PCR.
- Subject the PCR amplicons to deep sequencing.
- Analyze the sequence data: The sequences of the junctions between the two cut sites will reveal whether the cuts were blunt or staggered. The presence of overhangs of specific lengths indicates a staggered break [37].
Concomitant Repair Outcome Analysis:
- In parallel transfections, include a donor HDR template designed to introduce a specific sequence change (e.g., a BFP-to-GFP conversion or a small restriction site).
- Using the same deep sequencing data, quantify the frequency of precise HDR edits versus imprecise indels (a proxy for NHEJ/MMEJ activity) for each Cas9 variant.
Data Interpretation:
- Correlate the observed DNA break structure (from Step 2) with the measured repair pathway frequencies (from Step 3).
- Expected Result: Cas9 variants that produce larger staggered cuts (like vCas9) will show a strong correlation with increased precise editing frequency and a shift from NHEJ to MMEJ/HDR [37].
The approval of CASGEVY (exagamglogene autotemcel), known more commonly as exa-cel, represents a watershed moment in molecular medicine, culminating a decades-long journey from fundamental bacterial immunology to therapeutic genome editing. As the first FDA-approved CRISPR-based therapy, Casgevy treats two inherited hemoglobinopathies: sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TDT) in patients 12 years and older [39] [40]. This approval signals the clinical maturation of CRISPR-Cas9 technology, which was originally discovered as an adaptive immune system in prokaryotes that protects against viral invaders by storing fragments of viral DNA and using them to guide targeted cleavage of subsequent infections [8] [3]. The transformation of this bacterial defense mechanism into a precision gene-editing tool, often termed "genetic scissors," earned researchers Emmanuelle Charpentier and Jennifer Doudna the Nobel Prize in Chemistry in 2020 [8]. This article traces the scientific and clinical development of Casgevy, providing an in-depth technical guide to its mechanism, efficacy, and implementation within the broader context of CRISPR history.
Historical Foundation: The CRISPR-Cas9 Discovery Pathway
The development of CRISPR-Cas9 into a programmable genome-editing tool was built upon foundational discoveries made by numerous research groups across the globe. The timeline below charts the key milestones from initial observation of repetitive sequences in bacteria to the demonstration of CRISPR-mediated genome editing in human cells.
Figure 1: History of Key CRISPR Discoveries from 1987-2013
The Natural Biology of CRISPR
The biological function of CRISPR-Cas systems in prokaryotes provided the blueprint for all subsequent therapeutic applications. Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) loci, together with CRISPR-associated (Cas) genes, function as an adaptive immune system that confers resistance to foreign genetic elements such as plasmids and phages [3]. The system operates by incorporating short sequences of invading DNA as "spacers" between repeated sequences in the CRISPR array. Upon re-exposure, these spacers are transcribed into short CRISPR RNA (crRNA) molecules that guide Cas proteins to cleave complementary foreign DNA sequences [8] [5]. The discovery of the protospacer adjacent motif (PAM), a short DNA sequence adjacent to the target site that is required for recognition, was crucial for understanding targeting specificity [5].
Transformation into a Programmable Tool
The critical breakthrough for genome editing came when researchers recognized that the Type II CRISPR system from Streptococcus pyogenes could be simplified and repurposed. This system requires only the Cas9 nuclease and a guide RNA for targeted DNA cleavage [5]. In 2012, Charpentier and Doudna's teams demonstrated that the naturally occurring dual-RNA structure (crRNA and trans-activating crRNA, or tracrRNA) could be engineered into a single-guide RNA (sgRNA) [5] [3]. This created a two-component system where the sgRNA could be easily programmed to direct Cas9 to any DNA sequence adjacent to a PAM, typically 5'-NGG-3' [3]. This programmable nature, coupled with the ability to create double-strand breaks in DNA, enabled researchers to harness the cell's own repair mechanisms—either non-homologous end joining (NHEJ) or homology-directed repair (HDR)—to introduce precise genetic modifications [8].
Mechanism of Action: Precision Editing of BCL11A Enhancer
Casgevy employs a highly specific mechanism that mimics a natural benign condition known as hereditary persistence of fetal hemoglobin (HPFH) to address the root cause of sickle cell disease and beta thalassemia [41]. The therapeutic approach involves ex vivo genome editing of autologous CD34+ hematopoietic stem and progenitor cells (HSPCs) to disrupt an erythroid-specific enhancer region of the BCL11A gene, a transcriptional repressor of fetal hemoglobin (HbF) [39] [41].
Figure 2: Casgevy Therapeutic Workflow from Cell Collection to Therapeutic Effect
Molecular Mechanism of BCL11A Disruption
At the molecular level, the Casgevy editing process utilizes the CRISPR-Cas9 ribonucleoprotein (RNP) complex introduced into CD34+ cells via electroporation [41]. The engineered sgRNA directs the Cas9 enzyme to create a precise double-strand break in the erythroid-specific enhancer region of BCL11A [41]. This targeted disruption is designed to reduce BCL11A expression specifically in the erythroid lineage, thereby minimizing potential off-target effects in other cell types [41]. When the cell repairs this break through the error-prone NHEJ pathway, small insertions or deletions (indels) are introduced, effectively disrupting the enhancer function and reducing BCL11A expression [41]. The subsequent reduction in BCL11A, a key repressor of gamma-globin expression, leads to reactivation of fetal hemoglobin (HbF) production in red blood cells [39] [41].
Physiological Consequence in Hemoglobinopathies
The increased HbF production addresses the fundamental pathophysiology of both SCD and TDT through distinct mechanisms:
In Sickle Cell Disease: Elevated HbF reduces the intracellular concentration of sickle hemoglobin (HbS), which prevents hemoglobin polymerization and subsequent sickling of red blood cells under deoxygenating conditions [41]. This reduces vaso-occlusive crises (VOCs) by maintaining normal red blood cell morphology and blood flow [39] [41].
In Transfusion-Dependent Beta Thalassemia: Increased γ-globin production compensates for the deficient β-globin chains, improving the α-globin to non-α-globin chain balance and reducing ineffective erythropoiesis and hemolysis [41]. The resulting increase in total hemoglobin levels and improved red blood cell survival decreases or eliminates the need for regular transfusions [42].
Clinical Development and Efficacy Data
The approval of Casgevy was supported by robust clinical evidence from multiple trials demonstrating significant and sustained clinical benefits for patients with SCD and TDT.
Table 1: Efficacy Outcomes from Casgevy Clinical Trials in Sickle Cell Disease and Transfusion-Dependent Beta Thalassemia
| Parameter | Sickle Cell Disease Trial | Transfusion-Dependent Beta Thalassemia Trial |
|---|---|---|
| Primary Endpoint | Freedom from severe VOCs for ≥12 consecutive months during 24-month follow-up [39] | Complete resolution of VOEs (VOE-CR) between 6 and 18 months after infusion [39] |
| Patient Population | Patients 12 years and older with history of ≥2 severe VOCs/year [39] | Patients 12-50 years with history of VOEs [39] |
| Efficacy Results | 29 of 31 evaluable patients (93.5%) achieved primary endpoint [39] | 28 of 32 patients (88%) achieved VOE-CR [39] |
| Key Secondary Outcomes | All treated patients achieved successful engraftment; no graft failure/rejection [39] | Not specified in available sources |
| Follow-up Duration | 24 months [39] | 24 months [39] |
Clinical Trial Design and Patient Monitoring
The clinical development program for Casgevy employed single-arm, multi-center trials with careful patient selection and monitoring [39]. For the SCD trial, eligible patients were required to have a history of at least two protocol-defined severe vaso-occlusive crises (VOCs) during each of the two years prior to screening [39]. Similarly, the TDT trial enrolled patients with a documented history of vaso-occlusive events [39]. All patients underwent myeloablative conditioning with busulfan to clear bone marrow space before infusion of the edited cells [39] [41]. Patients were monitored for engraftment, adverse events, and the presence of edited cells in peripheral blood and bone marrow. The trials included long-term follow-up studies to evaluate both safety and effectiveness over an extended period [39].
Technical Protocol: From Cell Collection to Patient Infusion
The manufacturing and administration of Casgevy involves a multi-step, technically complex process that requires specialized facilities and expertise in stem cell transplantation.
Manufacturing Process
Cell Collection and Mobilization: CD34+ hematopoietic stem and progenitor cells are collected from the patient via apheresis after mobilization with mobilization agents [41] [42]. For patients with SCD, granulocyte-colony stimulating factor (G-CSF) is not used for mobilization due to the risk of triggering vaso-occlusive crises [43].
CRISPR-Cas9 Genome Editing: The collected CD34+ cells are transfected with the CRISPR-Cas9 ribonucleoprotein complex targeting the BCL11A erythroid-specific enhancer region using electroporation [41]. This non-viral delivery method enhances safety by avoiding the potential insertional mutagenesis associated with viral vectors [41].
Quality Control and Expansion: The edited cells undergo rigorous quality control testing, including assessments of viability, potency, and purity, before cryopreservation [42]. The entire manufacturing process may take up to six months from cell collection to final product release [42].
Patient Treatment Protocol
Pre-conditioning: Patients receive myeloablative conditioning with busulfan to create marrow space for the edited cells [41] [43]. This step is essential for successful engraftment but carries significant risks, including prolonged cytopenias and increased susceptibility to infections [39] [41].
Product Infusion: The cryopreserved Casgevy product is thawed and administered as a one-time intravenous infusion via a central venous catheter [43]. The minimum recommended dose is 3 × 10^6 CD34+ cells per kilogram of body weight [43].
Engraftment and Recovery: Patients require close monitoring in a specialized facility until neutrophil and platelet engraftment occurs, typically within 4-6 weeks [41] [42]. During this period, patients need comprehensive supportive care, including infection prophylaxis and management of conditioning-related toxicities [39].
Safety Profile and Risk Management
The safety assessment of Casgevy has revealed a predictable side effect profile consistent with myeloablative conditioning and hematopoietic stem cell transplantation.
Table 2: Adverse Events and Risk Management in Casgevy Treatment
| Adverse Event | Frequency | Clinical Management |
|---|---|---|
| Low platelet levels | Very common [39] [41] | Monitor platelet counts until engraftment; transfuse as needed; monitor for bleeding [41] |
| Low white blood cell levels | Very common [39] [41] | Monitor absolute neutrophil counts; manage infections per guidelines [41] |
| Mouth sores | Very common [39] | Supportive care with pain management and nutritional support |
| Febrile neutropenia | Common [39] | Prompt antibiotic therapy and fever management |
| Hypersensitivity reactions | Potential risk [41] | Premedication and monitoring during infusion for DMSO-related reactions |
| Delayed platelet engraftment | Observed [41] | Extended monitoring and platelet transfusion support |
Long-Term Safety Considerations
While the edited cells in Casgevy are extensively tested for off-target editing during manufacturing, the risk of unintended, off-target editing cannot be completely ruled out due to individual genetic variations [41]. The clinical significance of potential off-target editing remains unknown [41]. Additionally, as with all gene therapies, long-term monitoring is essential to identify any delayed adverse events. Patients receiving Casgevy are enrolled in long-term follow-up studies to monitor for potential long-term risks, including hematologic malignancy [39]. It is also recommended that patients do not donate blood, organs, tissues, or cells at any time in the future after treatment [42].
The development and implementation of Casgevy relies on a sophisticated array of biological reagents, manufacturing processes, and analytical tools.
Table 3: Research Reagent Solutions for CRISPR-Based Therapeutic Development
| Reagent/Resource | Function in Casgevy Development | Technical Specifications |
|---|---|---|
| CRISPR-Cas9 RNP Complex | Precise editing of BCL11A enhancer | Cas9 enzyme + sgRNA targeting BCL11A erythroid-specific enhancer; delivered via electroporation [41] |
| CD34+ Hematopoietic Stem Cells | Target cell population for editing | Autologous cells collected via apheresis after mobilization; minimum dose 3×10^6 cells/kg [41] [43] |
| Electroporation System | Non-viral delivery of RNP complex | Enables efficient intracellular delivery of CRISPR components without viral vectors [41] |
| Myeloablative Conditioning Agents | Create marrow niche for engraftment | Busulfan-based regimen; requires careful pharmacokinetic monitoring [41] [43] |
| Cryopreservation Medium | Long-term storage of cell product | Contains 5% dimethyl sulfoxide (DMSO) and dextran 40 [43] |
| GMP-compliant sgRNAs | Clinical-grade guide RNA production | High-purity, documented sgRNAs meeting Good Manufacturing Practice standards [44] |
The approval of Casgevy represents a transformative advancement in genetic medicine, demonstrating that CRISPR-based therapies can successfully transition from theoretical concept to clinical reality. This milestone builds upon decades of fundamental research into bacterial immunity and represents the culmination of efforts by countless researchers to harness CRISPR-Cas9 as a precise genome-editing tool. While challenges remain—including the complexity and cost of treatment, need for specialized medical centers, and long-term safety monitoring—Casgevy has established a new paradigm for addressing genetic diseases at their molecular root. As the field progresses, ongoing research aims to simplify delivery methods, improve targeting specificity, and expand the range of addressable genetic disorders. The journey from bacterial immunity to approved therapy exemplifies how fundamental biological research can yield unexpected and powerful clinical applications, offering new hope for patients with previously untreatable genetic conditions.
The journey of CRISPR from a curious bacterial sequence to a revolutionary therapeutic tool represents one of the most significant advancements in modern biotechnology. Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) were first identified in 1987 in Escherichia coli but their function remained mysterious for decades [8]. Francisco Mojica, working at the University of Alicante in Spain, was the first researcher to characterize what we now recognize as CRISPR loci and, in 2000, he recognized that disparate repeat sequences shared common features [5]. His critical insight came in 2005 when he reported that these sequences matched snippets from bacteriophage genomes, leading him to correctly hypothesize that CRISPR constitutes an adaptive immune system in prokaryotes [8] [5].
The subsequent decade witnessed rapid elucidation of the molecular mechanisms, culminating in the groundbreaking 2012 demonstration that the CRISPR-Cas9 system could be programmed for precise DNA cleavage in vitro [5]. This set the stage for the first demonstrations of CRISPR-mediated genome editing in eukaryotic cells in 2013 [5]. The remarkable efficiency and programmability of CRISPR-based systems have since propelled them to the forefront of therapeutic development, with the first CRISPR-based medicine, Casgevy (exagamglogene autotemcel), receiving regulatory approval in 2023 for sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT) [12] [45]. As of 2025, the global gene editing landscape has expanded dramatically, with more than 3,200 gene, cell, and RNA therapy trials underway worldwide [45].
Technical Foundations of Gene Editing Platforms
Evolution of Programmable Nucleases
Therapeutic genome editing relies on technologies that enable precise modifications to the human genome through addition, excision, or modification of specific genes [11]. Three foundational platforms have been developed, each with distinct mechanisms and characteristics [11].
Table 1: Comparison of Major Genome Editing Platforms
| Platform | DNA-Binding Domain Origin | Nuclease Domain | Recognition Mechanism | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| ZFNs | Zinc finger proteins (eukaryotes) | FokI restriction enzyme | Protein-DNA interaction (3 bp per finger) | High specificity due to dimer requirement | Complex design; high cost; potential off-target effects |
| TALENs | Transcription activator-like effectors (Xanthomonas bacteria) | FokI restriction enzyme | Protein-DNA interaction (1 bp per repeat) | Modular design; high binding affinity | Large protein size; challenging genetic construction |
| CRISPR-Cas9 | Bacterial adaptive immune system | Cas9 nuclease | RNA-DNA complementarity (20 bp guide RNA) | Easy programmability; multiplexing capability | PAM sequence requirement; off-target concerns |
CRISPR-Cas System Mechanism
The type II CRISPR-Cas9 system requires two key components: the Cas9 nuclease and a guide RNA (gRNA) that combines the functions of CRISPR RNA (crRNA) and trans-activating CRISPR RNA (tracrRNA) [8] [11]. The system operates through a precise molecular mechanism:
- gRNA-Cas9 Complex Formation: The single-guide RNA (sgRNA) complexes with the Cas9 enzyme, forming a ribonucleoprotein complex [11].
- PAM-Dependent Target Recognition: The complex scans DNA for the Protospacer Adjacent Motif (PAM) sequence (5'-NGG-3' for Streptococcus pyogenes Cas9) [8] [11].
- DNA Melting and Strand Invasion: Upon PAM binding, local DNA melting occurs, allowing the sgRNA to invade and test for complementarity [11].
- Double-Strand Break Formation: With sufficient complementarity, the Cas9 HNH domain cleaves the complementary strand and the RuvC domain cleaves the non-complementary strand [11].
The resulting double-strand break (DSB) activates cellular DNA repair pathways, primarily error-prone non-homologous end joining (NHEJ) leading to gene knockouts, or the more precise homology-directed repair (HDR) for specific gene corrections [11].
Advanced Gene Editing Technologies
Beyond standard CRISPR-Cas9, newer platforms have emerged that expand therapeutic possibilities:
Base Editing: This technology uses a catalytically impaired Cas protein (nickase) fused to a single-strand DNA-modifying enzyme, such as cytidine deaminase or adenine deaminase [11]. Cytidine base editors (CBEs) convert C•G to T•A base pairs, while adenine base editors (ABEs) convert A•T to G•C base pairs [11]. Crucially, base editors do not create double-strand breaks, reducing unintended indels and making them particularly valuable for correcting point mutations associated with genetic diseases [11].
Prime Editing: Considered a "search-and-replace" genome editing technology, prime editing uses a Cas9 nickase fused to a reverse transcriptase and a prime editing guide RNA (pegRNA) that specifies the target site and encodes the desired edit [11]. This system can mediate all 12 possible base-to-base conversions, as well as small insertions and deletions, without requiring double-strand breaks or donor DNA templates [11].
Therapeutic Delivery Systems
Effective delivery remains one of the most significant challenges in gene editing therapeutics. Current approaches can be broadly categorized into viral and non-viral methods, each with distinct advantages and limitations.
Table 2: Comparison of Major Delivery Systems for Gene Editing Therapeutics
| Delivery System | Mechanism | Therapeutic Approach | Key Advantages | Key Limitations | Clinical Examples |
|---|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Encapsulate editing components in lipid bilayers for cellular uptake | Primarily in vivo | Low immunogenicity; potential for redosing; organ-targeted versions in development | Primarily targets liver; limited payload capacity | CTX310, CTX320, VERVE-102, NTLA-2001 [12] [46] [47] |
| Adeno-Associated Virus (AAV) | Viral vector delivers genetic material encoding editors | In vivo | High transduction efficiency; broad tissue tropism | Pre-existing immunity; limited payload capacity; immunogenicity | HG-302 (packaged in single AAV) [46] |
| Electroporation | Electrical pulses create temporary pores in cell membranes | Ex vivo | High efficiency for hard-to-transfect cells | Only applicable to ex vivo approaches; cell damage concerns | CASGEVY (ex vivo editing of CD34+ cells) [12] |
| Viral Vectors (Lentiviral, Adenoviral) | Viral vectors for ex vivo modification | Ex vivo | Stable gene transfer; high efficiency | Insertional mutagenesis concerns; immunogenicity | CTX112, CTX131 (CAR T cells) [48] [47] |
The choice of delivery system significantly influences the therapeutic approach. Ex vivo strategies involve extracting patient cells, editing them in a controlled laboratory environment, and reinfusing them into the patient [12] [46]. This approach offers precise control over editing efficiency and safety but requires complex manufacturing and conditioning regimens [12]. In contrast, in vivo strategies deliver editing components directly to target cells within the patient's body, offering a simpler treatment paradigm but facing greater challenges in targeting and safety assessment [12] [46].
Clinical Trial Landscape Across Therapeutic Areas
Hematologic and Genetic Disorders
The most advanced gene editing therapeutics target hematologic and genetic disorders, with multiple candidates now in late-stage development.
Hemoglobinopathies: CASGEVY represents the pioneering success in this category. This non-viral, ex vivo CRISPR/Cas9 gene-edited cell therapy is approved for eligible patients with sickle cell disease (SCD) or transfusion-dependent beta thalassemia (TDT) [49]. The therapy involves editing the BCL11A gene in autologous CD34+ hematopoietic stem cells to increase fetal hemoglobin production, thereby compensating for the defective adult hemoglobin [12]. As of September 2025, approximately 165 patients have completed their first cell collection, with 39 patients receiving infusions globally [49]. Pediatric development is advancing, with enrollment completed in global Phase 3 studies for children aged 5-11 years [49].
Rare Genetic Disorders: Intellia Therapeutics' NTLA-2001 (nexiguran ziclumeran) represents a breakthrough as the first systemically administered CRISPR therapy to enter clinical trials [12]. This in vivo therapy targets the TTR gene for the treatment of transthyretin amyloidosis (ATTR) and is currently in global Phase 3 trials (MAGNITUDE trial, NCT06128629) [46]. The treatment uses lipid nanoparticles (LNPs) to deliver CRISPR components to the liver, resulting in rapid, deep (~90% reduction), and durable reduction of TTR protein levels [12]. All 27 participants who reached two years of follow-up showed sustained response with no evidence of waning effect [12].
Cardiovascular and Metabolic Diseases
Gene editing approaches for cardiovascular disease focus on modulating lipid metabolism to reduce atherosclerotic risk.
ANGPTL3-Targeting Therapies: CRISPR Therapeutics' CTX310 targets the ANGPTL3 gene to regulate LDL and triglyceride levels [47]. Phase 1 data presented in 2025 demonstrated dose-dependent decreases, with peak reductions of up to 82% in triglycerides and 81% in LDL [47] [49]. The therapy has been well-tolerated with no treatment-related severe adverse events [47]. CRISPR Therapeutics is advancing CTX310 into Phase 1b trials, prioritizing development in severe hypertriglyceridemia (sHTG) and mixed dyslipidemia [49].
PCSK9-Targeting Therapies: Verve Therapeutics has pioneered base editing approaches for cardiovascular disease. VERVE-101 and VERVE-102 use adenine base editing to permanently inactivate the PCSK9 gene in the liver [46]. While VERVE-101 enrollment was paused due to laboratory abnormalities, preliminary results for VERVE-102 showed the therapy has been well-tolerated in the first two dose cohorts [46].
Lp(a)-Targeting Therapies: CRISPR Therapeutics' CTX320 targets the LPA gene to reduce lipoprotein(a) levels, a genetically determined risk factor for major adverse cardiovascular events [47] [49]. Elevated Lp(a) affects up to 20% of the global population and remains unaddressed by current therapies [49]. The Phase 1 trial is ongoing with an update expected in the first half of 2026 [49].
Table 3: Selected Cardiovascular Gene Editing Therapies in Clinical Development
| Therapy | Target | Editing Approach | Delivery | Developer | Phase | Key Results |
|---|---|---|---|---|---|---|
| CTX310 | ANGPTL3 | CRISPR-Cas9 knockout | LNP | CRISPR Therapeutics | Phase 1b | Up to 82% TG reduction, 81% LDL reduction; well-tolerated [47] [49] |
| VERVE-102 | PCSK9 | Adenine Base Editing | GalNAc-LNP | Verve Therapeutics | Phase 1b | Well-tolerated in initial cohorts; no serious adverse events [46] |
| CTX320 | LPA | CRISPR-Cas9 knockout | LNP | CRISPR Therapeutics | Phase 1 | Update expected H1 2026 [49] |
| VERVE-201 | ANGPTL3 | Gene editing | GalNAc-LNP | Verve Therapeutics | Phase 1b | First patient dosed November 2024 [46] |
Oncology and Immuno-Oncology
Gene editing approaches in oncology primarily focus on engineering immune cells to enhance antitumor activity.
Next-Generation CAR T Therapies: CRISPR Therapeutics is developing allogeneic (off-the-shelf) CAR T product candidates, CTX112 (targeting CD19) and CTX131 (targeting CD70) [47] [49]. These candidates incorporate novel potency edits that lead to significantly higher CAR T cell expansion and cytotoxicity [47]. CTX112 has received Regenerative Medicine Advanced Therapy (RMAT) designation from the FDA for relapsed or refractory follicular lymphoma and marginal zone lymphoma [47] [49]. A Phase 1 clinical trial in autoimmune diseases (including systemic lupus erythematosus, systemic sclerosis, and inflammatory myositis) is also underway [49].
Other Therapeutic Areas
Hereditary Angioedema: Intellia Therapeutics' NTLA-2002 uses CRISPR-Cas9 delivered via LNP to disable the KLKB1 gene in vivo, reducing plasma kallikrein levels [12] [46]. Phase I/II results showed an average of 86% reduction in kallikrein and a significant reduction in the number of attacks, with 8 of 11 participants in the higher dose group being attack-free in the 16-week period after treatment [12].
Duchenne Muscular Dystrophy: HuidaGene Therapeutics' HG-302 uses a novel engineered Cas12 nuclease (hfCas12Max) to induce exon skipping in the DMD gene [46]. The compact hfCas12Max allows packaging in a single AAV vector for in vivo delivery to muscle tissue [46]. The first patient was dosed in December 2024 in the MUSCLE clinical trial [46].
Type 1 Diabetes: CRISPR Therapeutics' CTX211 (VCTX210A) is an immune-evasive, stem cell-derived beta-cell replacement therapy for Type 1 diabetes [46]. This ex vivo approach uses CRISPR-Cas9 to edit healthy donor cells to enhance their fitness and allow them to evade the host immune system before transplantation [46]. The Phase I/II trial is testing the therapy in up to 40 patients and is estimated to be completed in August 2025 [46].
The Scientist's Toolkit: Essential Research Reagents
Successful gene editing therapeutics development relies on a comprehensive suite of research reagents and technologies.
Table 4: Essential Research Reagents for Gene Editing Therapeutics
| Reagent/Technology | Function | Therapeutic Application Examples |
|---|---|---|
| Cas9 Nucleases | RNA-guided DNA endonuclease creating double-strand breaks | CASGEVY (BCL11A gene editing in HSCs) [12] |
| Base Editors (ABE/CBE) | Chemically converts one DNA base to another without DSBs | VERVE-101, VERVE-102 (PCSK9 inactivation) [46] |
| Lipid Nanoparticles (LNPs) | In vivo delivery of mRNA/gRNA editing components | CTX310, NTLA-2001 (liver-targeted delivery) [12] [47] |
| AAV Vectors | In vivo delivery of editing machinery genetic code | HG-302 (muscle-targeted delivery for DMD) [46] |
| Guide RNA (gRNA) | Targets Cas protein to specific genomic loci | All CRISPR-based therapies require optimized gRNAs [11] |
| Electroporation Systems | Ex vivo delivery of editing components to cells | CASGEVY (CD34+ HSC editing) [12] |
| Anti-CD117 (c-Kit) ADC | Targeted conditioning agent for HSC transplantation | Next-generation approaches for SCD/TDT (preclinical) [47] |
| Prime Editors | Search-and-replace editing with minimal byproducts | Preclinical development for precise corrections [11] |
Current Challenges and Future Directions
Despite remarkable progress, the field faces several significant challenges. Delivery efficiency remains a primary constraint, particularly for tissues beyond the liver [12] [48]. While LNPs naturally accumulate in the liver, researchers are working on versions with affinity for different organs [12]. Manufacturing complexity presents another hurdle, especially for ex vivo therapies like CASGEVY that require specialized authorized treatment centers and complex logistics [12] [49].
The high cost of gene editing therapies creates accessibility challenges [12]. However, progress is being made on reimbursement agreements with healthcare systems, such as the NHS in the UK [12] [47]. Safety concerns including off-target effects and immune responses to editing components or delivery vehicles continue to require careful assessment [11].
Future directions include next-generation editing platforms like prime editing that offer greater precision, targeted conditioning regimens to reduce the toxicity of hematopoietic stem cell transplantation, and in vivo approaches that could eliminate the need for ex vivo manipulation entirely [47] [49]. The successful case of Baby KJ, who received a personalized in vivo CRISPR treatment for CPS1 deficiency developed in just six months, points toward a future of on-demand gene editing therapies for rare genetic diseases [12].
However, the field also faces macroeconomic challenges. Recent reductions in venture capital investment and proposed cuts to US government science funding threaten to slow the pace of discovery and therapeutic development [12]. The National Science Foundation funding has been cut in half, with funding for undergraduate science education cut by 71%, and a 40% budget cut for the National Institutes of Health has been proposed [12]. These financial pressures have led to significant layoffs in CRISPR-focused companies and could dramatically impact the speed and quantity of future biomedical research [12].
The clinical landscape of gene editing in 5 represents a maturing field transitioning from theoretical promise to therapeutic reality. With over 3,200 gene, cell, and RNA therapy trials underway globally [45], the field has expanded far beyond initial proof-of-concept studies to address diverse therapeutic areas including hematologic, cardiovascular, metabolic, and infectious diseases. The success of CASGEVY has established a crucial precedent, while next-generation approaches like base editing and advanced delivery systems are addressing previous limitations.
The journey from Francisco Mojica's initial observations of strange bacterial repeats to transformative human therapies exemplifies how fundamental biological research can drive medical revolution. As the field addresses ongoing challenges in delivery, specificity, and accessibility, gene editing technologies appear poised to become increasingly central to therapeutic development across medicine. The coming decade will likely witness further expansion into common complex diseases, improved delivery platforms, and potentially one-time curative treatments for previously intractable genetic disorders.
The journey of CRISPR from a curious bacterial sequence to a revolutionary gene-editing technology represents one of the most significant advancements in modern biotechnology. Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) originated as an adaptive immune system in prokaryotes, protecting bacteria and archaea from viral invaders by storing fragments of viral DNA as "spacers" in their own genomes [8] [3]. This natural system enabled organisms to recognize and cleave foreign genetic material upon subsequent infections, providing a form of heritable immunity [3]. The transformation of this bacterial defense mechanism into a precise genome-editing tool culminated in the 2020 Nobel Prize in Chemistry, awarded to Emmanuelle Charpentier and Jennifer Doudna for developing the CRISPR-Cas9 "genetic scissors" [8].
The transition from laboratory tool to therapeutic application has hinged on solving one fundamental challenge: delivery. While viral vectors initially dominated gene therapy approaches, their limitations—including immunogenicity, limited payload capacity, and potential for insertional mutagenesis—prompted the search for alternatives [50]. Lipid nanoparticles (LNPs) have emerged as the transformative platform enabling systemic therapeutic delivery, offering a non-viral approach that combines efficacy with reduced safety concerns [51]. This technical guide examines how LNP-based delivery systems are revolutionizing in vivo CRISPR applications by providing targeted, efficient, and safe delivery of gene-editing components throughout the body.
Historical Foundations: The CRISPR-Cas Evolution
The development of CRISPR-Cas systems follows a trajectory of discovery spanning nearly four decades, with key insights emerging from diverse scientific disciplines and research groups worldwide. The table below chronicles the pivotal milestones in this journey.
Table 1: Key Historical Milestones in CRISPR-Cas Development
| Year | Discovery | Key Researchers/Teams | Significance |
|---|---|---|---|
| 1987 | Initial observation of CRISPR sequences | Ishino et al. [8] | First documentation of unusual repetitive DNA structures in E. coli |
| 1993-2005 | Characterization of CRISPR function | Mojica et al. [5] | Recognized CRISPR as an adaptive immune system with sequences derived from phages |
| 2005 | Identification of Cas9 and PAM | Bolotin et al. [5] | Discovered Cas9 protein and protospacer adjacent motif (PAM) requirement |
| 2007 | Experimental proof of adaptive immunity | Barrangou, Horvath et al. [8] [5] | Demonstrated CRISPR provides acquired resistance against viruses in prokaryotes |
| 2011 | Discovery of tracrRNA | Charpentier et al. [8] [5] | Identified trans-activating crRNA essential for Cas9 function |
| 2012 | CRISPR-Cas9 as programmable tool | Doudna, Charpentier, Šikšnys et al. [8] [5] | Reconstituted system in vitro; created single-guide RNA (sgRNA) |
| 2013 | Genome editing in eukaryotic cells | Zhang, Church et al. [5] | First demonstration of CRISPR editing in human and mouse cells |
The following diagram illustrates the logical progression from basic scientific discovery to therapeutic application, highlighting the interconnected milestones that enabled the current LNP-delivered CRISPR era:
Technical Foundations of Lipid Nanoparticles
LNP Composition and Mechanism of Action
Lipid nanoparticles represent a sophisticated delivery platform composed of precisely engineered lipid components that self-assemble into stable, nucleic acid-loaded particles typically measuring 50-120 nm in diameter [51]. The formulation of LNPs for CRISPR delivery requires four primary lipid components, each serving distinct structural and functional roles:
Table 2: Core Components of CRISPR-Loaded Lipid Nanoparticles
| Component | Category | Function | Examples |
|---|---|---|---|
| Ionizable Cationic Lipids | Functional | pH-dependent charge; encapsulation, cellular uptake, endosomal release | ALC-0315, ALC-0307, DLin-MC3-DMA (MC3) [50] [51] |
| Phospholipids | Structural | Form particle matrix; enhance stability and bilayer structure | DSPC [50] |
| Cholesterol | Structural | Stabilizes bilayer structure; enhances integrity and fluidity | Cholesterol [50] |
| PEGylated Lipids | Stealth | Control particle size, prevent aggregation, reduce clearance | ALC-0159, DMG-PEG [50] [51] |
The mechanism of LNP-mediated CRISPR delivery involves a meticulously orchestrated sequence of intracellular events. The following diagram illustrates the pathway from systemic administration to functional gene editing within the target cell:
The ionizable cationic lipids undergo protonation in the acidic endosomal environment (pH ~5-6), enabling interaction with the endosomal membrane and facilitating destabilization and payload release into the cytoplasm [50]. This precise pH-responsive behavior is crucial for efficient CRISPR component delivery while minimizing toxicity.
Advantages Over Viral Delivery Systems
The transition from viral to non-viral delivery platforms represents a paradigm shift in therapeutic gene editing. While viral vectors, particularly adeno-associated viruses (AAVs), have been widely used, LNP platforms offer distinct advantages for clinical applications:
Table 3: LNP vs. Viral Vector Delivery Characteristics
| Characteristic | LNP Platform | Viral Vectors (AAV) | Therapeutic Implications |
|---|---|---|---|
| Immunogenicity | Low; enables redosing [51] | High; limits to single administration [51] | LNPs allow dose titration and multiple administrations |
| Payload Capacity | Large; accommodates multiple components [50] | Limited (~4.7kb) [51] | LNPs can deliver Cas9 mRNA + sgRNA simultaneously |
| Manufacturing | Rapid (days), scalable [51] | Complex, lengthy (weeks) [51] | LNPs support rapid therapeutic development |
| Integration Risk | Minimal (non-integrating) | Potential for insertional mutagenesis [50] | Enhanced safety profile for LNPs |
| Expression Kinetics | Transient (days) [51] | Long-term, persistent [50] | LNPs reduce off-target editing risk |
The reduced immunogenicity of LNPs represents a particularly significant advantage, as demonstrated by multiple clinical cases where patients safely received repeated doses of LNP-CRISPR therapies—a approach not feasible with viral vectors due to immune recognition [12] [51].
Current Clinical Applications and Protocol Implementation
Advanced LNP-CRISPR Workflows: From Formulation to Analysis
The implementation of LNP-based CRISPR delivery requires meticulous protocol execution across three critical phases: (1) LNP formulation and payload encapsulation, (2) in vivo delivery and editing, and (3) analytical assessment of editing outcomes.
Table 4: Key Research Reagents for LNP-CRISPR Experiments
| Reagent/Category | Specific Examples | Function in Experimental Workflow |
|---|---|---|
| Ionizable Lipids | ALC-0315, ALC-0307, DLin-MC3-DMA [51] | Core functional component enabling encapsulation and endosomal escape |
| Cas9 mRNA | Modified nucleotides (e.g., pseudouridine) [50] | Encodes Cas9 protein; modifications enhance stability and reduce immunogenicity |
| Guide RNA | Single-guide RNA (sgRNA), crRNA:tracrRNA complex [50] | Targets Cas9 to specific genomic loci through complementary base pairing |
| Reporter Systems | tdTomato, EGFP [52] | Enables visualization and quantification of editing efficiency |
| Animal Models | Ai9 reporter mice, disease models (e.g., hATTR) [12] [52] | Provides in vivo context for evaluating therapeutic efficacy and safety |
Detailed Protocol Specifications:
LNP Formulation: Utilize microfluidic mixing devices with precise flow rate controls (typically 1:3 aqueous:organic ratio) to combine lipid mixtures in ethanol with CRISPR payloads in aqueous buffer [50]. Ionizable lipids should constitute 30-50 mol% of total lipid composition.
Payload Encapsulation: For mRNA/sgRNA delivery, maintain 1:2 mass ratio of Cas9 mRNA to sgRNA during encapsulation. For RNP delivery, pre-complex GeoCas9 variants with sgRNA (1:1.2 molar ratio) for 10 minutes at 37°C prior to LNP encapsulation [52].
In Vivo Administration: Implement intravenous injections via tail vein in murine models at dosing regimens of 0.5-3 mg RNA/kg body weight. Utilize tissue-specific LNP formulations by modifying surface conjugations (e.g., DARPin proteins for T-cell targeting) [51].
Efficiency Quantification: Apply next-generation sequencing (NGS) of PCR-amplified target loci 7-14 days post-administration. Calculate editing percentages as (edited reads/total reads) × 100%. For functional assessment, measure reduction in target protein levels (e.g., TTR reduction by ELISA) [12].
Clinical Translation and Therapeutic Outcomes
The remarkable progression of LNP-CRISPR therapies from preclinical validation to clinical application is evidenced by multiple advanced clinical trials demonstrating both safety and efficacy:
Table 5: Clinical Trial Outcomes of LNP-Delivered CRISPR Therapies
| Therapeutic Target | Development Phase | Key Outcomes | Reference |
|---|---|---|---|
| hATTR Amyloidosis | Phase III (Intellia) | ~90% sustained TTR reduction; functional improvement [12] | NEJM (2024) |
| Hereditary Angioedema | Phase I/II (Intellia) | 86% kallikrein reduction; 73% attack-free [12] | NEJM (2024) |
| CPS1 Deficiency | Single-patient trial | Multi-dosing feasible; symptom improvement [12] | IGI Report (2025) |
| Sickle Cell Disease | Approved Therapy | First FDA-approved CRISPR therapy (ex vivo) | Casgevy (2024) |
Recent clinical breakthroughs include the landmark case of an infant with CPS1 deficiency who received a personalized in vivo CRISPR therapy developed and delivered within six months [12]. The administration of three escalating LNP-CRISPR doses without serious adverse events demonstrates the safety profile and redosing capability of the LNP platform. Similarly, Intellia Therapeutics reported the first redosing of in vivo CRISPR therapy in hATTR patients, with participants safely receiving second infusions at higher doses to enhance efficacy [12].
Emerging Innovations and Future Applications
Novel LNP Formulations for Tissue-Specific Delivery
While current LNP platforms demonstrate exceptional tropism for hepatocytes, enabling liver-focused therapeutic applications, recent advances are expanding delivery capabilities to previously inaccessible tissues:
Thermostable Cas9 Variants: Laboratory-evolved GeoCas9 mutants (iGeoCas9) demonstrate >100-fold higher editing efficiency compared to wild-type GeoCas9 and maintain functionality under LNP formulation conditions that typically denature proteins [52]. These thermostable variants enable efficient RNP delivery to lung tissue with 19% editing efficiency of the disease-causing SFTPC gene—a breakthrough for pulmonary genetic disorders [52].
Tissue-Slective LNP Formulations: Incorporation of acid-degradable cationic lipids and pH-sensitive PEGylated lipids enables preferential accumulation in pulmonary tissue, achieving 16% whole-lung editing efficiency in reporter mice [52]. Alternative targeting strategies include conjugation of designed ankyrin repeat proteins (DARPins) to LNP surfaces, which has demonstrated up to 98% binding and 90% expression in human CD8+ T cells [51].
Brain-Targeted Delivery: Emerging approaches for neurological disorders are showing promising preclinical results, bringing brain editing "closer to reality" [53]. These advances leverage novel LNP formulations capable of crossing the blood-brain barrier, potentially enabling treatment of devastating neurological conditions.
AI-Enhanced CRISPR Development
The integration of artificial intelligence with CRISPR therapeutics represents a transformative innovation accelerating therapeutic development. CRISPR-GPT, an AI tool developed at Stanford Medicine, functions as a gene-editing "copilot" that leverages 11 years of published experimental data to optimize CRISPR design, predict off-target effects, and troubleshoot experimental flaws [54]. This technology demonstrably reduces the learning curve for researchers and shortens therapeutic development timelines from years to months [54].
The convergence of CRISPR-based genome editing with LNP delivery platforms has catalyzed a revolutionary shift in therapeutic development, transforming fundamental bacterial immunity mechanisms into powerful human therapeutics. The unique properties of LNPs—including their reduced immunogenicity, capacity for redosing, transient expression profile, and manufacturing scalability—address critical limitations of viral delivery systems while enabling precise, systemic administration of gene-editing components.
As LNP formulations continue to evolve with enhanced tissue specificity and novel CRISPR payloads, the therapeutic landscape will expand beyond current liver-dominated applications to address genetic disorders in pulmonary, neurological, and other currently inaccessible tissues. The ongoing clinical success of LNP-CRISPR therapies, combined with emerging technologies like AI-accelerated design and thermostable editors, heralds a new era of genetic medicine where precise, in vivo genome editing becomes a mainstream therapeutic modality with potential to address previously untreatable genetic diseases.
The discovery and development of the Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) system represents a paradigm shift in molecular biology, transitioning from a fundamental discovery of bacterial adaptive immunity to a powerful tool for genome editing. This journey began in 1987 with the initial observation of unusual repetitive sequences in Escherichia coli [8] [3], though their biological function remained enigmatic for over a decade. Francisco Mojica first characterized these sequences as a distinct family in the 1990s and later hypothesized their role in microbial immunity [5]. The system's potential was fully realized in 2012 when Emmanuelle Charpentier and Jennifer Doudna demonstrated that the CRISPR-Cas9 system could be programmed for precise DNA cleavage, a breakthrough that earned them the 2020 Nobel Prize in Chemistry [8] [3].
This case study examines the landmark application of this technology: the first successful personalized CRISPR treatment for an infant with carbamoyl phosphate synthetase 1 (CPS1) deficiency, a rare, life-threatening metabolic disorder. This event, occurring in early 2025, represents the culmination of decades of research, demonstrating the feasibility of rapidly developing "on-demand" gene therapies for rare genetic diseases [55] [56]. The therapy was developed and administered in just six months, establishing a new precedent for the speed and potential of personalized genomic medicine [56].
Clinical Background: CPS1 Deficiency
Pathophysiology and Clinical Burden
Carbamoyl phosphate synthetase 1 deficiency (CPS1D) is a severe urea cycle disorder with an estimated incidence of 1 in 1,300,000 live births [57]. The CPS1 enzyme catalyzes the initial and rate-limiting step of the urea cycle in hepatocytes, where ammonia is converted into carbamoyl phosphate [58]. Mutations in the CPS1 gene lead to a complete or partial absence of this enzyme, resulting in an inability to detoxify ammonia, a byproduct of protein metabolism [55] [57].
This failure causes hyperammonemia, where toxic ammonia accumulates in the bloodstream. The condition presents in neonates with refusal to eat, lethargy, vomiting, and irritability, rapidly progressing to seizures, respiratory distress, abnormal movements, and cerebral edema due to ammonia's neurotoxic effects [57]. The mortality rate in early infancy is approximately 50%, and survivors often face permanent neurological damage [57] [56]. Standard management involves a strict low-protein diet and nitrogen-scavenging medications to reduce ammonia levels, serving as a bridge until a liver transplant can be performed—the only definitive treatment but limited by donor availability and surgical risks [55] [57].
The Patient: An Urgent Clinical Need
The subject of this case study, infant KJ, was diagnosed with CPS1 deficiency shortly after birth [55]. His prognosis was poor, and by five months of age, he was placed on the liver transplant list. His management required constant hospitalization to monitor for life-threatening hyperammonemic episodes, which could be triggered by common stressors like infection or dehydration [55] [56]. This dire clinical situation created the urgency for developing an innovative therapeutic approach.
Technical Development of the Personalized Therapy
Strategic Approach: In Vivo Base Editing
The research team at the Children's Hospital of Philadelphia (CHOP) and the Perelman School of Medicine at the University of Pennsylvania, in collaboration with the Innovative Genomics Institute (IGI), developed a personalized therapy with several key strategic components [55] [56].
- Targeted Editing Approach: Rather than using traditional CRISPR-Cas9 which creates double-stranded breaks, the team employed a base editing strategy. KJ's condition was caused by a single-point mutation—a one-letter error in his genetic code [56]. Base editors are modified CRISPR systems that can directly convert one DNA base into another without breaking the DNA backbone, offering a safer and more precise correction for this type of mutation [59] [56].
- Delivery System: The therapy was delivered via lipid nanoparticles (LNPs) [57] [56]. These LNPs are designed to travel to the liver and fuse with hepatocyte membranes, releasing their therapeutic payload—the RNA molecules encoding the base editor and the guide RNA—directly into the target cells [56]. This method enables in vivo editing, eliminating the need to remove cells from the body.
- Targeting Non-Reproductive Cells: The editing machinery was carefully designed to target somatic (non-reproductive) cells, ensuring the genetic changes would be confined to the patient and not heritable [55].
Table 1: Key Characteristics of the Personalized CRISPR Therapy
| Feature | Description | Rationale |
|---|---|---|
| Editing Platform | CRISPR Base Editing | Corrects single-nucleotide point mutation without double-stranded DNA breaks [56]. |
| Delivery Vehicle | Lipid Nanoparticles (LNPs) | Enables in vivo delivery to hepatocytes in the liver, the site of CPS1 expression [57] [56]. |
| Target Cell | Somatic Liver Cells (Hepatocytes) | Limits genetic changes to the patient; non-heritable [55]. |
| Dosing Strategy | Initial low dose, followed by higher dose(s) | Ensures initial safety and allows for titration based on patient response [55]. |
The Six-Month Development Timeline
The accelerated, six-month timeline from diagnosis to treatment was a monumental achievement, made possible by a highly coordinated multi-institutional effort and pre-established platform technologies [56].
- Rapid Genomic Analysis: The ongoing INGENUITI research study allowed for immediate whole-genome sequencing of KJ and his parents, enabling the team to quickly pinpoint the specific causal mutation [56].
- Guide RNA Design and Editor Screening: Kiran Musunuru's team at Penn designed the guide RNA (gRNA) to direct the base editor to the precise genomic location and screened for the most effective base editor variant for KJ's specific mutation [56].
- Safety Assessment (OFF-Target Analysis): Concurrently, the team at the IGI performed a critical safety assessment using an assay called CHANGE-seq-BE [56]. This next-generation sequencing-based method comprehensively maps potential off-target sites across the entire genome where the base editor might bind and edit unintentionally. Using KJ's own genomic DNA for this analysis increased its accuracy and predictive value [56].
- Efficacy and Toxicology Testing: The designed therapy was tested in laboratory models, including a bespoke mouse model developed by the Jackson Laboratory, to establish proof-of-concept and assess toxicity [56].
- Regulatory Review and Manufacturing: The team compiled the data into an expanded-access Investigational New Drug (IND) application for a single patient. The U.S. Food and Drug Administration (FDA) approved the application in just one week [57] [56]. Clinical-grade manufacturing of the LNP-encapsulated RNA therapy was streamlined through collaboration with Danaher Corporation and its operating companies [56].
The following workflow diagram illustrates the rapid, parallelized development process.
Experimental Protocols and Outcomes
Key Methodologies
The development and validation of the therapy relied on several sophisticated experimental protocols.
- CHANGE-seq-BE Off-Target Analysis: This assay involved incubating the patient's genomic DNA with the pre-formed base editor ribonucleoprotein (RNP) complex in vitro. The enzymatically cleaved DNA was then processed for next-generation sequencing. Bioinformatic analysis of the resulting data identified locations in the genome with sequence similarity to the intended target, which were then ranked by risk. Potential high-risk off-target sites were further validated in cell-based models [56].
- In Vivo Efficacy Model: A hypomorphic mouse model of CPS1 deficiency, which carries a specific point mutation (Asn674Ile) and exhibits reproducible hyperammonemia and reduced citrulline, was used to test the therapy's ability to restore ureagenesis [58]. Mice treated with the LNP-formulated base editor were challenged with a protein load, and blood ammonia and glutamate levels were measured to quantify functional improvement.
- Clinical Monitoring: After administration of the LNP therapy, KJ was monitored for acute adverse effects. The therapy's efficacy was assessed through biochemical markers, including blood ammonia levels, dietary protein tolerance, and the required dosage of nitrogen-scavenging medications [55] [56].
Treatment Outcomes and Efficacy
The infant received his first low dose of the therapy at six months of age, followed by at least one higher dose [55]. The response was positive and clinically significant.
- Safety: The treatment was well-tolerated with no serious adverse effects reported after multiple doses [55] [56].
- Biochemical and Clinical Improvement: Signs of efficacy emerged rapidly. The infant demonstrated an increased tolerance to dietary protein, and the care team could reduce his dependence on ammonia-scavenging medications [55] [57]. A critical test of the therapy's success occurred when the infant contracted a rhinovirus and later a gastrointestinal illness. These common infections, which are normally extreme risks for hyperammonemic crises in CPS1D patients, were successfully overcome without dangerous spikes in blood ammonia [55] [56]. This indicated that the edited liver cells were producing sufficient functional CPS1 enzyme to manage metabolic stress.
Table 2: Quantitative Clinical Outcomes Post-Treatment
| Parameter | Pre-Treatment Status | Post-Treatment Status |
|---|---|---|
| Ammonia Level Control | Unstable, high risk of hyperammonemia | Stable, even during metabolic stress from infection [55] |
| Dietary Protein Tolerance | Severely restricted | Markedly improved [55] [56] |
| Nitrogen-Scavenger Medication | High dependency | Reduced requirement [55] [56] |
| Clinical Setting | Continuous inpatient hospitalization | Discharged to home [57] [56] |
The Scientist's Toolkit: Key Research Reagents
The successful development of this therapy depended on a suite of critical research reagents and platform technologies.
Table 3: Essential Research Reagents and Solutions
| Reagent / Solution | Function in the Experiment |
|---|---|
| Base Editor (e.g., k-abe) | The core enzymatic tool that chemically converts one DNA base into another at the target site without creating a double-stranded break [57]. |
| Single-Guide RNA (sgRNA) | A synthetic RNA molecule that combines the functions of crRNA and tracrRNA to programmatically direct the base editor to the specific mutation in the CPS1 gene [56]. |
| Lipid Nanoparticles (LNPs) | A delivery vehicle that encapsulates the RNA-based therapy, protects it from degradation, and facilitates its entry into hepatocytes in vivo [57] [56]. |
| CHANGE-seq-BE Assay | A high-throughput, cell-free next-generation sequencing assay used to comprehensively profile the genome-wide off-target activity of the base editor, crucial for safety evaluation [56]. |
| CPS1 Hypomorphic Mouse Model | A preclinical animal model with residual CPS1 enzyme activity that mimics the human metabolic phenotype, allowing for the testing of therapeutic efficacy and safety [58]. |
Ethical and Regulatory Considerations
This pioneering case was conducted under an expanded-access IND, often called "compassionate use," which allows for the use of an investigational therapy outside of a clinical trial for patients with serious or immediately life-threatening conditions [57]. A foundational ethical principle adhered to was the restriction of editing to somatic cells, preventing any changes from being passed to future generations [55] [59].
The case also highlights the ethical imperative of timing in severe pediatric diseases. The standard drug development timeline, which can take a decade or more, is incompatible with the survival of infants with conditions like CPS1D. The six-month development window for this therapy sets a new ethical and operational benchmark for rapid intervention in ultra-rare, rapidly progressive diseases [56].
The successful treatment of infant KJ represents a historic milestone, serving as a powerful proof-of-concept for the entire field of personalized genetic medicine. It demonstrates that it is feasible to rapidly design, develop, safety-profile, and deploy a customized CRISPR-based therapy for a single patient within a clinically relevant timeframe [55] [56].
This achievement bridges the entire history of CRISPR, from its origins as a bacterial immune defense [8] [5] to its repurposing as a programmable laboratory tool [3], and now to its application as a truly personalized therapeutic. As noted by NIH's Dr. Joni L. Rutter, this platform promises "a new era of precision medicine for hundreds of rare diseases, bringing life-changing therapies to patients when timing matters most" [55]. The challenge now is to scale this "CRISPR for one" model into a robust, accessible framework for "CRISPR for all" who face untreatable genetic disorders [56].
1 Introduction: From Bacterial Immunity to Precision Medicine
The journey of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) from a mysterious bacterial sequence to a revolutionary genome-editing technology represents a paradigm shift in biomedical science. First identified in Escherichia coli in 1987, CRISPR-Cas systems were ultimately recognized as adaptive immune systems in prokaryotes, protecting against invading phages by integrating spacer sequences from foreign genetic elements [60]. The seminal discovery that the CRISPR-associated protein Cas9 could be programmed with guide RNAs to create precise double-stranded breaks in DNA paved the way for its development as a versatile genome-editing tool [5]. This technical guide examines the application of this powerful technology across hematology, oncology, and monogenic diseases, providing researchers with a detailed overview of current methodologies, clinical progress, and experimental protocols.
2 Technical Foundations of CRISPR-Cas9 Genome Editing
2.1 Core Mechanism and DNA Repair Pathways
CRISPR-Cas9 editing functions by introducing a site-specific double-stranded break (DSB) in the DNA. This break is then repaired by the cell's endogenous machinery primarily via two pathways:
- Non-Homologous End Joining (NHEJ): An error-prone repair process that often results in small insertions or deletions (INDELS) at the cut site. This is harnessed to disrupt gene function by knocking out a target gene [61].
- Homology-Directed Repair (HDR): A precise repair pathway that uses a donor DNA template to introduce specific genetic changes, such as nucleotide substitutions or gene insertions. This approach is used for gene correction but is limited by lower efficiency compared to NHEJ in many therapeutically relevant cells, including hematopoietic stem cells [61].
2.2 Delivery Methods for Therapeutic Editing
Efficient delivery of CRISPR components is critical for successful editing. The preferred method for ex vivo manipulation of sensitive primary cells, such as hematopoietic stem and progenitor cells (HSPCs) and T lymphocytes, is the ribonucleoprotein (RNP) complex. This complex consists of the preassembled Cas9 protein and a synthetic single-guide RNA (sgRNA). RNP delivery offers high editing efficiency, low toxicity, and transient activity, reducing off-target effects [61]. For in vivo applications, lipid nanoparticles (LNPs) have emerged as a leading vehicle for systemic delivery, showing particular tropism for the liver [12]. The use of chemically modified sgRNAs (e.g., with 2’-O-methyl-3’phosphorothiate) can further enhance stability and editing efficiency [61].
3 Applications in Hematology
3.1 Hemoglobinopathies
β-hemoglobinopathies, including sickle cell disease (SCD) and β-thalassemia, are monogenic disorders that have been the first to witness the successful clinical translation of CRISPR-based therapies.
Therapeutic Strategies:
- Reactivating Fetal Hemoglobin (HbF): A leading strategy involves using CRISPR-Cas9 to disrupt erythroid-specific enhancer regions of the BCL11A gene, a repressor of fetal hemoglobin. This reactivation of HbF compensates for the defective or absent adult β-globin, ameliorating the disease phenotype [61]. This is the mechanism behind the approved therapy Casgevy (exagamglogene autotemcel) [12].
- Direct Gene Correction: An alternative approach involves using HDR to correct the causative mutation in the HBB gene directly in HSPCs, though this faces challenges due to the typically low HDR efficiency in these cells [61].
Clinical Trial Results: As of early 2025, Casgevy has received regulatory approval in multiple regions for both SCD and transfusion-dependent beta thalassemia (TBT). Over 50 active clinical sites are now treating patients, with treatment coverage being secured through various healthcare systems [12].
3.2 Other Hematological Diseases
Beyond hemoglobinopathies, clinical trials are investigating CRISPR for a range of other blood disorders, including immunodeficiencies and hemophilia [62].
4 Applications in Oncology
4.1 Engineering Immune Cells for Cancer Therapy
A major focus in oncology has been the ex vivo engineering of a patient's own immune cells to enhance their anti-tumor potency.
- CAR-T Cell Engineering: CRISPR is used to generate more potent chimeric antigen receptor (CAR) T cells. This includes knocking out endogenous T-cell receptor genes to prevent graft-versus-host disease in allogeneic "off-the-shelf" products, and disrupting immune checkpoint genes like PD-1 to prevent T-cell exhaustion and improve persistence within the tumor microenvironment [63].
- Experimental Protocol for T-cell Editing:
- Isolation: T cells are isolated from patient or donor leukapheresis material.
- Activation: Cells are activated using anti-CD3/CD28 antibodies.
- Electroporation: Activated T cells are electroporated with RNP complexes targeting the desired genetic loci (e.g., TRAC, PDCD1).
- Viral Transduction: For CAR-T cells, a viral vector (e.g., lentivirus) encoding the CAR is used to transduce the cells.
- Expansion and Formulation: Edited cells are expanded ex vivo and then formulated for infusion back into the patient [61] [63].
4.2 Functional Genomics and Target Discovery
CRISPR screening enables the systematic identification of genes essential for tumor growth or therapy response.
- Perturb-map: A cutting-edge spatial functional genomics platform that combines pooled CRISPR screening with multiplexed imaging. It allows for the in situ analysis of how dozens of different gene knockouts affect tumor growth, histopathology, and immune composition within the intact tissue architecture of a mouse model. For instance, it was used to show that knockout of Tgfbr2 in cancer cells leads to T-cell exclusion and a fibro-mucinous tumor microenvironment [64].
- Workflow: A standard CRISPR knockout screen involves transducing a cell population with a pooled lentiviral sgRNA library, applying a selective pressure (e.g., a drug), and then using next-generation sequencing to quantify sgRNA abundance to identify genes conferring sensitivity or resistance [63].
5 Applications in Monogenic Diseases
5.1 In Vivo CRISPR Therapy for Hereditary Disorders
The development of LNP delivery has enabled direct in vivo genome editing, opening doors for treating genetic disorders affecting solid organs.
- Hereditary Transthyretin Amyloidosis (hATTR): Intellia Therapeutics' NTLA-2001 is a landmark in vivo CRISPR therapy. It uses LNPs to deliver CRISPR components targeting the TTR gene in hepatocytes. Clinical trials have reported deep (>90%) and sustained reductions in serum TTR protein levels, with functional stabilization or improvement of disease symptoms [12].
- Hereditary Angioedema (HAE): Similarly, an LNP-based therapy targeting the KLKB1 gene to reduce plasma kallikrein has shown promise. In a Phase I/II trial, the higher dose group experienced an 86% reduction in kallikrein and a significant decrease in HAE attacks [12].
- Quantitative Systems Pharmacology (QSP) Modeling: The complexity of in vivo CRISPR therapies (LNP, mRNA, sgRNA) has spurred the development of QSP models. These computational platforms characterize the pharmacokinetic/pharmacodynamic relationships, incorporating mechanisms from LNP biodistribution to intracellular gene editing, to predict dose-response and aid clinical translation [65] [66].
5.2 Bespoke CRISPR Therapies for Ultra-Rare Diseases
A landmark case in 2024 demonstrated the potential for personalized in vivo CRISPR therapy. An infant with a rare, life-threatening monogenic disease, CPS1 deficiency, received a bespoke therapy developed, FDA-approved, and administered within six months. The LNP-delivered therapy was safely administered in multiple doses, leading to clinical improvement and establishing a regulatory precedent for platform therapies [12].
6 The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential Reagents for CRISPR-based Research and Therapy Development
| Reagent / Material | Function and Key Features |
|---|---|
| Cas9 Protein | The core effector nuclease. Purified, recombinant protein for RNP formation ensures high editing efficiency and transient activity. |
| Synthetic sgRNA | A single-guide RNA that complexes with Cas9 and directs it to the target genomic locus. Chemically modified versions enhance stability. |
| Lipid Nanoparticles (LNPs) | A delivery vehicle for in vivo applications. Protects CRISPR payload (mRNA/sgRNA) and facilitates delivery to target cells, particularly hepatocytes. |
| Donor DNA Template | A single-stranded oligonucleotide (ssODN) or double-stranded DNA template (e.g., via AAV) for introducing precise edits via HDR. |
| Electroporation System | A critical instrument for the efficient delivery of RNP complexes into hard-to-transfect primary cells like HSPCs and T cells. |
7 Conclusion
CRISPR technology has rapidly evolved from a fundamental discovery of bacterial immunity into a powerful and versatile platform for treating human disease. Its application in hematology, exemplified by the approved therapy for SCD and TBT, has proven its curative potential. In oncology, it is revolutionizing cancer immunotherapy and functional genomics. Meanwhile, advances in LNP delivery are unlocking the potential for in vivo treatment of a wide array of monogenic disorders. Despite this remarkable progress, challenges remain, including optimizing HDR efficiency, ensuring long-term safety, and simplifying protocols for broader accessibility. As the field continues to mature, the therapeutic arsenal of CRISPR-based interventions is poised to expand significantly, paving the way for a new era of precision genetic medicine.
Appendix: Visualizations
Diagram 1: CRISPR-Cas9 Mechanism and DNA Repair Pathways
Diagram 2: Ex Vivo Cell Therapy Workflow (e.g., CAR-T, HSPC)
Diagram 3: In Vivo LNP Delivery Mechanism
Navigating the Challenges: Safety, Specificity, and Delivery Hurdles
The discovery of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) represents a pivotal chapter in the history of molecular biology. What began as the study of a mysterious bacterial immune system has evolved into a revolutionary genome editing technology that is transforming therapeutic development. The journey from fundamental microbial research to clinical applications began in 1993 when Francisco Mojica first characterized CRISPR loci, though the term itself wasn't coined until 2000 [5]. By 2005, Mojica recognized that these sequences matched snippets from bacteriophage genomes, leading him to correctly hypothesize that CRISPR constitutes an adaptive immune system in prokaryotes [5]. The subsequent decade witnessed rapid elucidation of the molecular mechanisms, including the identification of the Cas9 protein by Alexander Bolotin in 2005 [5], the demonstration of its DNA cleavage function by Sylvain Moineau in 2010 [5], and the critical discovery of tracrRNA by Emmanuelle Charpentier in 2011 [5]. The transformative breakthrough came in 2012 when multiple groups demonstrated that CRISPR-Cas9 could be reprogrammed for genome engineering [5], setting the stage for the current era of gene editing.
The core CRISPR-Cas9 system functions as a precise DNA-targeting platform comprising a Cas nuclease guided by a RNA molecule (sgRNA) to a specific genomic locus complementary to the guide sequence [11]. This RNA-guided complex recognizes target DNA adjacent to a protospacer adjacent motif (PAM) and induces double-strand breaks (DSBs) through its HNH and RuvC nuclease domains [11]. The cell then repairs these breaks through either the error-prone non-homologous end joining (NHEJ) pathway, often resulting in gene knockouts, or the more precise homology-directed repair (HDR) pathway for specific genetic alterations [11].
Despite its transformative potential, a significant challenge impeding the clinical translation of CRISPR technology is off-target editing – the non-specific activity of the Cas nuclease at sites other than the intended target, which can cause undesirable genomic alterations [29]. This comprehensive technical guide examines the assessment methodologies and mitigation strategies, with particular emphasis on high-fidelity Cas variants, that are essential for advancing CRISPR toward safe therapeutic applications.
Mechanisms and Implications of Off-Target Effects
Molecular Basis of Off-Target Activity
Off-target effects primarily occur due to the inherent flexibility of the Cas9-sgRNA complex in recognizing DNA sequences that bear partial complementarity to the guide RNA [29]. Wild-type Streptococcus pyogenes Cas9 (SpCas9) can tolerate between three and five base pair mismatches between the guide RNA and target DNA, particularly if these mismatches are distributed rather than clustered and located distal to the PAM sequence [29]. This promiscuity means that a single guide RNA can potentially create double-stranded breaks at multiple genomic loci with similarity to the intended target that possess an appropriate PAM [29].
The clinical significance of off-target effects depends largely on their genomic location. Edits in non-coding regions may have minimal functional consequences, whereas alterations in protein-coding genes, regulatory elements, or especially tumor suppressor genes and oncogenes could potentially lead to malignant transformations [29]. The risk profile also varies with application type: ex vivo editing allows for selection of properly edited cells, while in vivo editing poses greater concern as off-target effects cannot be subsequently selected against or reversed [29].
Clinical Relevance and Regulatory Considerations
The therapeutic implications of off-target effects have gained prominence with the first regulatory approvals of CRISPR-based medicines. During the review process of Casgevy – the first FDA-approved CRISPR therapy for sickle cell disease and transfusion-dependent beta thalassemia – regulators specifically focused on potential off-target risks, noting that individuals with rare genetic variants might be at higher risk [29]. The FDA now recommends that preclinical and clinical studies include thorough characterization of CRISPR off-target editing to minimize potential safety concerns [29].
The risk level varies significantly between application modalities. Cell therapies, where editing occurs ex vivo, permit selection of correctly edited cells prior to administration, thereby reducing risk [29]. In contrast, in vivo gene therapies introduce greater concern as off-target effects cannot be subsequently selected against or reversed once delivered to the patient [29]. A 2025 review emphasized that despite development of numerous assessment tools, the absence of standardized guidelines leads to inconsistent practices across studies, complicating clinical translation [67].
Assessment Methodologies: From Prediction to Detection
Comprehensive off-target assessment employs complementary computational prediction and experimental detection methods to identify potential off-target sites throughout the genome.
In Silico Prediction Tools
Computational prediction represents the first line of screening for potential off-target effects, with numerous algorithms developed to nominate sites likely to experience off-target activity based on guide RNA sequence similarity.
Table 1: Comparison of Major Off-Target Prediction Tools
| Tool Name | Primary Algorithm Basis | Key Features | Limitations |
|---|---|---|---|
| CasOT [68] | Exhaustive search with custom parameters | First exhaustive prediction tool; allows adjustment of PAM, mismatch number | Limited consideration of epigenetic factors |
| Cas-OFFinder [68] | sgRNA alignment with tolerance for bulges | High tolerance for sgRNA length, PAM types, mismatches/bulges | Does not incorporate chromatin accessibility |
| FlashFry [68] | High-throughput characterization | Rapid analysis of thousands of targets; provides on/off-target scores | Optimized for speed rather than comprehensive epigenomic context |
| CCTop [68] | Distance of mismatches to PAM | User-friendly web interface; consensus-constrained topology | Limited to pre-defined reference genomes |
| DeepCRISPR [68] | Deep learning with epigenetic features | Incorporates chromatin opening, DNA methylation; genome-wide profiles | Requires substantial computational resources |
| Elevation [68] | DNA accessibility information | Includes DNA accessibility in predictions | Only works with human exome (GRCh38) |
These computational tools primarily focus on sgRNA-dependent off-target effects and may insufficiently consider the complex intranuclear microenvironment, including epigenetic states and chromatin organization [68]. Consequently, in silico predictions require experimental validation, particularly for therapeutic applications.
Experimental Detection Methods
Experimental approaches for off-target detection range from targeted candidate site validation to comprehensive genome-wide screening, each with distinct advantages and limitations.
Table 2: Experimental Methods for Off-Target Detection
| Method | Principle | Sensitivity | Advantages | Limitations |
|---|---|---|---|---|
| Candidate Site Sequencing [29] | Sequencing of predicted off-target sites | Variable based on sequencing depth | Simple, cost-effective | Limited to pre-identified sites; may miss novel off-targets |
| GUIDE-seq [68] | Capture of double-stranded breaks via oligo integration | High (theoretically ~0.01%) | Genome-wide; captures in cellular context | Requires delivery of double-stranded oligos |
| Digenome-seq [68] | In vitro cleavage of purified genomic DNA + WGS | High (can identify indels with 0.1% frequency) | Sensitive; quantitative; no background from cellular processes | High sequencing cost; omits chromatin context |
| DIG-seq [68] | In vitro cleavage of cell-free chromatin + sequencing | High | Retains chromatin states; more accurate than Digenome-seq | Complex protocol; requires specialized expertise |
| CIRCLE-seq [68] | In vitro cleavage of circularized genomic DNA + sequencing | Very high (theoretically ~0.001%) | Extremely sensitive; low background | Purely in vitro; may not reflect cellular context |
| Whole Genome Sequencing [29] | Comprehensive sequencing of entire genome | Detection limited by coverage and cost | Most comprehensive; detects all variants including structural | Extremely expensive; requires high coverage for confidence |
The following workflow illustrates the typical progression from computational prediction to experimental validation in off-target assessment:
Diagram 1: Off-target assessment workflow illustrating the iterative process from prediction to validation.
Mitigation Strategies: High-Fidelity Cas Variants and Beyond
High-Fidelity Cas9 Variants
Protein engineering approaches have yielded numerous enhanced-fidelity Cas9 variants with reduced off-target activity while maintaining robust on-target editing. These variants typically incorporate mutations that destabilize Cas9's interaction with DNA until full complementarity with the guide RNA is confirmed.
Table 3: High-Fidelity Cas9 Variants and Their Characteristics
| Variant | Key Mutations | Off-Target Reduction | On-Target Efficiency | Notes |
|---|---|---|---|---|
| SpCas9-HF1 [29] | N497A, R661A, Q695A, Q926A | ~85% reduction | Similar to wild-type | Weakenes protein-DNA interactions |
| eSpCas9(1.1) [29] | K848A, K1003A, R1060A | Undetectable off-targets by BLESS | ~70% of wild-type | Enhances proofreading mechanism |
| HypaCas9 [29] | N692A, M694A, Q695A, H698A | >90% reduction | Similar to wild-type | Improved recognition of target complementarity |
| xCas9 [29] | E1219V, A1322R, R1335V, T1337R | Broad PAM recognition (NG, GAA, GAT) | Variable by site | Expanded PAM flexibility |
| Sniper-Cas9 [29] | F539S, M763I, K890N | Significant reduction | High maintenance | Balanced on/off-target profile |
While high-fidelity variants significantly reduce off-target cleavage, it is important to note that they may not necessarily reduce off-target DNA binding, which remains relevant for applications using catalytically dead Cas9 (dCas9) for epigenetic editing or transcriptional regulation [29].
Additional Mitigation Approaches
Beyond high-fidelity nucleases, multiple complementary strategies can further minimize off-target effects:
gRNA Optimization: Careful guide design represents the most straightforward approach to reduce off-target potential. This includes selecting guides with high specificity scores, optimizing GC content (40-60%), using truncated guides (17-19 nucleotides instead of 20), and incorporating specific chemical modifications (2'-O-methyl analogs and 3' phosphorothioate bonds) that enhance specificity [29].
CRISPR Cargo and Delivery Optimization: The format and delivery method of CRISPR components significantly impact off-target rates. Ribonucleoprotein (RNP) complexes of Cas9 protein and guide RNA enable rapid editing and degradation, reducing the window for off-target activity compared to plasmid DNA expression systems that persist longer in cells [29]. Lipid nanoparticles (LNPs) have emerged as particularly promising delivery vehicles as they enable transient expression and have demonstrated compatibility with redosing in clinical settings [12].
Alternative CRISPR Systems: Naturally occurring or engineered alternatives to SpCas9 offer different specificity profiles. Cas12a (Cpf1) recognizes different PAM sequences (TTN rather than NGG) and may exhibit different off-target propensity [68]. Additionally, base editing and prime editing systems represent particularly promising alternatives as they do not create double-strand breaks, instead using catalytically impaired Cas9 fused to other enzymes to directly convert one DNA base to another or perform more precise search-and-replace editing, respectively [11].
The following diagram illustrates the multi-layered approach to off-target mitigation:
Diagram 2: Multi-layered off-target mitigation strategies encompassing nuclease engineering, guide optimization, and delivery approaches.
The Scientist's Toolkit: Essential Reagents and Methods
Successful assessment and mitigation of off-target effects requires access to specialized reagents, tools, and methodologies. The following table catalogues essential components of the off-target researcher's toolkit.
Table 4: Essential Research Reagents and Tools for Off-Target Assessment
| Tool Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| gRNA Design Tools | CRISPOR, CHOPCHOP, Benchling | Identify optimal guide RNAs with high on-target and low off-target potential | Generate multiple candidate guides; cross-validate predictions across platforms |
| Off-Target Prediction Software | Cas-OFFinder, DeepCRISPR, CCTop | Computational nomination of potential off-target sites | Use multiple algorithms with different scoring methods for comprehensive assessment |
| High-Fidelity Nucleases | SpCas9-HF1, eSpCas9(1.1), HypaCas9 | Reduce off-target editing while maintaining on-target activity | Select based on balance between on-target efficiency and off-target reduction for specific application |
| Detection Kits & Assays | GUIDE-seq, Digenome-seq, CIRCLE-seq kits | Experimental identification of off-target editing events | Match method sensitivity and throughput to application stage (discovery vs. validation) |
| Analysis Software | ICE (Inference of CRISPR Edits) | Analysis of editing efficiency and identification of off-target edits | Compatible with Sanger sequencing data; provides publication-quality figures |
| Chemical Modification Reagents | 2'-O-methyl analogs, 3' phosphorothioate bonds | Enhance gRNA stability and specificity | Particularly important for in vivo applications where guide persistence is concern |
| Delivery Vehicles | Lipid nanoparticles (LNPs), Electroporation systems | Enable efficient cargo delivery with controlled duration | LNPs show particular promise for transient expression and potential redosing |
The journey from fundamental discoveries about bacterial immunity to transformative genome editing technology represents one of the most rapid translational trajectories in modern science. As CRISPR-based therapies transition from theoretical concepts to approved medicines – exemplified by Casgevy for sickle cell disease and beta thalassemia [12] – comprehensive assessment and mitigation of off-target effects has become an essential component of therapeutic development.
The field has progressed from recognizing off-target effects as a fundamental challenge to developing sophisticated solutions including high-fidelity Cas variants, advanced detection methodologies, and optimized delivery strategies. While significant progress has been made, ongoing challenges include establishing standardized assessment guidelines, improving the predictive power of computational tools, and further refining editing precision through next-generation systems like base and prime editing.
For researchers and therapeutic developers, a systematic approach incorporating computational prediction, experimental validation, and layered mitigation strategies provides the most robust pathway to ensuring the safety and efficacy of CRISPR-based interventions. As the technology continues to evolve, the comprehensive characterization and minimization of off-target effects will remain foundational to realizing the full potential of precision genetic medicine.
The journey of CRISPR from a curious bacterial sequence to a revolutionary gene-editing tool represents one of the most significant breakthroughs in modern biology. Originally identified as clustered regularly interspaced short palindromic repeats in the Escherichia coli genome in 1987, these structures initially puzzled scientists [8]. The pivotal understanding came in 2005 when Francisco Mojica recognized that these sequences matched snippets from bacteriophage genomes, leading to the hypothesis that CRISPR serves as an adaptive immune system in prokaryotes [5]. This system allows bacteria and archaea to capture and store genetic memories of past viral invasions, using this information to recognize and cleave subsequent attacks by the same pathogens [69] [8].
The transformation of this bacterial defense mechanism into a programmable genome-editing platform began with key discoveries of its molecular components. The Cas9 protein was identified as a core element of the system, capable of creating double-stranded breaks in DNA at sequences specified by guide RNAs [5]. The system's reprogrammability was demonstrated in 2012, when researchers showed that a single guide RNA could direct Cas9 to specific DNA targets [5]. This breakthrough earned Emmanuelle Charpentier and Jennifer Doudna the Nobel Prize in Chemistry in 2020 and launched the era of CRISPR-based genome editing [8].
However, as the technology has rapidly advanced toward clinical applications, including the first approved CRISPR therapy (Casgevy for sickle cell disease and beta-thalassemia), researchers have uncovered unexpected complexities [70] [12]. Beyond the well-documented concerns about off-target effects, a more pressing challenge has emerged: on-target structural variations and chromosomal rearrangements that pose significant safety concerns for therapeutic applications [70].
The Molecular Mechanism of CRISPR-Cas Systems
Natural Function and Engineering
In its natural context, the CRISPR-Cas system operates through three distinct stages: adaptation, where spacers from invading DNA are incorporated into the CRISPR array; expression, involving transcription and processing of CRISPR RNA (crRNA); and interference, where Cas proteins use crRNAs to identify and cleave matching foreign DNA sequences [69]. Type II systems, which utilize the single protein Cas9 for interference, have been most widely adapted for genome engineering due to their relative simplicity [69].
The engineering of CRISPR-Cas9 for genome editing simplified this natural system by combining the crRNA and trans-activating crRNA (tracrRNA) into a single guide RNA (sgRNA) that directs Cas9 to specific genomic locations [5]. Upon binding to a target sequence adjacent to a protospacer adjacent motif (PAM), Cas9 creates a double-strand break (DSB) in the DNA, which cellular repair mechanisms then attempt to fix [70].
DNA Repair Pathways and Editing Outcomes
The fate of a CRISPR-induced DNA break depends on which cellular repair pathway is engaged. Two primary pathways handle double-strand breaks in human cells:
- Non-Homologous End Joining (NHEJ): An error-prone pathway that directly ligates broken ends, often resulting in small insertions or deletions (indels) that can disrupt gene function [70].
- Homology-Directed Repair (HDR): A more precise pathway that uses a DNA template to repair the break accurately, enabling specific genetic corrections [70].
The balance between these pathways determines editing outcomes. While early CRISPR applications primarily focused on maximizing editing efficiency, recent research reveals that both pathways can produce unexpected structural variations that extend far beyond small indels at the target site [70].
The Spectrum of CRISPR-Induced Genomic Alterations
Beyond Indels: Complex Structural Variations
Early assessments of CRISPR editing outcomes primarily focused on small insertions and deletions at the target site. However, advanced genomic analyses have revealed a much broader spectrum of unintended consequences:
| Type of Variation | Scale | Potential Consequences | Detection Methods |
|---|---|---|---|
| Kilobase-scale deletions | 1,000-100,000 bp | Loss of regulatory elements, multiple exons | CAST-Seq, LAM-HTGTS |
| Megabase-scale deletions | >100,000 bp | Chromosomal arm loss, multiple gene loss | KROMASURE, cytogenetics |
| Chromosomal translocations | Inter-chromosomal | Oncogene activation, gene fusions | CAST-Seq, fluorescent in situ hybridization |
| Chromothripsis | Chromosome-wide | Complex genomic rearrangements | Whole-genome sequencing |
| Acentric/dicentric chromosomes | Entire chromosomes | Genomic instability, cell death | Karyotyping, cytogenetics |
These large-scale structural variations occur because double-strand breaks can engage in complex repair mechanisms that differ from standard NHEJ or HDR. When multiple breaks occur simultaneously—either at on-target sites, off-target sites, or spontaneously occurring background breaks—they can join in abnormal configurations, leading to chromosomal translocations and other rearrangements [70].
Compounding Factors and Risk Amplification
The risk of structural variations is not uniform across all editing conditions. Several factors significantly increase the frequency and severity of these events:
- DNA-PKcs Inhibition: The use of DNA-PKcs inhibitors to enhance HDR efficiency, such as AZD7648, has been shown to increase kilobase- and megabase-scale deletions by up to thousand-fold in some cases [70].
- p53 Suppression: Transient suppression of p53 to improve cell survival after editing can reduce the frequency of large chromosomal aberrations but raises oncogenic concerns due to p53's critical tumor suppressor role [70].
- Background Genomic Instability: Therapeutic cells often carry pre-existing DNA damage from culture conditions or reprogramming. When CRISPR editing is applied on top of this unstable background, the risks become additive, with editing-induced alterations intersecting with spontaneous breaks to create complex rearrangements [71].
Methodologies for Detecting Structural Variations
Advanced Genomic Analysis Techniques
Traditional short-read sequencing approaches often fail to detect large structural variations because they cannot span the affected regions and may miss rearrangements that delete primer-binding sites. Specialized methods have been developed to address these limitations:
CAST-Seq and LAM-HTGTS: These techniques combine chromatin purification or linear amplification with high-throughput sequencing to identify chromosomal translocations and other rearrangements involving the target site [70]. They provide genome-wide profiling of structural variations resulting from CRISPR editing.
KROMASURE Platform: This single-cell visualization system uses fluorescent in situ hybridization to directly observe chromosomal integrity and structural variants at the individual-cell level, detecting rare aberrations down to 0.1% prevalence [71]. The platform offers orthogonal analyzers tailored for specific genomic analyses:
- InSite: For on- and off-target variation assessment
- Screen: For chromosomal structural insights
- KBand: For copy number analysis
- PinPoint: For transgene integration mapping
Single-Cell Resolution: Unlike bulk methods that average signals across cell populations, single-cell approaches can identify mosaicism and rare but clinically significant variants that might be missed by ensemble analyses [71]. This is particularly important for detecting low-frequency structural variations that could expand during cell proliferation.
Experimental Workflow for Comprehensive Risk Assessment
The following diagram illustrates a recommended workflow for detecting structural variations in CRISPR-edited cells:
Research Reagent Solutions for Structural Variation Analysis
The table below outlines key research tools and their applications for detecting structural variations in CRISPR-edited cells:
| Research Tool | Primary Function | Key Features and Applications |
|---|---|---|
| CAST-Seq Assay | Chromosomal translocation detection | Identifies translocations between on-target sites and off-target regions across the genome [70] |
| LAM-HTGTS | Structural variation profiling | Maps complex rearrangements involving target loci using linear amplification [70] |
| KROMASURE Platform | Single-cell structural variant visualization | Detects chromosomal abnormalities, transgene integration, and copy number variations at single-cell resolution [71] |
| DNA-PKcs Inhibitors (AZD7648) | HDR enhancement research | Research tool to study how NHEJ inhibition affects structural variation frequency [70] |
| p53 Inhibitors (pifithrin-α) | Cell survival studies | Investigates how p53 pathway manipulation influences structural variation rates [70] |
Clinical Implications and Safety Assessment
Therapeutic Applications and Associated Risks
The progression of CRISPR-based therapies into clinical trials has accelerated our understanding of structural variation risks in therapeutic contexts. Notable examples include:
- Casgevy (exa-cel): This approved therapy for sickle cell disease and beta-thalassemia targets the BCL11A gene to induce fetal hemoglobin production. Studies have revealed that editing at the BCL11A locus in hematopoietic stem cells frequently produces large kilobase-scale deletions, warranting careful safety assessment [70].
- In vivo therapies: Recent advances in lipid nanoparticle (LNP) delivery have enabled direct in vivo editing, as demonstrated in treatments for hereditary transthyretin amyloidosis (hATTR) and CPS1 deficiency [12]. The ability to administer multiple doses with LNPs introduces new considerations for cumulative genomic risk assessment.
Regulatory Considerations and Risk Mitigation
Regulatory agencies including the FDA and EMA now require comprehensive assessment of both on-target and off-target effects, with particular attention to structural genomic integrity [70]. This regulatory landscape demands robust detection methods capable of identifying low-frequency but high-impact events.
Strategies to mitigate structural variation risks include:
- Repair pathway modulation: Co-inhibition of DNA-PKcs and DNA polymerase theta has shown protective effects against kilobase-scale (though not megabase-scale) deletions [70].
- Alternative editing platforms: Base editors and prime editors, which avoid double-strand breaks, can reduce but not eliminate structural variations [70].
- Careful donor selection: In ex vivo therapies, post-editing selection methods can enrich for successfully edited cells with minimal genomic damage [70].
The discovery of on-target structural variations and chromosomal rearrangements represents a critical maturation point in CRISPR technology development. As we refine our understanding of how DNA repair pathways shape editing outcomes, we can develop increasingly sophisticated approaches to maximize therapeutic benefits while minimizing risks.
The future of safe CRISPR application will likely involve:
- Advanced detection methods that combine multiple orthogonal approaches to capture the full spectrum of possible genomic alterations
- Novel editor designs that minimize double-strand break formation or guide repair toward precise outcomes
- Comprehensive safety assessment integrated throughout therapeutic development, from initial discovery to clinical application
As CRISPR technology continues its rapid evolution from bacterial immunity system to therapeutic tool, acknowledging and addressing these hidden risks will be essential for realizing its full potential to treat human disease. The ongoing refinement of safety assessment methodologies provides a pathway toward increasingly precise and secure genome editing applications.
The journey of CRISPR from a curious bacterial sequence to a revolutionary gene-editing technology represents a paradigm shift in biological science. Initially identified in 1987 as tandem repeats in the E. coli genome and later named Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) in 2002, this system was ultimately recognized as an adaptive immune mechanism in bacteria and archaea [72]. By 2012, researchers had harnessed this system for programmable genome editing, creating a two-component system consisting of a Cas nuclease and a guide RNA (gRNA) that could be targeted to specific DNA sequences [72] [73]. This breakthrough initiated a transformation across biological research and therapeutic development.
However, the transition from laboratory research to clinical application has encountered a significant barrier: the delivery problem. Efficient delivery of CRISPR components to target cells remains the critical limiting factor for both basic research and clinical translation [74]. The delivery vehicle must navigate multiple biological barriers to transport CRISPR cargo—whether as DNA, RNA, or protein—safely and efficiently to the nucleus of target cells while minimizing off-target effects and immune responses [75] [76]. This technical guide comprehensively compares the two primary delivery platforms—viral vectors and lipid nanoparticles (LNPs)—and examines the evolving strategies to overcome the challenge of tissue-specific tropism.
Cargo Formats for CRISPR Delivery
The CRISPR-Cas system can be delivered in three primary formats, each with distinct advantages and limitations that influence experimental design and therapeutic outcomes [74] [76]:
DNA: Typically plasmid DNA encoding both Cas9 and gRNA sequences. This format is cost-effective and straightforward to produce but requires nuclear entry and transcription/translation, resulting in slower onset and prolonged Cas9 expression that increases off-target risks [75] [76].
RNA: Cas9 mRNA combined with separate gRNA. This format bypasses the transcription step, leading to faster translation and reduced off-target effects due to transient expression. However, RNA is inherently unstable and requires careful handling and stabilization [75].
Ribonucleoprotein (RNP): Pre-complexed Cas9 protein and gRNA. RNP delivery enables immediate genome editing without transcriptional or translational delays, resulting in the shortest activity window and lowest off-target effects. However, protein production is more complex and costly, with stability challenges during storage and handling [75] [76].
Table 1: Comparison of CRISPR Cargo Formats
| Cargo Format | Production Complexity | Onset of Activity | Duration of Activity | Risk of Off-target Effects | Risk of Insertional Mutagenesis |
|---|---|---|---|---|---|
| DNA (Plasmid) | Low | Slow (days) | Prolonged | High | Yes |
| RNA | Medium | Medium (hours) | Transient | Medium | No |
| RNP (Protein) | High | Fast (hours) | Shortest | Low | No |
Viral Vector Delivery Systems
Viral vectors leverage the natural efficiency of viruses to transduce cells and deliver genetic material. They are among the most widely used delivery systems for in vivo CRISPR applications, with each vector type offering distinct characteristics [75] [74].
Adeno-Associated Viral Vectors (AAV)
AAV vectors have emerged as a leading platform for in vivo gene therapy due to their favorable safety profile, high tissue specificity, and ability to induce sustained transgene expression [77]. These non-pathogenic viruses with mild immune responses in humans are particularly valuable for preclinical models and clinical applications [74].
Key Advantages:
- Safety Profile: Non-pathogenic with low immunogenicity compared to other viral vectors [75] [77]
- Tropism Diversity: Multiple serotypes enable targeting of specific tissues (AAV9 for central nervous system, AAV5 for retina, AAV8 for liver) [75] [77]
- Long-term Expression: Persists primarily as episomes, enabling sustained transgene expression [77]
Critical Limitations:
- Packaging Capacity: Limited to ~4.7 kb, insufficient for full-length SpCas9 (4.2 kb) with additional regulatory elements [75] [77]
- Production Complexity: Scalable manufacturing remains challenging [75]
Innovative Strategies to Overcome AAV Limitations:
- Compact Cas Orthologs: Utilizing smaller Cas proteins like Staphylococcus aureus Cas9 (SaCas9, ~3.2 kb) or Campylobacter jejuni Cas9 (CjCas9) that fit within AAV packaging constraints [75] [77]
- Dual AAV Systems: Splitting CRISPR components across two separate vectors that recombine in target cells [75] [77]
- Trans-splicing Vectors: Employing split-intron systems that reconstitute full-length Cas9 post-delivery [77]
Lentiviral Vectors (LV)
Lentiviral vectors are retroviral vectors derived from HIV backbone that integrate into the host genome, enabling long-term stable expression [75] [74].
Key Advantages:
- High Efficiency: Excellent transduction efficiency across diverse cell types [75]
- Large Capacity: Can accommodate large genetic payloads including Cas9 and multiple gRNAs [74]
- Dividing/Non-dividing Cells: Effectively transduces both dividing and non-dividing cells [74]
Critical Limitations:
- Insertional Mutagenesis: Random integration raises safety concerns for clinical applications [75] [74]
- Persistent Expression: Continuous Cas9 expression increases off-target risks [75]
- Immunogenicity: HIV backbone may trigger immune responses [74]
Safety Engineering Approaches:
- Integrase-Deficient Lentivirus (IDLV): Reduces integration rates by approximately 500-fold while maintaining transduction efficiency in post-mitotic cells [75]
- Inducible Systems: Tetracycline-responsive promoters enable temporal control of Cas9 expression [75]
Adenoviral Vectors (AdV)
Adenoviral vectors are larger DNA viruses with substantial packaging capacity, making them suitable for delivering oversized CRISPR constructs [74].
Key Advantages:
- Large Packaging Capacity: Can accommodate up to 36 kb of genetic material [74]
- High Titer Production: Amenable to industrial-scale manufacturing [74]
- Broad Tropism: Infects both dividing and non-dividing cells [74]
Critical Limitations:
- Immunogenicity: Strong immune activation limits redosing potential [75] [74]
- Cytotoxicity: Can induce inflammatory responses and host cell damage [74]
Table 2: Comparative Analysis of Viral Vector Systems for CRISPR Delivery
| Parameter | AAV | Lentivirus | Adenovirus |
|---|---|---|---|
| Packaging Capacity | ~4.7 kb | ~8 kb | ~36 kb |
| Integration | Mostly episomal | Random integration | Mostly episomal |
| Immunogenicity | Low | Moderate | High |
| Expression Duration | Long-term (years) | Long-term (stable) | Transient (weeks) |
| Production Titer | Moderate | High | Very high |
| Clinical Safety | High | Moderate (insertional mutagenesis) | Moderate (high immunogenicity) |
| Recommended Applications | In vivo therapy | Ex vivo editing, screening | In vivo vaccination, oncology |
Non-Viral Delivery: Lipid Nanoparticles (LNPs)
Lipid nanoparticles represent the leading non-viral delivery platform for CRISPR components, particularly gaining prominence through their successful application in mRNA COVID-19 vaccines [74]. LNPs are synthetic nanoparticles composed of ionizable lipids, phospholipids, cholesterol, and PEG-lipids that self-assemble into vesicles capable of encapsulating nucleic acids or proteins [75] [74].
LNP Formulation and Mechanism
LNPs protect their cargo from degradation and facilitate cellular entry through endocytosis. The critical step in LNP-mediated delivery is endosomal escape, where the nanoparticles must rupture the endosomal membrane before degradation in lysosomes [74]. The ionizable lipids undergo charge changes in the acidic endosomal environment, promoting membrane disruption and cargo release into the cytoplasm [74].
Advantages of LNP Delivery
- Transient Expression: Limited duration of activity reduces off-target effects [75]
- Redosing Capability: Lower immunogenicity enables multiple administrations, as demonstrated in clinical trials where participants received additional doses to increase editing efficiency [12]
- Flexible Cargo: Compatible with DNA, mRNA, and RNP formats [75] [74]
- Clinical Validation: FDA-approved for mRNA vaccines and CRISPR therapies in clinical trials [75] [12]
Limitations and Optimization Strategies
- Hepatic Tropism: Conventional LNPs predominantly accumulate in the liver, limiting applications for other tissues [12]
- Endosomal Escape: Inefficient escape from endosomes remains a bottleneck for delivery efficiency [74]
- Variable Efficiency: Delivery efficiency varies significantly across cell types [75]
Innovative Engineering Solutions:
- Selective Organ Targeting (SORT): Incorporation of supplementary lipids enables targeting of lung, spleen, and other tissues beyond the liver [74]
- Composition Optimization: Adjusting lipid ratios and structures to enhance stability, encapsulation efficiency, and endosomal escape [74]
Tropism Engineering Strategies
Tropism—the specific targeting of delivery vehicles to particular tissues or cell types—represents perhaps the most significant challenge in CRISPR therapeutics. Both viral and non-viral platforms have undergone extensive engineering to improve their targeting capabilities.
Viral Vector Tropism Modification
Natural Serotype Selection: Different AAV serotypes naturally target specific tissues—AAV9 crosses the blood-brain barrier, AAV1 targets muscle, AAV6 infects airways, and AAV8 has high liver tropism [75] [77].
Capsid Engineering:
- Directed Evolution: Sequential selection of capsid mutants with enhanced targeting properties [75] [77]
- Rational Design: Structure-guided modification of capsid surfaces to alter receptor binding [77]
- Peptide Display: Incorporation of targeting peptides into capsid proteins to redirect tropism [77]
LNP Tropism Enhancement
SORT Technology: The Selective Organ Targeting platform incorporates additional SORT molecules that determine tissue destination post-systemic administration, enabling targeted delivery to lung, spleen, and specific liver cell types [74].
Ligand Conjugation: Surface functionalization with antibodies, peptides, or small molecules that bind receptors on target cells [74].
Composition-driven Targeting: Modulating LNP size, surface charge, and lipid composition to influence biodistribution and cellular uptake patterns [74].
Experimental Protocols and Workflows
In Vivo CRISPR Delivery Workflow
The following diagram illustrates the complete workflow for in vivo CRISPR delivery using viral vectors or LNPs, from component preparation to validation:
Diagram 1: Comprehensive workflow for in vivo CRISPR delivery showing key decision points from cargo selection through administration and validation.
Protocol: LNP Formulation for mRNA Delivery
Materials Required:
- Ionizable lipid (e.g., DLin-MC3-DMA)
- Phospholipid (e.g., DSPC)
- Cholesterol
- PEG-lipid (e.g., DMG-PEG 2000)
- CRISPR mRNA or RNP
- Ethanol and citrate buffer (pH 4.0)
- Microfluidic mixer or T-tube apparatus
Procedure:
- Lipid Solution Preparation: Dissolve ionizable lipid, phospholipid, cholesterol, and PEG-lipid in ethanol at specific molar ratios (typically 50:10:38.5:1.5)
- Aqueous Phase Preparation: Dilute CRISPR cargo in 10 mM citrate buffer (pH 4.0)
- Nanoparticle Formation: Rapidly mix lipid and aqueous solutions using microfluidic device at 1:3 volumetric flow rate ratio
- Buffer Exchange: Dialyze or use tangential flow filtration to replace ethanol-citrate buffer with PBS
- Characterization: Measure particle size (70-100 nm ideal), polydispersity index (<0.2 ideal), and encapsulation efficiency (>90% target)
- Sterile Filtration: Pass through 0.22 μm filter for in vivo applications
Quality Control:
- Dynamic light scattering for size distribution
- RiboGreen assay for encapsulation efficiency
- Gel electrophoresis for cargo integrity
- Endotoxin testing (<5 EU/mL)
Protocol: AAV Production for CRISPR Delivery
Materials Required:
- Transfer plasmid with ITRs flanking CRISPR expression cassette
- Packaging plasmid (rep/cap genes)
- Adenoviral helper plasmid
- HEK293T cells
- Polyethylenimine (PEI) transfection reagent
- Opti-MEM reduced serum media
- Iodixanol gradient solutions
Procedure:
- Cell Seeding: Plate HEK293T cells at 70% confluency in cell factories or multilayer flasks
- Triple Transfection: Mix transfer, packaging, and helper plasmids at 1:1:1 ratio with PEI in Opti-MEM
- Media Change: Replace media 6-8 hours post-transfection
- Harvest: Collect cells and media 72 hours post-transfection
- Purification: Lys cells by freeze-thaw, treat with benzonase, and purify by iodixanol density gradient centrifugation
- Concentration and Buffer Exchange: Concentrate using Amicon centrifugal filters and exchange to final formulation buffer
- Quality Control: Determine viral titer (qPCR), purity (SDS-PAGE), and sterility
Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR Delivery Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Viral Packaging Systems | AAVpro Helper Free System (Takara), Lenti-X Packaging Single Shots (Clontech) | Production of high-titer viral vectors for in vivo delivery | Select serotype based on target tissue; optimize MOI for specific cell types |
| LNP Formulation Kits | PreciGen LNP Kit (Sigma), GenVoy-ILM (Precision NanoSystems) | Simplified LNP assembly for mRNA and RNP delivery | Compatible with standard microfluidic instruments; scalable from 1 mL to 100 mL |
| Tropism Modification Tools | AAV Phage Display Libraries (Vector Biolabs), SORT Lipid Kits (Sigma) | Engineering tissue-specific targeting | In vivo biopanning required for novel targeting peptides |
| Cargo Production Kits | HiScribe T7 mRNA Kit (NEB), Cas9 Protein Purification Kit (Thermo) | Generation of CRISPR components in DNA, RNA, or protein formats | Include modified nucleotides for mRNA stability; His-tag for protein purification |
| Analytical Tools | ZetaSizer (Malvern), qPCR AAV Titration Kit (Vector Biolabs) | Characterization of delivery vehicles and editing efficiency | Dynamic light scattering for size; ddPCR for precise titer determination |
Clinical Applications and Case Studies
The clinical translation of CRISPR therapies has highlighted the critical importance of delivery selection in determining therapeutic outcomes.
Successful Ex Vivo Therapy: Casgevy for Sickle Cell Disease
Casgevy, the first FDA-approved CRISPR-based therapy, utilizes RNP delivery via electroporation for ex vivo editing of hematopoietic stem cells [75] [12]. This approach avoids delivery challenges associated with in vivo administration and demonstrates the clinical viability of RNP formats for precise genome editing [75].
In Vivo LNP Delivery: Intellia Therapeutics for hATTR
Intellia's phase I trial for hereditary transthyretin amyloidosis (hATTR) represents the first successful systemic in vivo CRISPR therapy [12]. The therapy employs LNP-formulated CRISPR mRNA targeting the TTR gene in hepatocytes, leveraging the natural hepatic tropism of LNPs [12]. Clinical results showed rapid, deep (>90%), and sustained reduction of TTR protein levels with manageable side effects, establishing LNP delivery as a viable platform for in vivo genome editing [12].
In Vivo Viral Delivery: EDIT-101 for LCA10
EDIT-101 utilizes AAV5 vectors for subretinal delivery of CRISPR components to treat Leber Congenital Amaurosis type 10 [77]. This approach leverages the natural tropism of AAV5 for retinal cells and the immune-privileged status of the eye. Early phase trials demonstrated favorable safety and improved photoreceptor function, supporting the feasibility of AAV-mediated in vivo editing [77].
The evolution of CRISPR from a bacterial immune mechanism to a transformative therapeutic technology has consistently encountered the delivery problem as its primary limitation. Both viral vectors and LNPs offer distinct advantages—viral vectors provide unparalleled efficiency and tissue targeting through natural infection mechanisms, while LNPs offer transient expression, redosing capability, and flexible cargo accommodation.
The future of CRISPR delivery will likely involve hybrid approaches that combine the strengths of multiple platforms. Viral vectors may be employed for long-term expression of compact base editors, while LNPs could deliver larger nucleases for transient therapeutic effects. Tropism engineering will continue to advance through directed evolution and rational design, enabling precise targeting of specific cell types while avoiding off-target tissues.
As the field progresses, the integration of computational design with high-throughput screening will accelerate the development of next-generation delivery systems. Machine learning algorithms can predict optimal LNP compositions for specific tissues, while phage display libraries identify novel targeting peptides for viral vectors. These advances, combined with improved manufacturing processes, will ultimately solve the delivery problem and unlock the full potential of CRISPR-based therapeutics for a broad spectrum of genetic diseases.
The history of CRISPR—from fundamental bacterial biology to clinical application—serves as a powerful reminder that solving delivery challenges requires deep understanding of both biological mechanisms and engineering principles. As these fields continue to converge, the next chapter of CRISPR delivery will likely yield even more sophisticated solutions to this central problem in genetic medicine.
The transition of CRISPR-Cas9 from a bacterial immune system to a revolutionary gene-editing technology represents one of the most significant scientific advancements of the 21st century. Awarded the Nobel Prize in Chemistry in 2020, this "genetic scissors" technology enables precise manipulation of genomes across diverse organisms [8]. However, as research advances toward therapeutic applications, the immunogenicity of CRISPR components has emerged as a critical challenge. The very origin of CRISPR-Cas9 in bacteria contributes to its recognition by the human immune system, potentially triggering both innate and adaptive immune responses that can compromise safety and efficacy [78]. This in-depth technical guide examines the immunogenic concerns associated with Cas proteins and delivery vehicles, framing these challenges within the historical context of CRISPR development and providing researchers with current methodologies to assess and mitigate immune responses.
Historical Context: From Bacterial Immunity to Gene Editing
The journey of CRISPR-Cas9 from bacterial defense mechanism to gene-editing powerhouse informs our understanding of its immunogenic potential. The discovery timeline reveals how this natural system was repurposed for genetic engineering:
1987-2005: Initial Discoveries - CRISPR sequences were first identified in Escherichia coli in 1987 and later recognized as part of an adaptive immune system in prokaryotes by Francisco Mojica [8] [5]. The crucial observation that CRISPR spacers matched viral DNA sequences led to the hypothesis that CRISPR provides acquired resistance against viruses in prokaryotes [5].
2005-2011: Mechanism Elucidation - Alexander Bolotin's discovery of Cas9 and the protospacer adjacent motif (PAM) provided key insights into the system's functionality [5]. Subsequent research confirmed that CRISPR systems could function heterologously in other species, suggesting their potential as programmable gene-editing tools [5]. Emmanuelle Charpentier's discovery of tracrRNA completed the understanding of the natural CRISPR-Cas9 system's components [8] [5].
2012-Present: Tool Development - The engineering of the dual-RNA structure into a single-guide RNA (sgRNA) simplified the system [5], while the successful adaptation of CRISPR-Cas9 for genome editing in eukaryotic cells by Feng Zhang and George Church's teams opened new possibilities for therapeutic applications [5].
The historical development of CRISPR-Cas9 reveals a fundamental irony: the bacterial origins of the system that make it so effective for gene editing also contribute to its immunogenicity in human applications. As CRISPR technology progresses toward clinical use, understanding and addressing these immune responses becomes paramount.
Immune Responses to Cas Proteins
Mechanisms of Cas Protein Immunogenicity
Cas nucleases, particularly the commonly used Streptococcus pyogenes Cas9 (SpCas9), can trigger both innate and adaptive immune responses through multiple mechanisms:
Pre-existing Immunity: Bacterial infections common in human populations may have pre-sensitized immune systems to Cas proteins. Studies have detected anti-Cas9 antibodies and T-cell responses in healthy individuals [78]. This pre-existing immunity can lead to rapid clearance of CRISPR-treated cells and potentially serious adverse effects.
Intracellular Immune Recognition: Endogenous Cas9 expression can activate pro-inflammatory pathways through intracellular pattern recognition receptors. This includes potential activation of the cGAS-STING pathway in response to cytoplasmic DNA, leading to type I interferon production [78].
Major Histocompatibility Complex (MHC) Presentation: Cas9 peptides can be processed and presented via MHC class I and II pathways, activating CD8+ and CD4+ T cells respectively. This T-cell activation can lead to targeted elimination of CRISPR-engineered cells [78].
Assessing Cas9 Immunogenicity: Experimental Approaches
Researchers employ multiple methodologies to evaluate immune responses to Cas proteins:
Table 1: Experimental Approaches for Assessing Cas9 Immunogenicity
| Methodology | Key Measurements | Technical Considerations |
|---|---|---|
| ELISpot | IFN-γ producing cells, T-cell frequency | High sensitivity; requires fresh PBMCs |
| Intracellular Cytokine Staining | Multiplex cytokine detection, T-cell subset identification | Flow cytometry-based; enables immunophenotyping |
| Luminex Assay | Cytokine/chemokine profiling | Multiplex capability; comprehensive immune profiling |
| Antibody Detection ELISA | Anti-Cas9 IgG/IgM titers | Standardized protocols; establishes baseline immunity |
| T-cell Proliferation Assays | CFSE dilution, antigen-specific expansion | Measures functional T-cell responses |
Detailed Protocol: In Vitro T-cell Activation Assay
PBMC Isolation: Collect peripheral blood mononuclear cells (PBMCs) from healthy donor buffy coats using density gradient centrifugation (Ficoll-Paque PLUS).
Antigen Presentation Cell (APC) Preparation: Differentiate monocytes from PBMCs using GM-CSF (50 ng/mL) and IL-4 (20 ng/mL) over 5 days to generate dendritic cells. Pulse with Cas9 protein (10 μg/mL) for 24 hours.
T-cell Co-culture: Isolate CD4+ and CD8+ T cells using magnetic bead separation. Co-culture T cells with Cas9-pulsed APCs at 10:1 ratio in RPMI-1640 complete medium.
Activation Assessment: After 72 hours, measure T-cell proliferation via CFSE dilution using flow cytometry. Analyze supernatant for IFN-γ, IL-2, and IL-6 using Luminex multiplex assay.
Data Analysis: Calculate stimulation index (SI) relative to unpulsed APCs. SI >2 considered positive response.
Immune Responses to Delivery Vehicles
Viral Vector Immunogenicity
Viral vectors, particularly adeno-associated viruses (AAVs), represent the most common delivery method for in vivo CRISPR applications but present significant immunogenic challenges:
Table 2: Immune Challenges Associated with CRISPR Delivery Vehicles
| Delivery Vehicle | Immune Challenges | Mitigation Strategies |
|---|---|---|
| Adeno-Associated Virus (AAV) | Pre-existing neutralizing antibodies; Capsid-specific T-cell responses; Transgene-induced immunity | Capsid engineering; Serotype switching; Empty capsid removal; Immunosuppression |
| Lipid Nanoparticles (LNPs) | Complement activation; Anti-PEG antibodies; Inflammatory responses to ionizable lipids | PEG alternatives; Structure-activity relationship optimization; Selective organ targeting (SORT) molecules |
| Adenoviral Vectors | Strong innate immunity; High prevalence of pre-existing immunity; Inflammatory cytokine release | Hexon hypervariable region modification; Suppression of vector-induced innate responses |
| Lentiviral Vectors | Insertional mutagenesis concerns; Immune responses to viral enzymes | Self-inactivating (SIN) designs; Non-integrating versions; Pseudotyping |
AAV Immune Recognition Mechanisms:
Neutralizing Antibodies: Pre-existing AAV antibodies from natural infections can neutralize vectors before reaching target tissues, significantly reducing transduction efficiency [77] [74].
Capsid-Specific T Cells: AAV capsid peptides presented on MHC class I can activate CD8+ T cells, leading to elimination of transduced cells [77].
Toll-like Receptor (TLR) Activation: AAV genomes can activate endosomal TLRs (particularly TLR9), initiating innate immune responses that enhance adaptive immunity against the vector [77].
Assessing Vector Immunogenicity: Experimental Workflow
Immune Assessment Workflow for Delivery Vehicles
Mitigation Strategies for Cas9 and Delivery Vehicle Immunogenicity
Cas9 Protein Engineering
Multiple engineering approaches have been developed to reduce Cas9 immunogenicity:
Epitope Depletion: Computational mapping and experimental validation of immunodominant T-cell epitopes followed by targeted mutation to eliminate epitopes while maintaining nuclease activity [78]. This approach has yielded Cas9 variants with reduced T-cell activation while retaining >90% editing efficiency.
Humanization: Engineering Cas9 sequences to resemble human protein motifs reduces foreign character while maintaining function. This includes codon optimization and replacement of bacterial sequences with human homologs where structurally feasible [78].
Compact Cas Orthologs: Smaller Cas proteins from other bacterial species (SaCas9, CjCas9, Cas12f) offer dual advantages of reduced size for delivery and potentially lower cross-reactivity with pre-existing immunity [77]. These compact variants also enable packaging into AAV vectors with larger regulatory elements.
Delivery Vector Engineering
Innovative vector engineering strategies aim to evade immune recognition:
Capsid Engineering: Directed evolution and rational design of AAV capsids to create "stealth" vectors with reduced antibody recognition while maintaining tropism [77]. This includes engineering of novel AAV variants with altered antigenic surfaces.
Lipid Nanoparticle Optimization: Development of ionizable lipids with reduced immunostimulatory profiles while maintaining delivery efficiency. SORT (Selective Organ Targeting) technology enables tissue-specific delivery, potentially reducing systemic immune exposure [74].
Polymer Shields: Covalent attachment of PEG or other hydrophilic polymers creates steric hindrance that reduces protein adsorption and immune recognition. However, anti-PEG immunity necessitates alternative polymer strategies [74].
Table 3: Comparative Analysis of Immunogenicity Mitigation Approaches
| Strategy | Mechanism | Advantages | Limitations |
|---|---|---|---|
| Cas9 Epitope Depletion | Removal of T-cell epitopes | Maintains catalytic activity; Potentially universal application | Risk of developing new immunogenic sites; Possible reduction in activity |
| AAV Capsid Engineering | Altered antigenic surfaces | Evades pre-existing immunity; Enables redosing | Technical complexity; Potential impact on tropism |
| Immunosuppression | Transient immune suppression | Clinically established protocols; Immediate application | Increased infection risk; Non-specific immunosuppression |
| LNP Formulation Optimization | Reduced inflammatory lipid components | Tissue-specific targeting; Modular design | Complex manufacturing; Potential batch variability |
| Virus-Like Particles (VLPs) | Non-integrating, transient delivery | Reduced persistence concerns; Lower immunogenicity | Packaging capacity limitations; Manufacturing challenges |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Immunogenicity Assessment
| Reagent/Category | Function | Example Applications |
|---|---|---|
| Cas9 Enzyme Variants | Genome editing effector | Compare immunogenicity across orthologs; Epitope mapping studies |
| AAV Serotype Panel | Delivery vector comparison | Evaluate pre-existing immunity; Tropism studies |
| LNP Formulations | Non-viral delivery | Assess inflammatory potential; Tissue targeting efficiency |
| Human PBMCs | Ex vivo immunogenicity screening | Pre-clinical safety assessment; Donor variability studies |
| Cytokine Detection Kits | Immune response quantification | Multiplex cytokine profiling; Response kinetics |
| MHC Tetramers | Antigen-specific T-cell detection | Epitope mapping; T-cell frequency determination |
| Neutralization Assay Kits | Vector antibody assessment | Pre-existing immunity screening; Vaccine response evaluation |
| TLR Reporter Cell Lines | Innate immune activation | Pattern recognition receptor engagement; Adjuvant screening |
The immunogenic concerns surrounding Cas proteins and delivery vehicles represent significant but not insurmountable barriers to clinical translation of CRISPR-based therapies. The historical development of CRISPR from bacterial immunity to gene-editing technology informs our current understanding of these challenges. As the field progresses, integrated approaches combining protein engineering, vector development, and strategic immunosuppression will be essential for realizing the full therapeutic potential of CRISPR technologies. Future research directions include developing more comprehensive immunogenicity screening platforms, advancing humanized mouse models for immune response prediction, and establishing standardized assays for cross-study comparisons. By addressing these immunogenic concerns through multidisciplinary collaboration, the field can advance safe and effective CRISPR-based treatments for genetic disorders.
The discovery of the CRISPR-Cas9 system, awarded the Nobel Prize in Chemistry in 2020, has revolutionized genetic research and therapeutic development [8]. This journey began not in human cells, but in fundamental microbiology: Francisco Mojica first characterized CRISPR loci in 1993, and by 2005, he and other researchers had recognized their function as an adaptive immune system in prokaryotes [5]. The pivotal understanding that this system could be repurposed for precise genome editing created a new paradigm in molecular biology [8] [5].
At the heart of all CRISPR-mediated editing lies a critical biological process: the cellular response to double-strand breaks (DSBs). When the Cas nuclease introduces a DSB, it essentially creates a genetic decision point. The cell can repair this break primarily through two competing pathways: the error-prone non-homologous end joining (NHEJ) or the precise homology-directed repair (HDR) [79] [38]. The balance between these pathways ultimately determines the editing outcome. While HDR enables precise gene correction or insertion using a donor template, its efficiency is notoriously low, especially in post-mitotic cells, as NHEJ dominates the repair process in most mammalian cells [79]. This technical challenge has spurred the development of strategies to manipulate this balance, but as recent evidence reveals, such interventions carry underappreciated risks, including significant genomic alterations that threaten the safety and efficacy of clinical applications [80] [81].
DNA Repair Pathways in CRISPR Genome Editing
The Core Competing Pathways: NHEJ and HDR
The cellular machinery offers two main avenues for repairing the DSBs introduced by CRISPR-Cas9, each with distinct mechanisms and outcomes:
Non-Homologous End Joining (NHEJ): This is an error-prone repair pathway that rejoins broken DNA ends without requiring a homologous template [38]. It is active throughout the cell cycle and often results in small insertions or deletions (indels) at the cleavage site [81] [38]. These indels can disrupt gene function, making NHEJ the preferred pathway for gene knockout studies [38]. Its efficiency and template-independent nature make it the dominant repair mechanism in most somatic cells.
Homology-Directed Repair (HDR): This precise repair mechanism utilizes a donor template with homologous sequences flanking the DSB to accurately repair the break [79] [38]. Unlike NHEJ, HDR can introduce specific genetic modifications—such as point mutations, gene insertions, or gene corrections—with high fidelity [79]. However, HDR is inherently less efficient than NHEJ and is restricted primarily to the S and G2 phases of the cell cycle when a sister chromatid is available [79].
Alternative Repair Pathways: MMEJ and SSA
Beyond NHEJ and HDR, two alternative pathways contribute to the complex landscape of DSB repair:
Microhomology-Mediated End Joining (MMEJ): This pathway relies on the annealing of short microhomologous sequences (2-20 nucleotides) flanking the broken junction, frequently resulting in deletions [80]. It is considered a "backup" pathway but can significantly impact editing outcomes.
Single-Strand Annealing (SSA): The SSA pathway utilizes Rad52-dependent annealing of longer homologous sequences for DSB repair [80]. In CRISPR-mediated editing, SSA can lead to imprecise donor integration and specific faulty repair patterns like asymmetric HDR [80].
The following diagram illustrates the competitive interplay between these four repair pathways following a CRISPR-induced double-strand break:
Methodologies for Balancing NHEJ vs. HDR
Strategic Inhibition of Competing Pathways
A primary approach to enhance HDR efficiency involves suppressing the dominant NHEJ pathway. However, as our understanding of repair mechanisms deepens, targeting alternative pathways like MMEJ and SSA has shown promise in further improving precise editing outcomes.
Table 1: Small Molecule Inhibitors for DNA Repair Pathway Manipulation
| Target Pathway | Inhibitor Name | Molecular Target | Effect on Editing | Key Considerations |
|---|---|---|---|---|
| NHEJ | Alt-R HDR Enhancer V2 | DNA-PKcs | Increases HDR frequency ~3-fold [80] | Risk of large structural variations [81] |
| NHEJ | AZD7648 | DNA-PKcs | Promotes HDR | Aggravates genomic aberrations [81] |
| MMEJ | ART558 | POLQ | Reduces large deletions & complex indels [80] | Protective against kb-scale deletions [81] |
| SSA | D-I03 | Rad52 | Reduces asymmetric HDR [80] | Effect depends on DNA cleavage ends [80] |
Cell Cycle Synchronization and Other Approaches
Since HDR is most active in the S and G2 phases of the cell cycle, synchronizing cells to these phases can significantly enhance HDR efficiency [81]. This can be achieved through chemical treatments like thymidine or nocodazole, which arrest cells at specific cell cycle checkpoints.
Additional innovative strategies include:
- Fusion proteins: Tethering NHEJ-inhibiting domains (e.g., dominant-negative 53BP1) directly to Cas9 to locally manipulate repair outcomes [81].
- Donor template design: Optimizing the design and delivery of donor templates, such as using single-stranded oligodeoxynucleotides (ssODNs) or double-stranded DNA templates with extended homology arms [79].
- Cas nuclease modification: Using engineered Cas9 variants known as "high-fidelity" Cas9 to reduce off-target effects, though these may still introduce on-target aberrations [81].
The experimental workflow below outlines a typical protocol for enhancing HDR efficiency while monitoring for unintended consequences:
The Risk Landscape: Unintended Consequences of Repair Pathway Manipulation
Structural Variations and Chromosomal Aberrations
A pressing challenge in therapeutic genome editing is the occurrence of large, unintended structural variations (SVs) at on-target sites. These include:
- Kilobase- to megabase-scale deletions at the target site [81]
- Chromosomal translocations between the target site and off-target sites [81]
- Chromosomal losses or truncations, and even chromothripsis [81]
Notably, strategies aimed at enhancing HDR by inhibiting NHEJ can exacerbate these issues. The use of DNA-PKcs inhibitors, while boosting HDR rates, has been shown to significantly increase the frequency of both large-scale deletions and chromosomal translocations—in some cases by a thousand-fold [81].
Limitations of Standard Analysis Methods
Traditional short-read amplicon sequencing, commonly used to assess editing outcomes, often fails to detect these large SVs because the primer binding sites themselves may be deleted [81]. This limitation leads to an overestimation of HDR efficiency and a dangerous underestimation of genotoxic risks. More comprehensive methods like long-read amplicon sequencing (PacBio), CAST-Seq, and LAM-HTGTS are required for a complete safety assessment [80] [81].
Table 2: Genomic Aberrations in CRISPR Editing and Detection Methods
| Type of Aberration | Description | Detection Method | Impact on Safety & Efficacy |
|---|---|---|---|
| Small INDELs | Insertions/deletions <50 bp | Short-read sequencing [81] | Target gene disruption |
| Large Deletions | Kilobase- to megabase-scale losses | Long-read sequencing, CAST-Seq [80] [81] | Loss of regulatory elements, haploinsufficiency |
| Chromosomal Translocations | Exchange of genetic material between chromosomes | CAST-Seq, LAM-HTGTS [81] | Oncogenic potential |
| Asymmetric HDR | Imprecise donor integration (one side only) | Long-read amplicon sequencing [80] | Partial or dysfunctional gene integration |
| Complex Indels | Multiple rearrangements at cut site | Long-read amplicon sequencing [80] | Unpredictable gene function |
The Scientist's Toolkit: Essential Reagents for HDR Optimization
Table 3: Key Research Reagent Solutions for HDR Optimization Studies
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| Lipid Nanoparticles (LNPs) | In vivo delivery of CRISPR components; natural liver tropism [12] | Systemic delivery for liver-targeted editing (e.g., CTX310 for ANGPTL3) [82] |
| Alt-R HDR Enhancer V2 | NHEJ pathway inhibitor to enhance HDR efficiency [80] | Increasing precise knock-in rates in cell cultures |
| ART558 | POLQ inhibitor for MMEJ pathway suppression [80] | Reducing large deletions at the target site |
| D-I03 | Rad52 inhibitor for SSA pathway suppression [80] | Reducing asymmetric HDR and other imprecise integrations |
| Long-Read Sequencing | Comprehensive analysis of editing outcomes, including large SVs [80] | Safety assessment after editing with repair pathway modulators |
| Electroporation System | Physical delivery method for RNP complexes and donor DNA [80] | Knock-in experiments in hard-to-transfect cells (e.g., RPE1) |
Clinical Implications and Future Perspectives
The balance between achieving therapeutic efficacy and minimizing genotoxic risks represents the central challenge in clinical genome editing. The first approved CRISPR therapy, Casgevy (exa-cel) for sickle cell disease and beta-thalassemia, demonstrates this principle in action [12] [82]. However, as editing strategies become more complex—particularly with the rise of in vivo editing for common conditions like cardiovascular disease—comprehensive safety assessment becomes paramount [82].
Future directions focus on developing safer editing platforms:
- High-fidelity Cas variants with reduced off-target activity [81]
- Base and prime editing systems that avoid DSBs altogether [18]
- Novel delivery systems with improved tissue specificity [12]
- Multi-pathway inhibition strategies (e.g., combined NHEJ and MMEJ suppression) to minimize unintended edits while maintaining acceptable HDR levels [80] [81]
The field is moving toward a more nuanced understanding that maximizing HDR efficiency is not always necessary or advisable. In many therapeutic contexts, even moderate editing levels may suffice, particularly if corrected cells gain a selective advantage [81]. The future of safe, effective CRISPR therapeutics will depend on strategic, rather than maximal, manipulation of the DNA repair landscape.
The discovery that Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and the CRISPR-associated protein 9 (Cas9) system could be repurposed from a bacterial immune defense into a revolutionary gene-editing tool represents one of the most significant breakthroughs in modern biology [8] [83]. This natural system in prokaryotes provides adaptive immunity by storing snippets of viral DNA within CRISPR arrays in the host genome; upon subsequent viral exposure, these sequences are transcribed into guide RNAs that direct Cas nucleases to cleave matching foreign DNA, thereby neutralizing the threat [8] [5]. The pivotal realization that this system could be programmed to target virtually any DNA sequence of choice has catapulted CRISPR-Cas9 into the forefront of biomedical research, earning Emmanuelle Charpentier and Jennifer Doudna the Nobel Prize in Chemistry in 2020 [8].
The technology's leap from a fundamental biological mechanism to a powerful "genetic scissors" for precise genome manipulation has opened up unprecedented possibilities for treating genetic diseases, advancing basic research, and modifying crops [84] [85]. However, this immense power brings profound ethical responsibilities, particularly concerning applications that permanently alter the human genome. The birth of babies from genome-edited human embryos in 2018 sparked intense international criticism and highlighted the urgent need for ethical boundaries [8]. This article examines the resulting moratorium on heritable human genome edits and the critical role of informed consent, framing these ethical pillars within the broader context of CRISPR's journey from bacterial immunity to a tool that can reshape the human future.
Historical Context: The Evolution of a Technology
The development of CRISPR-Cas9 from an obscure genetic sequence to a precise gene-editing technology unfolded over three decades through the contributions of scientists worldwide. The timeline below summarizes key milestones, illustrating the collaborative and incremental nature of this scientific discovery.
Table 1: Key Historical Milestones in CRISPR-Cas9 Development
| Year | Key Discovery | Principal Researcher(s) | Significance |
|---|---|---|---|
| 1987 | Identification of unusual repetitive sequences in E. coli | Ishino et al. [8] | Initial discovery of what would later be known as CRISPR; function unknown. |
| 2000-2005 | Term "CRISPR" coined; hypothesized as adaptive immune system | Francisco Mojica [8] [5] | Recognized common features across species and proposed the immune function. |
| 2005 | Identification of Cas9 and Protospacer Adjacent Motif (PAM) | Alexander Bolotin [5] | Discovered the key nuclease (Cas9) and the PAM sequence essential for target recognition. |
| 2007 | Experimental proof of adaptive immunity in bacteria | Rodolphe Barrangou, Philippe Horvath [8] [5] | First experimental demonstration that CRISPR provides resistance to viruses in prokaryotes. |
| 2011 | Discovery of tracrRNA | Emmanuelle Charpentier [8] [5] | Identified the second essential RNA component (tracrRNA) for the Cas9 system. |
| 2012 | Reprogramming of CRISPR-Cas9 for gene editing in vitro | Charpentier, Doudna, and Siksnys [8] [5] | Demonstrated that Cas9 could be programmed with a guide RNA to cut any DNA target in vitro. |
| 2013 | Adaptation for genome editing in human and mouse cells | Feng Zhang, George Church [5] | Successfully harnessed CRISPR-Cas9 for precise genome engineering in eukaryotic cells. |
This progression from basic science to a transformative technology was not linear. Early research was driven by curiosity about a peculiar genetic feature, with its function remaining elusive for years. Francisco Mojica's persistence was crucial in recognizing CRISPR as a distinct class of sequences and, later, in hypothesizing its immune function [8] [5]. The applied potential became clear with the work of Barrangou and Horvath, who showed that the dairy bacterium Streptococcus thermophilus could be "vaccinated" against phages by incorporating new spacers into its CRISPR locus [8]. The final mechanistic pieces fell into place with the characterization of the crRNA and tracrRNA, which were fused into a single-guide RNA (sgRNA) by Charpentier and Doudna, simplifying the system into a two-component tool [5]. The subsequent demonstrations that this system could function heterologously in other species and, most importantly, in human cells, opened the floodgates for global adoption in biomedical research [5].
The Ethical Imperative: Germline Editing and the Moratorium
Defining the Ethical Problem
The application of CRISPR-Cas9 in human germline cells—which include sperm, eggs, and embryos—poses a unique and profound ethical challenge because edits in these cells are heritable, meaning they can be passed down to all subsequent generations [85]. This permanence and potential to alter the human gene pool differentiate it from somatic cell editing, which affects only the individual patient and is widely considered ethically permissible for therapeutic purposes [86]. The core ethical concerns surrounding heritable genome editing include:
- Off-Target Effects: The CRISPR-Cas9 system, while highly precise, can occasionally cleave DNA at unintended, off-target sites in the genome [85] [87]. The introduction of such unintended mutations into the germline carries the risk of causing new genetic diseases that could persist in the population.
- Eugenics and Social Justice: There is a legitimate concern that the technology could be co-opted for non-therapeutic enhancement, such as selecting for traits like intelligence or physical appearance, leading to a new form of eugenics and exacerbating social inequality [85].
- Uncertain Long-Term Consequences: The complex interactions within the human genome are not fully understood. A deliberate edit intended to correct one condition could have unforeseen pleiotropic effects on other biological processes in future generations [85].
- Informed Consent for Future Generations: A fundamental principle of medical ethics is that subjects must provide informed consent for treatments. However, it is impossible to obtain consent from the unborn future generations who will carry and be affected by the genetic modifications [85].
The international scientific community's widespread disapproval crystallized following the 2018 announcement by He Jiankui of the birth of the first gene-edited babies. This event was a catalyst, prompting urgent calls for a global moratorium on all clinical uses of heritable germline editing until technical and ethical issues are resolved, and international consensus is established [8].
The Technical Hurdles: Safety and Efficacy
The ethical concerns are inextricably linked to persistent technical challenges. While viral vectors like Adeno-associated virus (AAV) are commonly used for delivery in somatic therapies, their use in germline editing requires absolute certainty to avoid unforeseen consequences [87]. The two primary DNA repair pathways—Non-Homologous End Joining (NHEJ) and Homology-Directed Repair (HDR)—introduce variability. NHEJ is error-prone and can lead to small insertions or deletions (indels) that disrupt the target gene, while HDR, used for precise correction, is less efficient [84] [88]. The risk of mosaicism, where only a subset of cells in an edited embryo carries the intended modification, further complicates the clinical picture and poses a significant safety risk [8].
The Scientist's Toolkit: Research Reagents and Bioinformatics
Navigating the technical and ethical landscape of CRISPR research requires a suite of specialized tools and reagents. The table below details essential components for a typical CRISPR-Cas9 experiment.
Table 2: Essential Research Reagent Solutions for CRISPR-Cas9 Experiments
| Item | Function/Description | Key Considerations |
|---|---|---|
| Cas9 Nuclease | The enzyme that creates a double-strand break in the target DNA. | Can be wild-type SpCas9 or engineered high-fidelity versions (e.g., eSpCas9, SpCas9-HF1) to reduce off-target effects [88]. |
| Guide RNA (gRNA) | A synthetic RNA composed of a scaffold (for Cas9 binding) and a ~20 nt spacer that defines the genomic target. | Design is critical for specificity and efficiency. Must be unique in the genome and located adjacent to a PAM [88]. |
| Delivery Vector | A vehicle to introduce CRISPR components into cells. | Options include plasmids, lentiviruses, and adenoviruses for in vitro work, and AAV or non-viral vectors for in vivo use [87]. |
| HDR Template | A donor DNA template containing the desired edit, flanked by homology arms. | Used for precise gene correction or insertion. Can be a single-stranded oligodeoxynucleotide (ssODN) or a double-stranded DNA plasmid [88]. |
| Bioinformatics Tools | Computational software for experiment design and analysis. | Tools like CHOPCHOP and CRISPResso are vital for gRNA design, off-target prediction (e.g., Cas-OFFinder), and analyzing sequencing data to quantify editing efficiency [89]. |
Bioinformatics tools are indispensable for a responsible and efficient CRISPR workflow. They help researchers select gRNAs with maximal on-target activity and minimal potential for off-target effects, a key step in risk mitigation [89]. Furthermore, analysis tools are required to validate editing outcomes and quantify the frequency of indels or precise edits in a pool of cells [89]. The continuous development of these tools is essential for advancing the safety and precision of CRISPR applications.
Methodologies: Experimental Protocols and Workflows
Protocol for a Typical In Vitro CRISPR-Cas9 Knockout Experiment
This protocol outlines the key steps for generating a gene knockout in a cell line using the NHEJ repair pathway.
gRNA Design and Cloning:
- Use bioinformatics tools (e.g., CHOPCHOP) to design a gRNA with a 20-nucleotide spacer sequence that is unique in the genome and located upstream of a 5'-NGG-3' PAM [88].
- Synthesize the gRNA oligonucleotides and clone them into a plasmid vector that also expresses the Cas9 nuclease, often via a U6 promoter for the gRNA and a ubiquitous promoter (e.g., CMV) for Cas9 [88].
Cell Transfection:
- Culture the target cells (e.g., HEK293T) under standard conditions.
- Transfect the CRISPR-Cas9 plasmid construct into the cells using an appropriate method (e.g., lipid-based transfection for immortalized cell lines, electroporation for primary cells) [87].
Validation and Analysis:
- Harvest Genomic DNA: 48-72 hours post-transfection, harvest cells and extract genomic DNA.
- Assay Editing Efficiency: Use the T7 Endonuclease I assay or Tracking of Indels by DEcomposition (TIDE) analysis to detect and quantify the presence of indels at the target site. For absolute precision, perform Sanger sequencing of PCR-amplified target regions and analyze with tools like CRISPResso [89].
- Functional Validation: Confirm the phenotypic knockout via Western blot to check for loss of protein expression or a functional assay relevant to the target gene.
Workflow for Human Embryo Genome Editing (Research Context)
Research on human embryos is strictly regulated and for basic research only. The following workflow is based on methodologies used in pre-clinical studies to understand early human development.
The process begins with the most critical ethical and legal step: obtaining informed consent from donors of the gametes or embryos and securing approval from an institutional oversight body [90]. The CRISPR-Cas9 components are then introduced into the zygote via microinjection, typically in the form of a pre-assembled ribonucleoprotein (RNP) complex for greater precision and reduced off-target effects [8]. The edited embryos are cultured in vitro for a limited period, not exceeding the internationally recognized 14-day limit for human embryo research. Finally, the embryos are comprehensively analyzed at the genomic and, where possible, phenotypic level to assess the efficiency and safety of the editing process before the research is concluded and the embryos are disposed of according to regulatory protocols [8].
The Path Forward: Balancing Innovation with Responsibility
The future of heritable human genome editing hinges on resolving the complex interplay between scientific capability, ethical boundaries, and regulatory frameworks. The current consensus among major scientific bodies, including the International Society for Stem Cell Research (ISSCR), advocates for a cautious approach, supporting research but opposing clinical application at this time [86]. Key considerations for the path forward include:
- Strengthening Technical Safety: Ongoing research is focused on developing next-generation editors with higher fidelity and specificity, such as high-fidelity Cas9 variants and base editors, which can reduce off-target effects and eliminate the need for double-strand breaks [88]. Improving the efficiency of HDR is also a major focus to enable more precise corrections.
- Establishing Robust Regulatory Pathways: Before any clinical application can be considered, national and international regulatory agencies must develop clear pathways for oversight. This includes defining the criteria for safety and efficacy, and determining which, if any, serious genetic conditions would justify the use of germline editing [85].
- Fostering Public Engagement and Global Consensus: The decision to alter the human germline is not one for scientists alone. It requires broad societal discourse and the development of international norms and agreements to prevent irresponsible use and "ethics tourism" where researchers seek permissive regulatory environments [85].
The journey of CRISPR from an obscure bacterial immune system to a technology that forces humanity to confront its own evolutionary future is a testament to the power of basic scientific research. As the technology continues to evolve, the principles of a moratorium on heritable edits and rigorous informed consent will remain essential guides, ensuring that scientific progress is matched by a steadfast commitment to ethical responsibility.
Proving Efficacy and Value: Clinical Validation and Technology Comparison
The treatment of hereditary transthyretin amyloidosis (hATTR) has undergone a revolutionary shift with the development of therapies capable of achieving sustained, profound reduction of the pathogenic transthyretin (TTR) protein. The pursuit of ≥90% protein reduction represents a critical efficacy benchmark in hATTR clinical trials, a therapeutic strategy that parallels the precision-based approaches pioneered by gene-editing technologies. This paradigm has roots in the evolving understanding of biological systems, notably the CRISPR-Cas microbial adaptive immune system, which demonstrated the therapeutic potential of highly specific genetic targeting [8] [5] [91]. Just as CRISPR systems evolved in prokaryotes to recognize and eliminate specific genetic invaders [91], modern hATTR therapies are designed to precisely target the root cause of disease—whether by stabilizing the TTR tetramer or reducing its production at the genetic level.
The molecular pathogenesis of hATTR amyloidosis involves the dissociation, misfolding, and aggregation of mutant TTR protein into amyloid fibrils, which deposit in tissues and cause progressive organ dysfunction [92] [93]. The dissociation of the TTR tetramer is the crucial rate-limiting step for amyloid fibril formation [93]. This understanding has informed two primary therapeutic strategies: TTR stabilizers that prevent tetramer dissociation, and TTR "knock-down" agents that reduce the production of the protein precursor, with the latter approach demonstrating the capacity to achieve the >90% reduction benchmark that correlates with improved clinical outcomes [92] [94].
Molecular Mechanisms of hATTR Amyloidosis
TTR Tetramer Destabilization and Fibrillogenesis
The process of TTR amyloid formation follows a complex pathogenic cascade that begins with the destabilization of the native TTR tetramer, leading to dissociation into monomers that misfold into amyloidogenic intermediates [93]. These misfolded monomers aggregate into oligomers and protofibrils, which subsequently assemble into mature amyloid fibrils that deposit in target tissues, particularly the heart and peripheral nerves [92] [93]. The kinetics of amyloid formation exhibit sigmoidal characteristics with three distinct phases: nucleation (lag phase), growth (exponential elongation), and saturation (plateau phase) [93]. This process is dramatically accelerated by the presence of preformed fibrils that act as seeds for further aggregation, creating a self-propagating cycle of amyloid deposition [93].
Tissue Damage Mechanisms
The pathogenic effects of TTR amyloid deposits result from both physical disruption of tissue architecture and direct proteotoxicity. Amyloid infiltration leads to mass effect with disruption of normal tissue structure and function [95]. At the cellular level, TTR amyloid toxicity induces oxidative stress in cardiomyocytes, alters mitochondrial function, and disrupts cytoplasmic calcium homeostasis, contributing to cardiac dysfunction [93]. Transcriptional sequencing and cytokine proteomic analysis of cardiac fibroblasts exposed to TTR deposits have revealed upregulation of inflammatory genes, potentially exacerbating cardiac inflammation and subsequent fibrosis [93].
Figure 1: Molecular Pathogenesis of hATTR Amyloidosis. The cascade begins with TTR tetramer destabilization and progresses through misfolding, aggregation, and tissue deposition, culminating in multiple mechanisms of cellular damage.
Historical Context: From Bacterial Immunity to Therapeutic Gene Modulation
The conceptual foundation for targeted protein reduction therapies traces back to the discovery and characterization of the CRISPR-Cas system in prokaryotes. Initially observed as unusual repetitive DNA sequences in Escherichia coli in 1987 by Ishino and colleagues, the true function of these sequences remained enigmatic for nearly two decades [8] [5]. In 2005, Francisco Mojica's pivotal insight that these sequences matched snippets from bacteriophage genomes led to the correct hypothesis that CRISPR constitutes an adaptive immune system in microbes [5]. This period also saw independent confirmation of this hypothesis by Bolotin, who discovered the Cas9 protein and its associated protospacer adjacent motif (PAM) in Streptococcus thermophilus [5].
The subsequent elucidation of the CRISPR system's mechanism revealed a strikingly precise biological targeting system: upon viral infection, bacteria incorporate fragments of viral DNA into their CRISPR loci as "spacers"; these sequences are then transcribed into guide RNAs that direct Cas proteins to recognize and cleave complementary invading DNA sequences during future infections [8] [91]. The period from 2008-2012 witnessed rapid advancements in understanding the molecular details, including the demonstration that CRISPR targets DNA (Marraffini and Sontheimer, 2008), the discovery of tracrRNA (Charpentier, 2011), and the revolutionary reconstitution of the CRISPR-Cas9 system for programmable gene editing (Doudna and Charpentier, 2012) [8] [5].
This foundational knowledge catalyzed the development of two transformative therapeutic platforms: direct gene editing using CRISPR-based technologies, and gene silencing using RNA interference approaches. The latter has yielded the most immediately applicable results for hATTR amyloidosis, with siRNA and antisense oligonucleotide therapies demonstrating the capacity to achieve the >90% TTR reduction benchmark that forms the focus of this review.
Therapeutic Classes and Efficacy Benchmarks
TTR Stabilizers
TTR stabilizers constitute the first class of disease-modifying therapies developed for hATTR amyloidosis. These small molecule drugs function by binding to the TTR tetramer and increasing its structural stability, thereby preventing dissociation into amyloidogenic monomers [92].
Table 1: TTR Stabilizers in hATTR Amyloidosis
| Drug | Mechanism | TTR Reduction | Clinical Trial Evidence | Key Outcomes |
|---|---|---|---|---|
| Tafamidis | Selective TTR tetramer stabilizer binding to T4 site | Minimal reduction (stabilizes existing tetramers) | ATTR-ACT (N=441; 30 months): Phase 3 RCT in ATTR-CM [92] | Lower all-cause mortality (HR 0.70) & CV hospitalizations; slower functional decline [92] [94] |
| Acoramidis (AG10) | Selective TTR stabilizer mimicking protective T119M mutation | Minimal reduction (stabilizes existing tetramers) | ATTRibute-CM (N=632; 30 months): Phase 3 RCT [92] | Lower all-cause mortality & CV hospitalizations; similar AE profile to placebo [92] |
| Diflunisal | Non-selective NSAID TTR stabilizer | Minimal reduction (stabilizes existing tetramers) | Retrospective analyses & single-arm studies [92] | Slowed disease progression in observational studies; limited by NSAID side effects [92] |
While TTR stabilizers have demonstrated clinical benefits, they primarily function to prevent further amyloid formation rather than reducing the production of new TTR protein. This limitation prompted the development of more targeted approaches capable of achieving profound reduction of TTR synthesis.
TTR Gene Silencing Therapies
TTR gene silencing therapies represent a more direct approach to reducing the source of pathogenic protein by targeting TTR mRNA, thereby preventing its translation into protein. This class includes both small interfering RNA (siRNA) and antisense oligonucleotide (ASO) platforms.
Table 2: TTR Gene Silencing Therapies
| Drug | Mechanism | TTR Reduction | Clinical Trial Evidence | Key Outcomes |
|---|---|---|---|---|
| Patisiran | siRNA targeting TTR mRNA | ~80-90% reduction | APOLLO (N=225; 18 months): Phase 3 RCT [94] | Improved neuropathy, quality of life, and functional capacity; reduced mortality [94] |
| Vutrisiran | siRNA with enhanced stabilin chemistry | ~90% sustained reduction | HELIOS-A (N=164; 18 months): Phase 3 RCT [92] [94] | Similar efficacy to patisiran with potential for less frequent dosing [92] |
| Inotersen | 2'-MOE ASO targeting TTR mRNA | ~70-80% reduction | NEURO-TTR (N=172; 15 months): Phase 3 RCT [94] | Improved neuropathy progression; requires regular monitoring for thrombocytopenia/glomerulonephritis [94] |
| Eplontersen | 2'-MOE ASO with GalNAc conjugate | ~80-90% reduction | Phase 3 trial (ongoing) [94] | Promising sustained reduction with monthly dosing [94] |
The capacity of these gene silencing therapies to achieve sustained ≥90% TTR reduction represents a significant milestone in the treatment of hATTR amyloidosis. A recent meta-analysis of randomized controlled trials confirmed that TTR-targeting therapies are associated with significant reduction in all-cause mortality (RR 0.70; 95% CI 0.60, 0.83; p < 0.01) with both stabilizers and knock-down therapies showing effective reductions [94].
Emerging Therapeutic Approaches
The therapeutic landscape for hATTR amyloidosis continues to evolve with several innovative approaches in development:
- CRISPR-Cas9 Gene Editing: Currently in early research stages, this approach aims to directly correct or disrupt the mutant TTR gene in hepatocytes, potentially offering a one-time curative treatment [92] [93].
- Monoclonal Antibodies Targeting Amyloid Deposits: These investigational therapies, known as "TTR depleters," aim to directly clear existing amyloid fibrils from tissues by using monoclonal antibodies that recognize and promote removal of amyloid deposits [92].
- Combination Therapies: Simultaneous targeting of multiple steps in the amyloid cascade (e.g., stabilization of circulating TTR combined with suppression of new TTR production) may provide synergistic benefits, particularly for patients with advanced disease [92].
Experimental Protocols and Methodologies
Quantification of TTR Reduction
The accurate measurement of TTR protein levels in clinical trials requires highly specific and sensitive methodologies. Two principal techniques are employed:
Immunoturbidimetric Assay for Serum TTR Quantification
- Principle: Measures TTR concentration in serum based on antigen-antibody reaction and turbidity measurement [92]
- Procedure: Serum samples are mixed with anti-TTR antibodies; the resulting complex formation increases solution turbidity proportional to TTR concentration; measured spectrophotometrically at 340 nm [92]
- Standards: Calibrated against WHO international reference standard for prealbumin
- Limitations: Cannot distinguish between wild-type and mutant TTR; measures concentration but not thermodynamic stability
Mass Spectrometry-Based TTR Quantification
- Principle: Uses stable isotope dilution mass spectrometry with synthetic reference peptides as internal standards [96]
- Procedure: TTR is immunoprecipitated from serum; digested with trypsin; analyzed by LC-MS/MS with synthetic isotopically-labeled TTR peptides; quantification based on light-to-heavy peptide ratio [96]
- Advantages: Can quantify specific TTR variants and post-translational modifications; higher specificity than immunoassays [96] [97]
- Applications: Particularly valuable for clinical trials requiring precise quantification of TTR reduction and monitoring of therapy compliance [96]
Assessment of Clinical Efficacy Endpoints
Clinical trials of hATTR therapies employ comprehensive endpoint assessments to evaluate treatment efficacy:
Neurological Assessment
- mNIS+7: Modified Neuropathy Impairment Score +7 composite score evaluating muscle strength, sensation, and reflexes [94]
- Norfolk QoL-DN: Quality of Life-Diabetic Neuropathy questionnaire assessing physical functioning, symptoms, and activities of daily living [94]
- NIS-LL: Neuropathy Impairment Score in the Lower Limbs [94]
Cardiac Assessment
- Echocardiography: Measures left ventricular wall thickness, strain imaging, and diastolic function parameters [92] [94]
- Cardiac Biomarkers: High-sensitivity troponin T and N-terminal pro-B-type natriuretic peptide (NT-proBNP) for monitoring cardiac stress and injury [92]
- Cardiac MRI: Provides tissue characterization including extracellular volume fraction and late gadolinium enhancement [92]
Global Assessment
- 6-Minute Walk Test: Functional capacity assessment [92]
- Composite Endpoints: All-cause mortality, cardiovascular hospitalizations, and change from baseline in functional capacity [92] [94]
Figure 2: Clinical Trial Workflow for hATTR Therapies. Schematic representation of key phases in clinical trial design from patient screening through endpoint assessment.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for hATTR Therapeutic Development
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| TTR Protein Assays | Immunoturbidimetric kits, ELISA kits, Mass spectrometry internal standards | Quantification of TTR concentration in biological samples; monitoring therapeutic efficacy [92] [96] |
| Cell-Based Systems | Hepatocyte cell lines (HepG2, Hep3B), Primary human hepatocytes | In vitro assessment of TTR production, secretion, and gene silencing efficacy [92] |
| Animal Models | Transgenic mice expressing human TTR variants, PrP-TTR transgenic mice | In vivo evaluation of amyloid formation, tissue distribution, and therapeutic response [93] |
| Amyloid Detection Reagents | Congo red, Thioflavin T, Anti-TTR antibodies (immunohistochemistry) | Histological identification and quantification of amyloid deposits in tissues [93] |
| Gene Expression Tools | TTR siRNA libraries, CRISPR-Cas9 gene editing constructs, qPCR primers for TTR mRNA | Molecular assessment of TTR gene expression and modulation [92] [93] |
| Mass Spectrometry Tags | Isotopically labeled TTR peptides (AQUA), Elemental mass tags (MSIHC) | Highly specific protein detection and quantification; multiplexed imaging [96] [98] |
The achievement of sustained >90% TTR protein reduction represents a transformative efficacy benchmark in hATTR amyloidosis therapeutics, reflecting the successful translation of fundamental biological principles into clinically meaningful treatments. The evolution of these therapies parallels the journey of CRISPR from a curious bacterial immune system to a precision gene-editing platform, demonstrating how understanding natural biological mechanisms can inspire revolutionary therapeutic approaches.
Current evidence confirms that both TTR stabilizers and gene silencing therapies provide significant clinical benefits, with meta-analyses demonstrating reduced all-cause mortality and cardiovascular hospitalizations [94]. The profound TTR reduction achieved by siRNA and ASO platforms correlates with stabilization or improvement of neurological and cardiac manifestations, fundamentally altering the disease trajectory.
Future directions in hATTR therapeutics include the development of CRISPR-based gene editing approaches that may offer permanent solutions, combination therapies targeting multiple steps in the amyloid cascade, and methods to enhance tissue penetration for more effective clearance of established amyloid deposits [92] [93]. As these innovative therapies progress through clinical development, the ≥90% protein reduction benchmark will continue to serve as a critical efficacy standard, ensuring that new treatments provide meaningful improvements in the lives of patients with this progressive and debilitating disease.
The advent of programmable gene-editing technologies has fundamentally transformed molecular biology, offering unprecedented precision in manipulating the genetic code. This evolution represents a journey from early, cumbersome methods to the current era of highly specific, multiplexable genome engineering. Framed within the broader history of CRISPR's transformation from a bacterial immune system to a revolutionary research tool, this review provides a comparative analysis of the leading genome-editing technologies: Zinc Finger Nucleases (ZFNs), Transcription Activator-Like Effector Nucleases (TALENs), RNA Interference (RNAi), and CRISPR-Cas systems. For researchers and drug development professionals, understanding the specific advantages, limitations, and optimal applications of each tool is critical for designing effective experimental and therapeutic strategies. We examine the mechanisms, experimental protocols, and reagent requirements for each technology, providing a technical guide for their application in basic research and translational medicine.
The Historical Trajectory of CRISPR: From Bacterial Immunity to Gene Editing
The discovery of CRISPR-Cas is a testament to the importance of basic, curiosity-driven research. The journey began in 1987 when unusual repetitive sequences were identified in the E. coli genome [14] [99]. These sequences were later characterized in other bacteria and archaea, and in 2002, they were formally named Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) [8] [5].
A pivotal breakthrough came from Francisco Mojica, who recognized that the spacer sequences between repeats were derived from viral DNA and correctly hypothesized that CRISPR serves as an adaptive immune system in prokaryotes [8] [5]. This was experimentally validated in 2007 by Barrangou and Horvath, who demonstrated that Streptococcus thermophilus could acquire resistance to bacteriophages by integrating new spacers into its CRISPR locus [8] [5].
The development of CRISPR into a programmable gene-editing tool required the elucidation of its molecular mechanism. Key steps included the discovery of the CRISPR RNA (crRNA) by John van der Oost's group [5], the demonstration by Marraffini and Sontheimer that the system targets DNA [8] [5], and the characterization of the Cas9 protein and its requisite Protospacer Adjacent Motif (PAM) by Bolotin and others [8] [5]. In 2011, Emmanuelle Charpentier discovered the trans-activating tracrRNA [8] [5]. The field culminated in 2012 when the teams of Charpentier and Doudna, and independently Siksnys, reconstituted the CRISPR-Cas9 system in vitro, showing it could be programmed with a single guide RNA (sgRNA) to cut any DNA sequence of choice [8] [5]. The following year, Feng Zhang and George Church's labs adapted the system for efficient genome editing in eukaryotic cells, heralding a new era in genetic engineering [5].
Mechanisms of Action and Experimental Protocols
RNA Interference (RNAi)
Mechanism: RNAi is a gene-silencing technology that relies on the introduction of small interfering RNA (siRNA) or microRNA (miRNA) into cells. These short RNA molecules are loaded into the RNA-induced silencing complex (RISC), which uses the RNA as a guide to identify and cleave complementary messenger RNA (mRNA) transcripts. This degradation or translational repression of the target mRNA results in a temporary knockdown of gene expression rather than a permanent knockout [100] [101].
Typical Experimental Workflow:
- Design: Synthesize siRNA duplexes or miRNA mimics with 21-23 nucleotides that are complementary to the target mRNA.
- Delivery: Transfect the siRNA/miRNA into cells using lipid nanoparticles, electroporation, or viral vectors.
- Analysis: Assess gene knockdown efficiency 48-72 hours post-transfection using qRT-PCR (mRNA level) or western blot (protein level).
Programmable Nucleases: ZFNs, TALENs, and CRISPR-Cas
These technologies create permanent changes in the DNA sequence by inducing double-strand breaks (DSBs), which are then repaired by the cell's endogenous repair machinery.
DNA Repair Pathways and Editing Outcomes:
- Non-Homologous End Joining (NHEJ): An error-prone repair pathway that directly ligates the broken ends, often resulting in small insertions or deletions (indels). This can disrupt the coding frame of a gene, leading to a gene knockout [102] [99].
- Homology-Directed Repair (HDR): A precise repair pathway that uses a homologous DNA template, such as an externally supplied donor vector, to repair the break. This allows for specific gene knock-in or correction of mutations [102] [99].
Zinc Finger Nucleases (ZFNs)
Mechanism: ZFNs are fusion proteins comprising a custom zinc-finger protein (ZFP) DNA-binding domain and the cleavage domain of the FokI restriction enzyme. Each zinc finger recognizes a 3-base pair sequence; multiple fingers are assembled to target a longer, unique site (typically 9-18 bp). Because FokI must dimerize to become active, a pair of ZFNs is designed to bind opposite strands of the DNA at the target site, bringing the two FokI domains together to create a DSB [102] [100] [103].
Typical Experimental Workflow:
- Design & Cloning: Identify a target site and assemble the requisite zinc finger arrays using modular assembly or selection-based methods (e.g., OPEN). Fuse the arrays to the FokI nuclease domain in an expression plasmid [102] [100].
- Delivery: Co-transfect the pair of ZFN expression plasmids into target cells. Optionally, a donor DNA template for HDR can be included.
- Validation: Screen for modifications using restriction fragment length polymorphism (RFLP) analysis, T7 endonuclease I assay, or sequencing.
Transcription Activator-Like Effector Nucleases (TALENs)
Mechanism: Similar to ZFNs, TALENs are fusions of a custom DNA-binding domain (from TALE proteins) to the FokI nuclease domain. The key advantage is the simple code governing TALE DNA-binding: each TALE repeat is 33-35 amino acids long and recognizes a single DNA base pair via two hypervariable residues known as the Repeat-Variable Diresidue (RVD). This one-to-one code (e.g., NI for A, HD for C, NG for T, NN for G) makes TALENs easier to design and engineer than ZFNs [102] [100] [103].
Typical Experimental Workflow:
- Design & Cloning: Design a pair of TALE arrays to flank the target site using the RVD code. Assemble the arrays using high-throughput methods like Golden Gate cloning into a TALEN backbone plasmid [102] [100].
- Delivery: Co-transfect the pair of TALEN expression plasmids into target cells, with or without a donor DNA template.
- Validation: Analyze editing efficiency as for ZFNs.
CRISPR-Cas9 System
Mechanism: The CRISPR-Cas9 system is an RNA-guided DNA endonuclease. The core components are the Cas9 nuclease and a single guide RNA (sgRNA). The ~20 nucleotide sequence at the 5' end of the sgRNA directs Cas9 to a specific genomic locus via Watson-Crick base pairing. Cas9 cleaves the DNA only if the target sequence is adjacent to a short Protospacer Adjacent Motif (PAM), which for the commonly used S. pyogenes Cas9 is 5'-NGG-3' [104] [14] [99]. Cas9 contains two nuclease domains, HNH and RuvC, which cleave the complementary and non-complementary DNA strands, respectively, generating a DSB [5] [99].
Typical Experimental Workflow:
- Design & Cloning: Design an sgRNA sequence of ~20 nucleotides that is unique in the genome and precedes a PAM (NGG). The sgRNA sequence is cloned into an expression vector, often containing a U6 promoter.
- Delivery: The sgRNA plasmid (or a synthetic sgRNA) is co-transfected with a Cas9 expression plasmid (or mRNA) into the target cells. Ribonucleoprotein (RNP) complexes of purified Cas9 protein and sgRNA can also be delivered directly via electroporation for higher efficiency and reduced off-target effects [14].
- Validation: Editing efficiency is assessed using the same methods as for ZFNs/TALENs. For HDR, a donor template must be supplied.
Comparative Analysis of Gene-Editing Technologies
The following tables provide a detailed, side-by-side comparison of the key technical and practical features of ZFNs, TALENs, RNAi, and CRISPR-Cas9.
Table 1: Core Mechanisms and Technical Specifications
| Feature | ZFNs | TALENs | RNAi | CRISPR-Cas9 |
|---|---|---|---|---|
| Core Component | Protein (Zinc Finger-FokI) | Protein (TALE-FokI) | RNA (siRNA/miRNA) | RNA (sgRNA) & Protein (Cas9) |
| Targeting Molecule | Protein-DNA interaction | Protein-DNA interaction | RNA-RNA complementarity | RNA-DNA complementarity |
| Recognition Site Length | 9-18 bp (per ZFN) [103] | 30-40 bp (per TALEN) [103] | 21-23 nt | 20 nt + PAM (e.g., NGG) [103] |
| Nuclease / Effector | FokI (dimerizes) | FokI (dimerizes) | RISC complex | Cas9 nuclease |
| Primary Outcome | Permanent DNA modification (KO/KI) | Permanent DNA modification (KO/KI) | Transient mRNA knockdown | Permanent DNA modification (KO/KI) |
| Typical Efficiency | Moderate | Moderate to High | Variable, often incomplete | High [105] |
Table 2: Practical Considerations for Research and Development
| Feature | ZFNs | TALENs | RNAi | CRISPR-Cas9 |
|---|---|---|---|---|
| Ease of Design & Cloning | Challenging; context-dependent effects [102] [100] | Moderate; simple code but repetitive sequences [102] [100] | Very Easy | Very Easy; requires only sgRNA synthesis [105] |
| Cost | High [105] | High [105] | Low | Low [105] |
| Scalability & Multiplexing | Low | Low | High for knockdown | High; ideal for library screens & multi-gene edits [104] [105] |
| Delivery | Plasmid DNA, mRNA | Plasmid DNA, mRNA | RNA oligos, Viral vectors | Plasmid DNA, mRNA, RNP, Viral vectors [14] |
| Key Advantage | High specificity; well-validated | Flexible targeting; simple design | Rapid knockdown; high-throughput | Ease of use; multiplexing; versatility [104] [105] |
| Key Limitation | Difficult design; off-target toxicity [102] [100] | Large size; labor-intensive cloning [105] | Transient effect; off-target silencing | Off-target cuts; PAM requirement [105] [101] |
The Scientist's Toolkit: Essential Research Reagents
Successful genome editing requires a suite of well-characterized reagents. The table below details essential materials and their functions for experiments utilizing these technologies.
Table 3: Key Research Reagent Solutions
| Reagent / Tool | Function in Experiment | Technology Platform |
|---|---|---|
| FokI Nuclease Domain | Catalyzes DNA double-strand break; requires dimerization. | ZFNs, TALENs [102] [100] |
| Zinc Finger Array | Binds to specific 3-bp DNA triplets; confers target specificity. | ZFNs [102] [100] |
| TALE Repeat Array | Binds to single DNA base pairs via RVD code; confers target specificity. | TALENs [102] [100] |
| Cas9 Nuclease (WT) | RNA-guided DNA endonuclease; creates DSBs at target sites. | CRISPR-Cas9 [5] [14] |
| Guide RNA (sgRNA) | Combines crRNA and tracrRNA function; directs Cas9 to DNA target. | CRISPR-Cas9 [5] [99] |
| Donor DNA Template | Provides homologous sequence for precise HDR-mediated editing (knock-in). | ZFNs, TALENs, CRISPR-Cas9 [102] |
| High-Fidelity Cas9 (e.g., HF-Cas9, HypaCas9) | Engineered variant with reduced off-target activity. | CRISPR-Cas9 [14] [103] |
| Cas9 Nickase | Mutant Cas9 (e.g., D10A) that cuts only one DNA strand; used in pairs for higher specificity. | CRISPR-Cas9 [99] [103] |
| Dead Cas9 (dCas9) | Catalytically inactive Cas9; used for gene regulation (CRISPRi/a) without cleavage. | CRISPR-Cas9 [99] [103] |
| Base Editors (e.g., ABE, CBE) | dCas9 fused to deaminase enzymes; enables direct, precise single-base changes without DSBs. | CRISPR-Cas9 [105] [14] |
The landscape of gene-editing technologies has progressed dramatically, from the protein-centric engineering of ZFNs and TALENs to the RNA-guided simplicity of CRISPR-Cas9. While ZFNs and TALENs demonstrated that targeted genome editing was possible and remain valuable for certain high-specificity niche applications, their complexity and cost limited widespread adoption [102] [105]. RNAi continues to be a powerful tool for rapid, reversible gene knockdown but is unsuitable for permanent genetic modification.
The CRISPR-Cas9 system has democratized gene editing due to its unparalleled ease of design, low cost, and exceptional versatility [104] [105] [99]. Its ability to be easily multiplexed and adapted into diverse platforms, such as base editing and transcriptional control, has solidified its role as the preeminent tool for both basic research and therapeutic development. The ongoing refinement of CRISPR systems, including the reduction of off-target effects and expansion of PAM compatibility, promises to further accelerate innovation. For the research and drug development community, the choice of technology is now context-dependent, but CRISPR-Cas9 stands as the transformative workhorse that is shaping the present and future of genetic engineering.
The emergence of CRISPR-Cas9 as a powerful genome-editing tool represents one of the most significant biotechnology breakthroughs of the 21st century, earning researchers Emmanuelle Charpentier and Jennifer Doudna the Nobel Prize in Chemistry in 2020 [8]. This technology, often termed "genetic scissors," has evolved from its original biological function as a prokaryotic immune system that protects bacteria and archaea from mobile genetic elements like viruses [8]. The journey from fundamental bacterial immunity to applied gene editing has created an urgent need for robust regulatory frameworks that can ensure patient safety without stifling innovation.
For researchers and drug development professionals working with CRISPR-based therapies, genotoxicity assessment presents particular challenges. These assessments must evaluate potential off-target effects and unintended consequences of genome manipulation while adhering to established regulatory pathways [106]. The FDA and EMA have developed comprehensive guidelines for genotoxicity testing of pharmaceuticals, primarily through the ICH S2(R1) guideline, which aims to "optimize the standard genetic toxicology battery for prediction of potential human risks" [107] [108]. This technical guide examines current regulatory requirements within the context of rapidly evolving gene-editing technologies, providing a roadmap for compliance and safety assessment.
Historical Context: From Bacterial Immunity to Genetic Engineering
The Natural History of CRISPR-Cas Systems
The discovery of CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) began in 1987 when Japanese researchers first observed unusual repetitive DNA sequences in Escherichia coli [8]. However, the functional significance remained mysterious until 2005, when Francisco Mojica at the University of Alicante recognized that these sequences matched snippets from bacteriophage genomes, leading him to correctly hypothesize that CRISPR is an adaptive immune system in prokaryotes [5]. Around the same time, Alexander Bolotin at the French National Institute for Agricultural Research discovered the Cas9 protein in Streptococcus thermophilus and noted the presence of a specific sequence motif adjacent to viral DNA fragments—now known as the Protospacer Adjacent Motif (PAM), essential for target recognition [5].
Key milestones in elucidating the CRISPR mechanism include:
- 2007: Experimental demonstration by Philippe Horvath and Rodolphe Barrangou of Danisco that CRISPR systems provide adaptive immunity against viruses in prokaryotes [5]
- 2008: John van der Oost's discovery that spacer sequences are transcribed into small CRISPR RNAs (crRNAs) that guide Cas proteins to target DNA [5]
- 2011: Emmanuelle Charpentier's identification of tracrRNA (trans-activating CRISPR RNA), essential for processing crRNA [5]
- 2012: Charpentier and Doudna's collaboration demonstrating that crRNA and tracrRNA could be fused into a single guide RNA, significantly simplifying the system for practical applications [5]
The natural biological function of CRISPR-Cas systems provided the blueprint for its development as a programmable genome-editing tool. In 2013, Feng Zhang's lab at the Broad Institute successfully adapted CRISPR-Cas9 for genome editing in eukaryotic cells, demonstrating targeted cleavage in human and mouse cells and opening the door to therapeutic applications [5].
The Evolution of Regulatory Science for Advanced Therapies
As CRISPR technology advanced from basic research to clinical applications, regulatory agencies faced the challenge of evaluating safety for increasingly complex therapeutic modalities. The standard genetic toxicology battery described in ICH S2(R1) was designed primarily for traditional small-molecule pharmaceuticals, but its principles remain relevant for assessing gene therapies [107] [108].
The recent case of "Baby KJ," an infant treated with a custom CRISPR therapy for a rare liver disease, illustrates both the promise and regulatory challenges of personalized gene editing [109] [12]. This bespoke therapy was developed, approved by the FDA, and delivered in just six months, demonstrating the need for flexible yet rigorous regulatory pathways for individualized treatments [12]. In response to such cases, the FDA has begun developing new frameworks like the "plausible mechanism" pathway, designed to accelerate treatments for ultra-rare diseases that cannot be tested in traditional large-scale clinical trials [110].
Current Regulatory Framework for Genotoxicity Assessment
ICH S2(R1): The International Standard
The ICH S2(R1) guideline, adopted by both the FDA and EMA, represents the primary regulatory standard for genotoxicity testing of pharmaceuticals intended for human use [107] [108]. This harmonized guideline combines and replaces two previous documents (S2A and S2B) with the goal of "improving risk characterization for carcinogenic effects that have their basis in changes in the genetic material" [108].
Key aspects of the ICH S2(R1) approach include:
- Optimized test battery: A standard genetic toxicology battery designed to predict potential human risks
- Follow-up testing standards: Internationally agreed-upon approaches for additional testing when initial results are positive
- Interpretation guidance: Framework for distinguishing relevant from non-relevant findings [107]
This guidance applies specifically to pharmaceuticals and explicitly states that it "does not apply to biologics" [107], creating potential regulatory gaps for advanced therapy medicinal products (ATMPs) including CRISPR-based therapies.
OECD Test Guidelines and FDA Implementation
The Organisation for Economic Co-operation and Development (OECD) provides globally recognized test guidelines for genotoxicity assessment, which are accepted by both FDA and EMA for some product types [111] [112]. These include:
- OECD TG 471: Bacterial Reverse Mutation Test (Ames test)
- OECD TG 487: In Vitro Mammalian Cell Micronucleus Test
- OECD TG 476: In Vitro Mammalian Cell Gene Mutation Tests
The FDA has implemented a New Alternative Methods Program specifically intended to "spur the adoption of alternative methods for regulatory use that can replace, reduce, and refine animal testing (the 3Rs)" [111]. This program emphasizes qualification of alternative methods for specific contexts of use, similar to how drugs are approved for specific indications [111].
Table 1: Core Genotoxicity Tests and Their Applications in Gene Therapy Development
| Test Method | Regulatory Basis | Key Endpoints | Relevance to CRISPR Therapies |
|---|---|---|---|
| Bacterial Reverse Mutation (Ames) | OECD 471, ICH S2(R1) | Gene mutations in bacterial strains | Assess potential off-target effects on microbial DNA |
| In Vitro Mammalian Cell Micronucleus | OECD 487, ICH S2(R1) | Chromosomal damage, micronucleus formation | Evaluate chromosomal integrity after gene editing |
| In Vitro Mammalian Gene Mutation | OECD 476, ICH S2(R1) | Mutations at specific genetic loci (e.g., HPRT, TK) | Assess specific gene mutations from editing |
| In Vivo Micronucleus Test | OECD 474, ICH S2(R1) | Chromosomal damage in hematopoietic cells | Systemic evaluation of genotoxicity in whole organism |
Genotoxicity Assessment of CRISPR-Based Therapies
Specific Considerations for Gene Editing Products
CRISPR-based therapies present unique challenges for genotoxicity assessment due to their mechanism of action, which involves creating double-stranded breaks in DNA [5]. The primary concerns include:
- Off-target effects: Unintended editing at genomic sites with sequence similarity to the target site
- On-target consequences: Unpredictable outcomes at the target site, including large deletions or complex rearrangements
- Long-term genomic instability: Persistent effects following gene editing
Recent preclinical studies of CRISPR therapies have demonstrated approaches to address these concerns. For example, CRISPR Therapeutics' SyNTase Gene Editing Technology for Alpha-1 Antitrypsin Deficiency reported "high levels of editing (up to 95%) in SERPINA1-E342K human hepatocyte cell models without any detectable (<0.5%) off-target effects" [106]. This highlights the importance of comprehensive off-target assessment in relevant cell models.
Emerging Testing Strategies and Platforms
The field of genotoxicity testing is evolving toward more human-relevant and mechanistic approaches. Key innovations include:
- 2D/3D Human Cell Models: Reconstructed human tissues that better mirror in vivo biology [112]
- Advanced imaging techniques: High-content imaging with FISH staining for detailed chromosomal analysis [112]
- Miniaturized, high-throughput assays: 384-well AMES MPF and 24-well MicroNucleus formats that save time and resources [112]
- Computational toxicology: In silico approaches for predicting mutagenic potential [111]
The FDA's Innovative Science and Technology Approaches for New Drugs (ISTAND) pilot program is designed to expand the types of tools acceptable for drug development, potentially including novel genotoxicity assessment methods specifically suited for advanced therapies [111].
Table 2: Advanced Methods for Genotoxicity Assessment of Gene Therapies
| Methodology | Principle | Application in CRISPR Therapy Development | Regulatory Status |
|---|---|---|---|
| High-Content Imaging | Automated microscopy with multiple fluorescent probes | Detection of subtle chromosomal abnormalities after editing | Early adoption, not yet standardized |
| Next-Generation Sequencing | Whole-genome or targeted sequencing approaches | Comprehensive identification of on- and off-target editing effects | Increasingly expected for clinical trials |
| Microphysiological Systems (Organs-on-Chips) | 3D models that simulate human organ biology | Assessment of tissue-specific genotoxic responses | FDA ISTAND program qualification ongoing |
| In Silico Prediction Tools | Computational assessment of off-target propensity | Early screening of guide RNA specificity | Accepted as complementary data |
Experimental Protocols for Genotoxicity Assessment
Standard Battery Testing Workflow
The following diagram illustrates a comprehensive testing strategy for CRISPR-based therapies, integrating standard regulatory requirements with gene-editing specific analyses:
Detailed Methodologies for Key Assays
Bacterial Reverse Mutation Test (Ames Test)
Purpose: To assess the mutagenic potential of CRISPR components or delivery vehicles in bacterial systems [112].
Protocol:
- Strain Selection: Use Salmonella typhimurium strains TA98, TA100, TA1535, TA1537, and E. coli WP2 uvrA
- Metabolic Activation: Include testing with and without S9 liver fraction to simulate mammalian metabolism
- Sample Preparation: Test CRISPR construct, delivery vehicle (e.g., LNP), and complete formulation separately
- Incubation: Plate bacteria with test article and incubate at 37°C for 48-72 hours
- Analysis: Count revertant colonies; positive result indicated by dose-dependent increase
Interpretation: While not directly assessing genome editing, this test identifies potential mutagenic effects of delivery components or unexpected chemical activities associated with the therapeutic formulation.
In Vitro Mammalian Cell Micronucleus Test
Purpose: To detect chromosomal damage caused by off-target CRISPR activity or delivery system toxicity [112].
Protocol:
- Cell Culture: Use human lymphocytes or appropriate mammalian cell lines (e.g., TK6 cells)
- Dosing: Expose cells to CRISPR therapeutic across a concentration range for 3-6 hours with and without metabolic activation
- Recovery: Allow 1.5-2.0 cell cycle periods for micronucleus expression
- Cytochalasin B: Add to block cytokinesis while allowing nuclear division
- Harvest and Stain: Prepare slides and stain with DNA-specific dyes
- Scoring: Count micronuclei in binucleated cells; minimum 2000 cells per concentration
CRISPR-Specific Modifications: Include positive controls specific to nuclease activity (e.g., known clastogens) and extended recovery times to detect delayed genotoxic effects.
Next-Generation Sequencing Off-Target Analysis
Purpose: To comprehensively identify unintended editing events across the genome [106].
Protocol:
- Guide RNA Design: Include bioinformatic prediction of potential off-target sites
- Cell Transfection: Deliver CRISPR therapeutic to relevant human cell types
- Genomic DNA Extraction: Harvest DNA 72-96 hours post-transfection
- Library Preparation: Use whole-genome sequencing or targeted capture of predicted off-target sites
- Sequencing: Perform high-coverage sequencing (minimum 50x for WGS, 1000x for targeted)
- Variant Calling: Use specialized algorithms (e.g., GATK) to identify editing events
- Validation: Confirm potential off-target sites using orthogonal methods (e.g., digital PCR)
The Scientist's Toolkit: Essential Reagents and Platforms
Table 3: Key Research Reagent Solutions for Genotoxicity Assessment
| Reagent/Platform | Function | Application in Genotoxicity Testing |
|---|---|---|
| Lipid Nanoparticles (LNPs) | In vivo delivery of CRISPR components | Enable efficient editing; themselves require genotoxicity assessment [12] |
| CRISPR-Cas9 Ribonucleoprotein (RNP) | Precomplexed Cas9 and guide RNA | Reduces off-target effects compared to plasmid delivery [106] |
| Ames MPF Kit | Miniaturized bacterial mutation assay | 384-well format reduces test article requirement by 90% [112] |
| Human Stem Cell-Derived Hepatocytes | Metabolically competent human cells | Provides relevant metabolic profile for in vitro testing [111] |
| CometAssay Kit | Single-cell gel electrophoresis for DNA damage | Detects DNA strand breaks at single-cell level [112] |
| Microfluidic Organ-on-Chip Platforms | Physiologically relevant 3D tissue models | Assess tissue-specific genotoxic responses [111] |
Future Directions and Regulatory Evolution
The regulatory landscape for genotoxicity assessment of advanced therapies is rapidly evolving. The FDA's "plausible mechanism" pathway represents a significant shift toward evidence-based flexibility for bespoke therapies targeting ultra-rare diseases [110]. This approach requires:
- Target engagement confirmation: Demonstration that the therapy successfully edits its intended target
- Well-characterized natural history: Historical data on disease progression without intervention
- Ongoing monitoring: Post-administration follow-up to assess long-term safety and efficacy [110]
Simultaneously, international harmonization efforts continue through the OECD, ICH, and ISO, with a clear trend toward human-relevant models and reduced animal testing [111] [112]. The FDA's New Alternative Methods Program explicitly aims to "replace, reduce, and refine animal testing (the 3Rs)" while maintaining rigorous safety standards [111].
For CRISPR-based therapies specifically, the demonstrated ability to redose treatments safely—as shown in both Baby KJ's case and Intellia Therapeutics' hATTR trial—opens new avenues for iterative therapeutic optimization but also requires careful assessment of potential cumulative genotoxic effects [12].
As the field advances, regulatory science will continue to balance the imperative for patient safety with the need to enable transformative therapies for previously untreatable conditions. By understanding both the historical context of CRISPR development and the current regulatory framework, researchers and drug developers can navigate this complex landscape more effectively, bringing safe, effective gene therapies to patients in need.
The global genome editing market is on a trajectory of remarkable growth, driven by technological advancements, increased funding, and rising demand for treatments for genetic disorders. This market is expected to surge from $9.3 billion in 2024 to $23.7 billion by 2030, reflecting a robust compound annual growth rate (CAGR) of 16.9% [113] [114]. This growth is largely fueled by the dominance of CRISPR-Cas9 technology, which has revolutionized genetic engineering due to its simplicity, precision, and cost-effectiveness. North America currently leads the market, with the Asia-Pacific region emerging as a significant growth hub [115] [116].
Market Size and Growth Projections
Recent analyses from leading market research firms consistently project a rapid expansion of the genome editing sector. The table below summarizes the key market forecasts.
Table 1: Global Genome Editing Market Projections
| Report Metric | Details | Source |
|---|---|---|
| Base Year Market Size (2024) | $9.3 Billion | [114] |
| Market Size in 2025 | $10.8 Billion | [113] [114] |
| Projected Market Size (2030) | $23.7 Billion | [113] [114] |
| Forecast Period CAGR | 16.9% (2025-2030) | [113] [114] |
This growth is segmented across various technologies, applications, and end-users. CRISPR technology, in particular, is a major driver and is expected to grow at a CAGR of approximately 15.6% through 2030 [115].
Table 2: Market Segmentation and Key Characteristics
| Segment | Sub-category | Market Share or Key Characteristic |
|---|---|---|
| Technology | CRISPR/Cas9 | Dominant segment due to simplicity, low cost, and high precision [113] [99]. |
| TALENs & ZFNs | Pre-CRISPR technologies that require more complex protein engineering [99]. | |
| Application | Cell Line Engineering | Accounted for over USD 2.2 billion in 2021 [115]. |
| Drug Development & Clinical Therapy | Critical for developing treatments for genetic disorders and cancer [116]. | |
| End-user | Biotech & Pharma Companies | Held over 45.5% market share in 2021 [115]. |
| Academic & Research Institutes | Major drivers of basic research and innovation. | |
| Region | North America | Largest market share (38% in 2021), valued at $4.3B in 2024 [115] [114]. |
| Asia-Pacific | Expected to be the fastest-growing region, led by China's CRISPR advancements [116]. |
A Historical Perspective: From Bacterial Immunity to Gene Editing
The transformative power of genome editing, particularly CRISPR, is rooted in its origins as a bacterial immune system. The journey from a fundamental biological discovery to a Nobel Prize-winning technology provides critical context for its current market potential.
Diagram 1: Natural CRISPR-Cas Adaptive Immunity in Bacteria. This simplified workflow illustrates how prokaryotes acquire immunity to viruses, forming the foundation for gene-editing tools.
Key Discoveries in CRISPR History
The development of CRISPR-Cas9 into a programmable gene-editing tool was built upon decades of foundational research by scientists worldwide [5].
Table 3: History of CRISPR-Cas9 Discovery and Development
| Year(s) | Key Discovery | Lead Researcher(s) | Significance |
|---|---|---|---|
| 1987-1993 | Initial identification of unusual repetitive DNA sequences in E. coli and archaea. | Ishino, Mojica [8] [5] | First observation of what would later be termed CRISPR. |
| 2000-2002 | Term "CRISPR" coined; cas genes identified adjacent to repeats. | Mojica, Jansen [8] [5] | Defined the genetic locus and proposed a common nomenclature. |
| 2005 | Spacers derived from viral DNA; proposed adaptive immune function. | Mojica, Bolotin, Pourcel [8] [5] | Hypothesized the core biological function as an immune defense. |
| 2007 | Experimental proof of adaptive immunity in S. thermophilus. | Barrangou, Horvath [8] [5] | First direct evidence that CRISPR provides resistance to viruses. |
| 2008 | CRISPR sequences processed into guide RNAs (crRNAs). | van der Oost [5] | Identified RNA-guided targeting as the interference mechanism. |
| 2010-2011 | Cas9 identified as the sole nuclease creating double-stranded breaks; tracrRNA discovered. | Moineau, Charpentier [8] [5] | Defined the core two-RNA:one-protein effector complex. |
| 2012 | Programmable CRISPR-Cas9 system developed. crRNA and tracrRNA fused into single-guide RNA (sgRNA). | Doudna, Charpentier, Šikšnys [8] [5] | Critical breakthrough: Created a simplified, programmable system for cutting any DNA sequence. |
| 2013 | First demonstration of CRISPR-Cas9 genome editing in human cells. | Zhang, Church [5] | Proven effective in eukaryotic cells, unleashing potential for human therapy. |
The pivotal moment came in 2012 when Emmanuelle Charpentier and Jennifer Doudna, along with Virginijus Siksnys's group, reconstituted the CRISPR-Cas9 system in vitro and engineered it into a programmable tool [8] [5]. Their key innovation was fusing the two natural RNAs—crRNA and tracrRNA—into a single-guide RNA (sgRNA) [5] [99]. This created a two-component system where the sgRNA directs the Cas9 nuclease to a specific DNA sequence, which Cas9 then cuts. For this discovery, Charpentier and Doudna were awarded the 2020 Nobel Prize in Chemistry [8].
Technical Guide: CRISPR-Cas9 Genome Editing Workflow
The application of CRISPR-Cas9 in a research or therapeutic setting follows a structured workflow. The core mechanism involves the sgRNA-Cas9 complex creating a precise double-strand break (DSB) in the DNA, which the cell's own repair machinery then fixes.
Molecular Mechanism of CRISPR-Cas9
The Cas9 enzyme is a multi-domain nuclease. Its activity is directed by the sgRNA and requires a short Protospacer Adjacent Motif (PAM), typically 5'-NGG-3' for the commonly used S. pyogenes Cas9, adjacent to the target site [8] [99].
- Target Recognition: The sgRNA base-pairs with the target DNA strand (complementary strand).
- DNA Cleavage: The Cas9 enzyme contains two nuclease domains:
- The HNH domain cleaves the target DNA strand complementary to the sgRNA.
- The RuvC domain cleaves the non-complementary DNA strand [99].
- This results in a double-strand break (DSB) 3-4 nucleotides upstream of the PAM site [5].
Experimental Protocol for Targeted Genome Editing
The following diagram and protocol outline a standard workflow for a CRISPR-Cas9 experiment in mammalian cells.
Diagram 2: CRISPR-Cas9 Experimental Workflow. The process from design to validation, highlighting the two key DNA repair pathways that result in different editing outcomes.
Step 1: Target Selection and sgRNA Design
- Identify Target Sequence: Select a 20-nucleotide target sequence adjacent to a 5'-NGG PAM site in your gene of interest.
- sgRNA Design Tools: Use computational algorithms (e.g., from Broad Institute or commercial vendors) to design sgRNAs with high on-target efficiency and minimal off-target effects [99].
- Validate Specificity: BLAST the sgRNA sequence against the host genome to ensure uniqueness.
Step 2: Delivery of CRISPR Components
The engineered sgRNA and Cas9 nuclease must be delivered into the target cells. Common methods include:
- Plasmid Transfection: The genes for Cas9 and sgRNA are cloned into a plasmid vector and introduced into cells via chemical transfection (e.g., lipofection) or electroporation.
- RNA Transfection: In vitro-transcribed sgRNA and Cas9 mRNA are directly delivered, leading to faster expression but being less stable.
- Ribonucleoprotein (RNP) Complex Delivery: Pre-complexed, purified Cas9 protein and sgRNA are electroporated into cells. This is the fastest and most specific method, reducing off-target effects and immune responses [99].
Step 3: Cellular Repair and Genetic Modification
After the Cas9-induced double-strand break, the cell activates one of two endogenous repair pathways:
- Non-Homologous End Joining (NHEJ):
- Mechanism: An error-prone repair pathway that directly ligates the broken DNA ends.
- Outcome: Often results in small insertions or deletions (indels). If these occur in a protein-coding exon, they can disrupt the reading frame, leading to a gene knockout [99].
- Homology-Directed Repair (HDR):
- Mechanism: A precise repair pathway that uses a homologous DNA template to repair the break.
- Outcome: By co-delivering a designed "donor template" DNA molecule, researchers can introduce specific point mutations, insert a gene (e.g., a fluorescent reporter), or correct a pathogenic mutation, achieving precise gene editing or knock-in [99].
Step 4: Validation and Analysis
- Efficiency Assessment: Use mismatch detection assays (e.g., T7E1 assay, TIDE analysis) or next-generation sequencing (NGS) to quantify indel formation.
- Clonal Isolation: Single-cell-derived clones are isolated and expanded.
- Genotypic Confirmation: PCR amplification and Sanger sequencing of the targeted genomic locus to confirm the intended edit.
- Phenotypic Validation: Perform functional assays (e.g., Western blot, immunofluorescence, metabolic assays) to confirm the biological effect of the genetic modification.
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for CRISPR-Cas9 Experiments
| Reagent / Material | Function / Description | Key Considerations |
|---|---|---|
| Cas9 Nuclease | The enzyme that creates double-strand breaks in DNA. | Available as a purified protein, encoded on plasmid DNA, or as mRNA. |
| sgRNA | Synthetic single-guide RNA that directs Cas9 to the target genomic locus. | Can be produced by in vitro transcription or purchased as synthetic RNA. |
| Delivery Vehicles | Methods to introduce components into cells (e.g., electroporation systems, lipid nanoparticles, viral vectors). | Choice depends on cell type (e.g., adherent, suspension, primary cells). |
| HDR Donor Template | A single-stranded or double-stranded DNA molecule containing the desired edit, flanked by homologous arms. | Essential for precise gene correction or knock-in. |
| Cell Culture Media & Supplements | For maintaining and expanding the target cells pre- and post-editing. | Formulation is cell-type specific. |
| Selection Markers | Antibiotics or fluorescent proteins used to enrich for successfully transfected/transduced cells. | Integrated into delivery plasmids or donor templates. |
| Validation Tools | PCR primers, sequencing kits, and antibodies for verifying genetic and phenotypic changes. | Critical for confirming edit specificity and efficiency. |
The genome editing market's trajectory toward $23.7 billion by 2030 is firmly supported by the ongoing technological revolution initiated by CRISPR [113] [114]. Future growth will be fueled by:
- Therapeutic Applications Expansion: Clinical trials for genetic diseases like sickle cell anemia and beta-thalassemia are showing promising results, paving the way for commercial therapies [8] [18].
- Technological Refinements: Innovations like base editing and prime editing offer even greater precision without requiring double-strand breaks, potentially improving safety profiles [18].
- Agricultural and Diagnostic Applications: Use of CRISPR in developing resilient crops and sensitive diagnostic tests (e.g., SHERLOCK for virus detection) expands the market beyond medicine [115] [116].
However, challenges remain, including ensuring specificity to avoid off-target effects, developing efficient and safe delivery systems in vivo, and navigating the complex ethical and regulatory landscape, especially concerning germline editing [8] [99]. Despite these hurdles, the convergence of strong market drivers, continuous technological advancement, and vast unmet medical need positions genome editing as a cornerstone of 21st-century biotechnology and medicine.
The journey from a novel therapeutic concept to an approved treatment is a meticulously structured process defined by distinct clinical trial phases. This whitepaper provides a technical analysis of Phase I through Phase III clinical trials, detailing their objectives, design, and escalating complexity. We present current quantitative data on success rates, duration, and participant numbers to offer a realistic perspective on drug development attrition. Furthermore, we frame this analysis within the transformative context of CRISPR-Cas9 gene editing, tracing its path from a bacterial immune system to a precision tool now navigating this very clinical pathway. The convergence of structured clinical testing and disruptive biotechnology like CRISPR heralds a new era of therapy development, demanding a thorough understanding of both the regulatory roadmap and the underlying molecular toolkit.
Clinical research represents the critical stage where laboratory discoveries are translated into human therapies. This process is systematically divided into phases, each designed to answer specific questions about a new treatment's safety, efficacy, and overall benefit-risk profile [117] [118]. The pathway is inherently high-risk, with significant attrition at each stage; understanding its structure is fundamental for researchers and drug development professionals.
This document analyzes the core pre-approval phases (I-III), which can be visualized as a sequential, gated process. The following diagram outlines the key objectives and progressive nature of this pathway.
Detailed Analysis of Clinical Trial Phases (I-III)
Each clinical trial phase serves a distinct purpose in the scientific evaluation of an investigational product. The following table summarizes the core characteristics of these phases, synthesizing data from U.S. National Institutes of Health (NIH), the Food and Drug Administration (FDA), and recent analyses [117] [119] [118].
Table 1: Core Characteristics of Clinical Trial Phases I-III
| Phase | Primary Objective | Typical Study Population Size | Approximate Duration | Key Outcomes Measured |
|---|---|---|---|---|
| Phase I | Initial safety & tolerability, pharmacokinetics/pharmacodynamics (PK/PD), identify dosage range [120] [121] [118]. | 20-100 participants [121] [118] | Several months [118] | Incidence and severity of adverse events, maximum tolerated dose (MTD) [120]. |
| Phase II | Preliminary efficacy in targeted patient population, further evaluation of safety [120] [118]. | 100-300 participants [121] | Several months to 2 years [121] [118] | Biomarker response, clinical efficacy endpoints, dose-response relationship. |
| Phase III | Confirm efficacy, monitor adverse reactions, compare to standard-of-care [120] [118]. | 300-3,000 participants [121] [118] | 1 to 4 years [121] [118] | Statistically powered primary efficacy endpoints, safety in a larger population, risk-benefit assessment. |
Phase I: First-in-Human Safety Assessment
Phase I trials represent the first administration of a new drug to humans. The primary goal is to establish a preliminary safety profile. While historically conducted in healthy volunteers, for severe diseases like cancer, Phase I trials typically enroll patients with the condition [120] [118]. These studies are often open-label and non-randomized, focusing on dose escalation to find the Maximum Tolerated Dose (MTD). A Phase I trial can take several months to complete, and approximately 70% of investigational drugs successfully proceed to Phase II [118].
Phase II: Proof-of-Concept and Dose Finding
Once initial safety is established, Phase II trials begin to assess the drug's efficacy in a specific patient population. These studies are larger and may incorporate blinding and randomization against a placebo or active control. A key objective is to refine the dosing regimen for Phase III [118]. This phase faces significant attrition, with only about 33% of drugs moving forward, often due to insufficient efficacy or emerging safety concerns [118].
Phase III: Pivotal Confirmatory Trials
Phase III trials are large, randomized, and controlled studies designed to provide definitive evidence of efficacy and a comprehensive safety profile. They are often called "pivotal" trials because their data forms the core of the submission package for regulatory approval [118]. These trials are complex, lengthy, and expensive, requiring a large and diverse patient population to generate statistically robust results. Only about 25-30% of drugs that enter Phase III successfully complete this stage and are submitted for regulatory review [118].
Quantitative Analysis of Success Rates
The drug development pipeline is characterized by high attrition. Recent dynamic analyses of clinical trial success rates (ClinSR) in the 21st century show a cumulative likelihood of approval from Phase I is approximately 5-14% [121] [122]. This low overall success rate underscores the immense challenge and risk inherent in therapeutic development.
Table 2: Attrition Rates and Cumulative Success in Clinical Development
| Development Stage | Probability of Proceeding to Next Phase | Cumulative Probability of Success (from Phase I) |
|---|---|---|
| Phase I to Phase II | ~70% [118] | 100% (Baseline) |
| Phase II to Phase III | ~33% [118] | ~70% |
| Phase III to Submission/Approval | ~25-30% [118] | ~19% - ~33% |
| Overall Approval (Phase I to Market) | N/A | ~9% - ~14% [121] [122] |
Factors influencing these rates include the therapeutic area (e.g., oncology has lower success rates than some other diseases), study design quality, patient recruitment and retention, and the fundamental mechanism of action of the drug [119] [122].
CRISPR-Cas9: A New Therapeutic Class Navigating the Clinical Pathway
The history of CRISPR-Cas9 provides a powerful case study of a disruptive technology now progressing through clinical trials. Its journey from a fundamental biological discovery to a therapeutic tool mirrors the structured progression of the clinical development pathway.
From Bacterial Immunity to Gene Editing Tool: A Historical Timeline
The development of CRISPR-Cas9 was not a single discovery but a series of key insights over decades [8] [5] [99]:
- 1987-2005: Discovery and Functional Hypothesis: Unusual repetitive sequences were first identified in E. coli in 1987 [8]. Francisco Mojica, studying these sequences in archaea and bacteria, was the first to hypothesize they were part of an adaptive immune system, coining the term CRISPR [8] [5].
- 2005-2007: Key Molecular Components: Alexander Bolotin discovered the Cas9 protein and the essential Protospacer Adjacent Motif (PAM) [5]. The role of CRISPR-Cas9 in providing adaptive immunity in Streptococcus thermophilus was experimentally demonstrated by Barrangou and Horvath [8] [5].
- 2008-2011: Mechanism Elucidation: Researchers showed that CRISPR targets DNA (not RNA) and characterized the two RNA components: crRNA and tracrRNA [8] [5]. Emmanuelle Charpentier's lab identified tracrRNA as essential for Cas9 function [8] [5].
- 2012: Engineering for Genome Editing: The teams of Virginijus Siksnys and, independently, Jennifer Doudna and Emmanuelle Charpentier, reconstituted the CRISPR-Cas9 system in vitro, demonstrating programmable DNA cleavage [5]. Doudna and Charpentier engineered a single-guide RNA (sgRNA), simplifying the system into a two-component tool [5].
- 2013 Onward: Therapeutic Applications: Feng Zhang and George Church's labs simultaneously published the first demonstrations of CRISPR-Cas9 editing in human cells, launching its use as a therapeutic modality [5].
The following diagram maps this foundational research timeline that enabled clinical applications.
The Core CRISPR-Cas9 Mechanism and Toolkit
The simplicity of the CRISPR-Cas9 system is the source of its power. As a bacterial immune system, it allows microbes to record past viral infections and cleave the DNA of invading viruses [99]. As a laboratory tool, it has been reduced to two principal components:
Table 3: Key Research Reagent Solutions for CRISPR-Cas9 Experiments
| Component | Function | Technical Application |
|---|---|---|
| Cas9 Nuclease | The effector enzyme that creates double-strand breaks (DSBs) in target DNA. Its activity is directed by the sgRNA [99]. | Wild-type Cas9 is used for gene knockout via error-prone non-homologous end joining (NHEJ) repair. |
| Single-Guide RNA (sgRNA) | A chimeric RNA molecule combining the functions of natural crRNA and tracrRNA. The 5' end is programmable to guide Cas9 to a specific DNA locus via Watson-Crick base pairing [99]. | Design of the 20-nucleotide guide sequence is critical for specificity and efficiency. It must be adjacent to a PAM sequence in the target DNA. |
| Protospacer Adjacent Motif (PAM) | A short (2-6 base pair) DNA sequence adjacent to the target site that is essential for Cas9 recognition and cleavage [8] [99]. | For the commonly used S. pyogenes Cas9, the PAM sequence is 5'-NGG-3'. This constraint influences targetable sites in the genome. |
| Donor DNA Template | An exogenous DNA molecule provided to the cell containing the desired edit, flanked by homology arms. | Used for precise gene editing via Homology-Directed Repair (HDR), allowing for gene correction or insertion. |
The mechanism can be summarized as follows: The Cas9 protein complexed with the sgRNA scans the genome. When the sgRNA finds a complementary DNA sequence adjacent to a PAM, the Cas9 enzyme undergoes a conformational change and cleaves both strands of the DNA [99]. The cell's repair mechanisms—either error-prone NHEJ or precise HDR—are then harnessed to achieve the desired genetic outcome.
CRISPR in the Clinical Arena: Protocols and Progress
CRISPR-based therapies are now actively navigating the clinical trial phases described in this document. The first approved therapy, CASGEVY (exagamglogene autotemcel), for sickle cell disease and transfusion-dependent beta thalassemia, exemplifies this journey. It involves ex vivo gene editing of a patient's own hematopoietic stem cells to reactivate fetal hemoglobin.
Detailed Experimental/Therapeutic Protocol (Ex Vivo Approach):
- Hematopoietic Stem Cell (HSC) Collection: CD34+ HSCs are collected from the patient via apheresis after mobilization [99].
- Ex Vivo Electroporation: The collected cells are transfected with the CRISPR-Cas9 components—typically a precomplexed ribonucleoprotein (RNP) of Cas9 protein and sgRNA targeting the BCL11A gene enhancer—using electroporation [99].
- Editing and Expansion: The edited cells are cultured briefly to allow the CRISPR machinery to perform the cut in the BCL11A gene, disrupting its expression. This disruption promotes fetal hemoglobin production.
- Patient Myeloablation: The patient undergoes conditioning chemotherapy (e.g., busulfan) to clear the bone marrow and make space for the engraftment of the modified cells.
- Reinfusion: The CRISPR-edited CD34+ cells are infused back into the patient.
- Engraftment and Monitoring: Patients are monitored for successful engraftment, increased fetal hemoglobin levels, and reduction of disease symptoms, alongside long-term safety follow-up for any potential off-target effects [99].
This application successfully passed through Phases I/II/III, demonstrating a favorable risk-benefit profile and leading to regulatory approval, thereby completing the journey from bacterial immunity to a commercially available human gene therapy.
The clinical development pathway for new drugs is a rigorous, phased process designed to ensure patient safety and demonstrate therapeutic efficacy. As quantitative analysis shows, this path is marked by significant attrition at each stage. The emergence of CRISPR-Cas9 as a clinical modality represents a paradigm shift in therapeutic development. Its own history—from fundamental microbiological discovery to a programmable genome engineering tool—provides a template for how deep mechanistic understanding can rapidly translate into clinical applications. For researchers and drug developers, mastering the intricacies of both the clinical trial framework and powerful new technologies like CRISPR is essential for successfully bringing the next generation of transformative medicines to patients.
The discovery of the Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) system as an adaptive immune system in bacteria and its subsequent development into a programmable genome-editing tool represents one of the most significant biological breakthroughs of the 21st century. While the Cas9 nuclease from Streptococcus pyogenes became the workhorse that launched the genome-editing revolution, the field has rapidly expanded beyond this single system. The known diversity of CRISPR–Cas systems continues to grow at an accelerated pace, with researchers discovering and characterizing novel effectors with distinct properties and functionalities [123]. This evolution from a single molecular tool to a diverse toolkit has been complemented by the development of sophisticated editing modalities that overcome fundamental limitations of early CRISPR systems.
The journey from foundational bacterial immunity research to today's advanced gene-editing technologies has been marked by key milestones. Francisco Mojica first characterized CRISPR loci in 1993, and by 2005, he and others recognized them as adaptive immune systems [5]. The critical discovery of the Cas9 protein and its associated protospacer adjacent motif (PAM) by Alexander Bolotin in 2005 laid the groundwork for understanding the mechanism [5]. Subsequent research by Emmanuelle Charpentier revealed the tracrRNA [5], while the teams of both Virginijus Siksnys and Jennifer Doudna with Emmanuelle Charpentier biochemically characterized Cas9-mediated cleavage [5]. The final pivotal step came in 2013 when Feng Zhang and George Church independently demonstrated that CRISPR-Cas9 could be harnessed for genome editing in eukaryotic cells [5].
This whitepaper provides an in-depth technical guide to the novel CRISPR systems and editing modalities that have emerged beyond the foundational Cas9, with particular focus on their mechanisms, experimental applications, and growing importance in therapeutic development.
Updated Classification and Diversity of CRISPR-Cas Systems
The classical division of CRISPR–Cas systems into two classes (Class 1 with multi-subunit effector complexes and Class 2 with single-protein effectors) and six types (I-VI) has recently been updated to encompass newly discovered variants. The current evolutionary classification now includes 2 classes, 7 types, and 46 subtypes, a significant expansion from the 6 types and 33 subtypes defined just five years ago [123]. This expanded diversity comprises the "long tail" of CRISPR–Cas distribution in prokaryotes and includes many rare variants that are just beginning to be characterized experimentally [123].
Table 1: Updated Classification of Major CRISPR-Cas Systems
| Class | Type | Signature Effector | Target | Key Features | Subtypes |
|---|---|---|---|---|---|
| Class 1 | I | Cas3 (helicase-nuclease) | DNA | Multi-subunit effector complex (Cascade) | 8 subtypes (I-A to I-H) |
| III | Cas10 (large subunit) | DNA/RNA | Involves cOA signaling; can cleave RNA collaterally | 9 subtypes (III-A to III-I) | |
| IV | DinG (helicase) | DNA | Minimal systems; function not fully characterized | 3 subtypes | |
| VII | Cas14 (metallo-β-lactamase) | RNA | Found in archaea; targets transposable elements [123] | 1 subtype | |
| Class 2 | II | Cas9 | DNA | Single effector protein; requires tracrRNA | 6 subtypes |
| V | Cas12 (including Cas12a-k) | DNA | Single effector; self-processing RNase activity | 16+ subtypes | |
| VI | Cas13 | RNA | RNA-guided RNase; collateral cleavage activity | 4+ subtypes |
Class 2 Novelty: Cas12 and Cas13 Effectors
The Class 2 CRISPR systems have seen particularly significant expansion with the characterization of numerous Cas12 and Cas13 effectors. Type V systems (Cas12) represent a diverse family of DNA-targeting enzymes with varying PAM requirements and cleavage patterns. Unlike Cas9, which typically cleaves DNA to produce blunt ends, many Cas12 effectors generate staggered ends with 5' overhangs, which can be advantageous for certain gene-editing applications [124].
Type VI systems (Cas13) represent a fundamental divergence as they exclusively target RNA rather than DNA. Cas13 effectors are RNA-guided RNases that have been leveraged for various applications including nucleic acid detection, RNA tracking, and potential therapeutic interventions at the transcript level [124]. Recent evolutionary studies using integrated sequence/structure analysis have revealed that Cas13 likely evolved from AbiF, an abortive infection-linked gene encoded within a toxin-antitoxin (TA) system with a conserved non-coding RNA (ncRNA) antitoxin [125]. The discovery of Cas13e as a miniature evolutionary intermediate between AbiF and other known Cas13s provides crucial insight into how a non-guided TA system evolved into a programmable RNA-guided CRISPR system [125].
Novel Editing Modalities: Base and Prime Editing
While novel Cas effectors expanded the targeting range of CRISPR systems, the development of base editing and prime editing represented a fundamental advancement in editing precision. These modalities address a critical limitation of traditional CRISPR nucleases: the reliance on creating double-strand breaks (DSBs) in DNA, which can lead to unpredictable repair outcomes including unwanted insertions, deletions, and chromosomal rearrangements [126] [11].
Base Editing
Base editors are fusion proteins that combine a catalytically impaired Cas nuclease (incapable of making DSBs) with a deaminase enzyme that can directly convert one DNA base to another [11]. Two main classes have been developed:
- Cytosine Base Editors (CBEs): Convert cytosine (C) to thymine (T through a C→U→T transformation [126] [11]).
- Adenine Base Editors (ABEs): Convert adenine (A) to guanine (G) through an A→I→G transformation (where I is inosine) [11].
Base editors operate without creating DSBs, significantly reducing unintended mutations compared to nuclease-based approaches [11]. However, they are limited to specific transition mutations (C-to-T or A-to-G) and can cause unwanted "bystander" edits to adjacent nucleotides within the editing window [126].
Prime Editing
Prime editing represents a more versatile "search-and-replace" technology that can introduce all types of base substitutions, small insertions, and deletions without requiring DSBs or donor DNA templates [126]. A prime editor consists of three core components:
- A Cas9 nickase (H840A) fused to an engineered reverse transcriptase (RT)
- A specialized prime editing guide RNA (pegRNA) that both specifies the target site and encodes the desired edit [126]
Table 2: Evolution of Prime Editing Systems
| Editor Version | Key Components | Editing Frequency | Innovations and Improvements |
|---|---|---|---|
| PE1 | Nickase Cas9 + M-MLV RT | ~10-20% in HEK293T cells | Initial proof-of-concept system [126] |
| PE2 | Nickase Cas9 + engineered RT | ~20-40% in HEK293T cells | Optimized RT for higher processivity and stability [126] |
| PE3 | PE2 + additional sgRNA | ~30-50% in HEK293T cells | Additional nick on non-edited strand to enhance efficiency [126] |
| PE4/PE5 | PE system + MLH1dn | ~50-80% in HEK293T cells | Inhibition of mismatch repair pathway to reduce indels [126] |
| PE6 | Modified RT + epegRNAs | ~70-90% in HEK293T cells | Compact RT variants and enhanced Cas9 variants [126] |
| vPE | Mutated Cas9 + stabilized template | 1/60th of original error rate | Dramatically reduced error rate (1 in 101 to 1 in 543 edits) [127] |
Recent advances in prime editing have focused on improving efficiency and precision. In 2025, MIT researchers reported a dramatically improved prime editor (vPE) that reduced the error rate from approximately one error in seven edits to one in 101 for the most-used editing mode through the introduction of specific Cas9 mutations that make old DNA strands less stable, facilitating their degradation and replacement with newly edited strands [127].
Experimental Protocols and Workflows
Protocol for Prime Editing in Mammalian Cells
The following detailed protocol outlines the implementation of a prime editing experiment in mammalian cells, based on established methodologies [126]:
Day 1: Cell Seeding
- Seed HEK293T or other appropriate mammalian cells in a 24-well plate at approximately 60-70% confluence in complete growth medium. Ensure cells are healthy and actively dividing.
Day 2: Transfection
- Prepare the transfection complex containing:
- Prime editor plasmid: Expressing the Cas9 nickase-reverse transcriptase fusion protein (e.g., PE2, PE3, or advanced versions)
- pegRNA plasmid: Encoding both the spacer sequence for target recognition and the RT template containing the desired edit
- (For PE3 systems) Additional sgRNA plasmid: Targeting the non-edited strand to enhance editing efficiency
- Use an appropriate transfection reagent (e.g., lipofectamine-based) according to manufacturer protocols. For difficult-to-transfect cells, consider using viral delivery systems (lentivirus, AAV) or electroporation.
- Incubate cells with transfection complex for 6-24 hours, then replace with fresh medium.
Day 3-6: Expression and Editing
- Allow cells to recover and the prime editing components to be expressed and function. The process involves:
- Target binding: The pegRNA directs the prime editor to the target genomic locus
- DNA nicking: The Cas9 nickase cleaves the PAM-containing DNA strand
- Reverse transcription: The reverse transcriptase uses the pegRNA's RT template to synthesize DNA containing the desired edit
- Flap resolution: Cellular machinery resolves the DNA structures to incorporate the edit into the genome
Day 7: Harvest and Analysis
- Harvest cells for genomic DNA extraction using standard protocols (e.g., column-based extraction)
- Amplify the target region by PCR using specific primers flanking the edit site
- Analyze editing efficiency using next-generation sequencing, restriction fragment length polymorphism (if a site is created or destroyed), or specific quantitative assays
- For clonal analysis, perform single-cell sorting and expand colonies before genotyping
Prime Editing Workflow: Diagram illustrating the molecular mechanism of prime editing, from complex formation to edit integration.
Protocol for RNA Targeting with Cas13
The following protocol outlines the implementation of Cas13 for RNA knockdown in mammalian cells, based on current methodologies [125] [124]:
Day 1: Vector Design and Preparation
- Select appropriate Cas13 ortholog (e.g., Cas13a, Cas13b, Cas13d) based on size, specificity, and PFS (protospacer flanking site) requirements
- Design crRNA with spacer sequence complementary to the target RNA transcript
- Clone the Cas13 expression vector and crRNA expression vector (or single vector combining both)
Day 2: Cell Seeding and Transfection
- Seed appropriate mammalian cells in 24-well or 12-well plates
- Transfect with Cas13 expression vector and crRNA expression vector using appropriate transfection reagent
- Include controls: non-targeting crRNA and untreated cells
Day 3-5: Incubation and Expression
- Allow 48-72 hours for Cas13 expression and RNA degradation
- Cas13 mechanism:
- Complex formation: Cas13 protein binds to the crRNA to form the effector complex
- Target binding: The complex binds complementary target RNA sequences
- Activation and cleavage: Target binding activates Cas13's RNase activity, leading to cleavage of the target RNA
- Collateral activity: (For some applications) Non-specific cleavage of surrounding RNA molecules
Day 6: Analysis
- Extract total RNA from cells using standard methods
- Analyze target RNA levels using qRT-PCR, RNA-seq, or Northern blot
- Assess potential collateral RNA cleavage effects by examining housekeeping gene levels
- For detection applications, leverage collateral activity with fluorescent reporters
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Novel CRISPR Systems
| Reagent Category | Specific Examples | Function and Application | Key Considerations |
|---|---|---|---|
| Novel Cas Effectors | Cas12a (Cpf1), Cas12b, Cas12e, Cas13a, Cas13d | DNA or RNA targeting; diverse PAM requirements; specific cleavage patterns | Size affects delivery efficiency; PAM restrictions determine targeting range |
| Base Editor Plasmids | BE4max (CBE), ABE8e (ABE) | Direct conversion of C•G to T•A or A•T to G•C without DSBs | Editing window typically 4-5 nucleotides; potential for bystander edits |
| Prime Editor Systems | PE2, PE3, PE6, vPE | Precise edits without DSBs or donor templates; all 12 possible base-to-base conversions | pegRNA design critical for efficiency; requires optimization of RT template |
| Delivery Vehicles | Lipid Nanoparticles (LNPs), AAV, Lentivirus | Efficient intracellular delivery of editing components | LNP size and composition affect tropism; viral vectors have packaging constraints |
| Guide RNA Scaffolds | pegRNAs, epegRNAs, crRNAs for Cas13 | Target recognition and (for PE) template for new genetic information | Chemical modifications enhance stability; structure affects efficiency |
| Validation Tools | NGS libraries, GUIDE-seq, targeted amplicon sequencing | Detection of on-target edits and identification of potential off-target effects | Depth of coverage critical for detecting rare edits; multiple methods recommended |
Clinical Applications and Current Trials
The translation of novel CRISPR systems from basic research to clinical applications is advancing rapidly. The first CRISPR-based medicine, Casgevy (exagamglogene autotemcel), received approval for sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT) and represents a landmark for the field [12] [128]. This therapy uses CRISPR-Cas9 to edit hematopoietic stem cells, but newer systems are poised to follow.
Novel CRISPR systems are demonstrating particular promise in several therapeutic areas:
Liver-Targeted Therapies: The natural tropism of lipid nanoparticles (LNPs) for the liver has enabled the development of in vivo CRISPR therapies for various genetic conditions. Intellia Therapeutics' Phase I trial for hereditary transthyretin amyloidosis (hATTR) using LNP-delivered CRISPR-Cas9 represents the first systemically administered CRISPR therapy, showing sustained reduction of disease-related protein levels [12]. CRISPR Therapeutics is advancing CTX310 (targeting ANGPTL3) and CTX320 (targeting LPA) for cardiovascular diseases, with updates expected in 2025 [128].
Cancer Immunotherapy: Allogeneic CAR-T cell therapies using novel gene-editing approaches are showing promising results. CRISPR Therapeutics' CTX112, a next-generation allogeneic CAR T product targeting CD19, has demonstrated strong efficacy in relapsed or refractory B-cell malignancies and is being expanded to autoimmune diseases [128].
Rare Disease and Personalized Therapies: A landmark case in 2025 demonstrated the potential for personalized in vivo CRISPR therapy, where an infant with CPS1 deficiency received a bespoke treatment developed and delivered in just six months [12]. This case sets a precedent for rapid development of customized gene-editing therapies for rare genetic disorders.
Emerging Trends and Future Directions
Artificial Intelligence in CRISPR Technology
The integration of artificial intelligence (AI) and machine learning (ML) is revolutionizing CRISPR technology development. AI-driven models are addressing key challenges including:
- gRNA design optimization: Models like DeepCRISPR, CRISPRon, and Rule Set 2 analyze large datasets to predict gRNA on-target activity and minimize off-target effects [129]
- Off-target prediction: AI algorithms can identify potential off-target sites throughout the genome by recognizing patterns in sequencing data [129]
- Protein engineering: Generative AI models are being used to design novel Cas proteins with improved properties, such as smaller size, altered PAM requirements, or enhanced specificity [129]
Delivery Technologies and Redosable Therapies
A critical advancement in CRISPR therapeutics has been the demonstration of redosable therapies using LNP delivery. Unlike viral vectors, which typically trigger immune responses that prevent redosing, LNPs have enabled multiple administrations of CRISPR therapies. Intellia Therapeutics reported that participants in their hATTR trial safely received second infusions, while the personalized CPS1 deficiency treatment involved three doses, each providing additional therapeutic benefit [12]. This represents a significant advantage for treating chronic conditions requiring sustained editing.
AI in CRISPR Development: Diagram showing how artificial intelligence is accelerating multiple aspects of CRISPR technology.
The CRISPR landscape has evolved far beyond the foundational Cas9 system, expanding to include a diverse array of novel effectors with distinct properties and increasingly sophisticated editing modalities that offer unprecedented precision. The discovery and characterization of Cas12 and Cas13 families, coupled with the development of base editing and prime editing technologies, has dramatically expanded the toolbox available to researchers and therapeutic developers.
This rapid progress is reflected in the updated classification of CRISPR-Cas systems, which now encompasses 7 types and 46 subtypes [123], and in the advancing clinical pipeline that includes not only ex vivo cell therapies but also systemically administered in vivo treatments [12] [128]. The integration of artificial intelligence into CRISPR development is accelerating the optimization of these systems [129], while advances in delivery technologies, particularly LNPs, are enabling more efficient and even redosable therapies [12].
As the field continues to mature, the convergence of novel CRISPR systems, precise editing modalities, advanced delivery technologies, and AI-driven optimization promises to unlock new therapeutic possibilities for genetic diseases, cancer, and other conditions that have previously been intractable to conventional treatments. The journey from bacterial immunity to transformative genetic medicine continues to accelerate, with novel CRISPR systems and editing modalities at the forefront of this revolution.
Conclusion
The journey of CRISPR from a fundamental biological curiosity to a clinical powerhouse represents one of the most rapid and impactful transformations in modern science. This synthesis demonstrates that while the foundational understanding of its native immune function provided the essential blueprint, the true revolution came from its re-engineering into a precise programmable tool. The successful clinical translation, marked by approved therapies and a robust pipeline, validates its therapeutic potential. However, the path forward must be navigated with careful consideration of the technical challenges—particularly genomic integrity and delivery—that remain active areas of investigation. Future directions will likely focus on enhancing specificity with next-generation editors, expanding in vivo delivery capabilities, and navigating the complex ethical and regulatory landscape. For researchers and drug developers, CRISPR is no longer a promise but a reality, poised to continue reshaping the boundaries of medicine and therapeutic intervention for years to come.
References
- 1. History of CRISPR-Cas from Encounter with a Mysterious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5847661/]
- 2. CRISPR system: Discovery, development and off-target ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656820300541]
- 3. crispr [https://en.wikipedia.org/wiki/CRISPR]
- 4. Timeline: CRISPR-Cas9 [https://www.whatisbiotechnology.org/index.php/timeline/science/CRISPR-Cas9]
- 5. CRISPR Timeline [https://www.broadinstitute.org/what-broad/areas-focus/project-spotlight/crispr-timeline]
- 6. A Brief History of CRISPR-Cas9 Genome-Editing Tools [https://bitesizebio.com/47927/history-crispr/]
- 7. CRISPR History and Development for Genome Engineering [https://www.addgene.org/crispr/history/]
- 8. CRISPR–Cas9: A History of Its Discovery and Ethical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9377665/]
- 9. CRISPR-Cas systems: prokaryotes upgrade to adaptive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4025954/]
- 10. CRISPR-Based Adaptive Immune Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3119747/]
- 11. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 12. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 13. CRISPR Acquired Resistance Against Viruses (2007) [https://embryo.asu.edu/pages/crispr-acquired-resistance-against-viruses-2007]
- 14. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 15. The tracrRNA in CRISPR biology and technologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7614092/]
- 16. characteristics of functional guide RNAs for the CRISPR/Cas9 ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-015-0784-0]
- 17. The CRISPR-Cas toolbox and gene editing technologies [https://www.sciencedirect.com/science/article/pii/S109727652101039X]
- 18. Past, present, and future of CRISPR genome editing ... [https://www.sciencedirect.com/science/article/pii/S0092867424001119]
- 19. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 20. Importance of the PAM Sequence in CRISPR Experiments [https://www.synthego.com/guide/how-to-use-crispr/pam-sequence/]
- 21. Protospacer adjacent motif [https://en.wikipedia.org/wiki/Protospacer_adjacent_motif]
- 22. A History of CRISPR [https://www.flagshippioneering.com/timelines/a-history-of-crispr]
- 23. PAM identification by CRISPR-Cas effector complexes [https://pmc.ncbi.nlm.nih.gov/articles/PMC6546366/]
- 24. Rapid characterization of CRISPR - Cas protospacer adjacent motif... 9 [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-015-0818-7]
- 25. Kinetics of the CRISPR-Cas9 effector complex assembly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4824121/]
- 26. Assessing Temperature-Dependent DNA by Cleavage - CRISPR Cas 9 [https://bio-protocol.org/en/bpdetail?id=5463&type=0]
- 27. / Crispr -mediated Cas facilitate homologous recombination... 9 cleavages [https://pmc.ncbi.nlm.nih.gov/articles/PMC9132348/]
- 28. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 29. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 30. CRISPR-detector: fast and accurate detection, visualization ... [https://www.sciencedirect.com/science/article/pii/S1673852723000747]
- 31. CRISPR-Cas Systems: Bridging Bacterial Immunity and ... [https://www.mdpi.com/2673-8007/5/4/118]
- 32. CRISPR-based technologies for the manipulation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5235943/]
- 33. Early “reduction to practice” of the CRISPR–Cas9 invention ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.1009688/full]
- 34. Federal Appeals Court Sends CRISPR-Cas9 Patent Case ... [https://vcresearch.berkeley.edu/news/federal-appeals-court-sends-crispr-cas9-patent-case-back-patent-office-reconsideration]
- 35. Harnessing bacterial immunity: CRISPR-Cas system as a ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1588446/full]
- 36. Real-space and real-time dynamics of CRISPR-Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5681550/]
- 37. Altered DNA repair pathway engagement by engineered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10242711/]
- 38. HDR vs. NHEJ: CRISPR Gene Editing Techniques [https://www.zeclinics.com/blog/hdr-vs-nhej-in-crispr-gene]
- 39. FDA Approves First Gene Therapies to Treat Patients with ... [https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease]
- 40. Casgevy [https://www.fda.gov/vaccines-blood-biologics/casgevy]
- 41. How Does CASGEVY® Work? [https://www.casgevyhcp.com/mechanism-of-action]
- 42. Vertex Announces US FDA Approval of CASGEVY ... [https://investors.vrtx.com/news-releases/news-release-details/vertex-announces-us-fda-approval-casgevytm-exagamglogene]
- 43. Casgevy (exagamglogene autotemcel) dosing, indications ... [https://reference.medscape.com/drug/casgevy-exagamglogene-autotemcel-4000387]
- 44. Understanding CRISPR Clinical Trials [https://www.synthego.com/blog/understanding-crispr-clinical-trials/]
- 45. Quarterly Industry Landscape Report | ASGCT [https://www.asgct.org/news-publications/landscape-report]
- 46. CRISPR Clinical Trials to Follow [https://www.synthego.com/blog/crispr-clinical-trials/]
- 47. Press Release - CRISPR Therapeutics [https://crisprtx.gcs-web.com/news-releases/news-release-details/crispr-therapeutics-provides-first-quarter-2025-financial]
- 48. Advancing gene editing therapeutics: Clinical trials and ... [https://www.sciencedirect.com/science/article/pii/S2162253125002203]
- 49. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-provides-business-update-and-reports-third-6]
- 50. Lipid-Nanoparticle-Based Delivery of CRISPR/Cas9 Genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9176214/]
- 51. Advancing gene editing: the role of lipid nanoparticles in ... [https://www.drugtargetreview.com/article/188056/advancing-gene-editing-the-role-of-lipid-nanoparticles-in-crispr-delivery/]
- 52. Lung and liver editing by lipid nanoparticle delivery of a ... [https://www.nature.com/articles/s41587-024-02437-3]
- 53. Brain editing now 'closer to reality': the gene-altering tools ... [https://www.nature.com/articles/d41586-025-02578-8]
- 54. AI-powered CRISPR could lead to faster gene therapies ... [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]
- 55. Infant with rare, incurable disease is first to successfully ... [https://www.nih.gov/news-events/news-releases/infant-rare-incurable-disease-first-successfully-receive-personalized-gene-therapy-treatment]
- 56. First Patient Treated with On-Demand CRISPR in Just 6 ... [https://innovativegenomics.org/news/first-patient-treated-with-on-demand-crispr-therapy/]
- 57. Severe Carbamoyl Phosphate Synthetase 1 (CPS1) ... [https://www.skpharmteco.com/news-insights/blog/rare-diseases-part-vi-severe-carbamoyl-phosphate-synthetase-1-cps1-deficiency/]
- 58. A hypomorphic model of CPS1 deficiency for investigating the ... [https://pubmed.ncbi.nlm.nih.gov/40421838/]
- 59. Ethical considerations of gene editing and genetic selection [https://pmc.ncbi.nlm.nih.gov/articles/PMC7260159/]
- 60. of History -Cas from Encounter with a Mysterious Repeated... CRISPR [https://pubmed.ncbi.nlm.nih.gov/29358495/]
- 61. CRISPR/Cas9 for the treatment of haematological diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC8118330/]
- 62. Overview CRISPR Clinical Trials 2025 - Learn | Innovate [https://crisprmedicinenews.com/clinical-trials/]
- 63. Comprehensive review of CRISPR-based gene editing [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01925-5]
- 64. Spatial CRISPR genomics identifies regulators of the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8992964/]
- 65. A quantitative systems pharmacology (QSP) platform for preclinical to... [https://pubmed.ncbi.nlm.nih.gov/39372210/]
- 66. Frontiers | A quantitative systems pharmacology (QSP) platform for... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1454785/full]
- 67. Off-target effects in CRISPR-Cas genome editing for ... [https://pubmed.ncbi.nlm.nih.gov/40777742/]
- 68. Off-target effects in CRISPR/Cas9 gene editing [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1143157/full]
- 69. Annotation and Classification of CRISPR-Cas Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5901762/]
- 70. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 71. Navigating the Hidden Risks of CRISPR with the ... - KROMATID [https://kromatid.com/blog/navigating-the-hidden-risks-of-crispr-with-the-kromasure-platform]
- 72. Recent Updates of the CRISPR/Cas9 Genome Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11164216/]
- 73. Comprehensive protocols for CRISPR/Cas9-based gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988528/]
- 74. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 75. This Way: Choosing Between CRISPR System | VectorBuilder Delivery [https://en.vectorbuilder.com/resources/vector-academy/lessons/crispr-delivery-systems.html]
- 76. medicine for blood disorders: Progress and challenges in... CRISPR [https://pmc.ncbi.nlm.nih.gov/articles/PMC9853164/]
- 77. innovations and challenges in rAAV vector-based CRISPR ... [https://www.nature.com/articles/s41434-025-00573-2]
- 78. Peeling back the layers of immunogenicity in Cas9-based ... [https://www.sciencedirect.com/science/article/pii/S1525001625005350]
- 79. CRISPR-Cas9-mediated homology-directed repair for ... [https://www.sciencedirect.com/science/article/pii/S2162253124002312]
- 80. Comparative analysis of multiple DNA double-strand break ... [https://www.nature.com/articles/s42003-025-08187-5]
- 81. The hidden risks of CRISPR/Cas: structural variations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325979/]
- 82. CRISPR Therapeutics Provides First Quarter 2025… [https://crisprtx.com/about-us/press-releases-and-presentations/crispr-therapeutics-provides-first-quarter-2025-financial-results-and-announces-positive-top-line-data-from-phase-1-clinical-trial-of-ctx310-targeting-angptl3]
- 83. Origins of CRISPR: How it Came to Be [https://www.bioagilytix.com/blog/origins-of-crispr-how-it-came-to-be/]
- 84. CRISPR–Cas9 Gene Editing: Curing Genetic Diseases by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10980556/]
- 85. Bioethical issues in genome editing by CRISPR-Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7129066/]
- 86. Gene Editing [https://crisprtx.com/gene-editing]
- 87. Clinical applications of the CRISPR/Cas9 genome-editing ... [https://www.sciencedirect.com/science/article/pii/S235230422300079X]
- 88. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 89. CRISPR-Cas9 and Its Bioinformatics Tools: A Systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109910/]
- 90. Informed Consent for Human Embryo Genome Editing [https://www.sciencedirect.com/science/article/pii/S2213671120301004]
- 91. What is CRISPR? A bioengineer explains - Stanford Report [https://news.stanford.edu/stories/2024/06/stanford-explainer-crispr-gene-editing-and-beyond]
- 92. Transthyretin Cardiac Amyloidosis: Current and Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11754378/]
- 93. Molecular mechanisms and emerging therapies in wild ... [https://link.springer.com/article/10.1007/s10741-023-10380-9]
- 94. a systematic review and meta-analysis of randomized trials [https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-025-04653-4]
- 95. AL amyloidosis: from molecular mechanisms to targeted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6142527/]
- 96. Mass spectrometry based targeted protein quantification [https://pmc.ncbi.nlm.nih.gov/articles/PMC2657955/]
- 97. IHC Analysis vs. Mass Spectrometry for Clinical Protein ... [https://sapient.bio/resources/ihc-analysis-vs-mass-spectrometry/]
- 98. Immunohistochemistry and mass spectrometry for highly ... [https://www.sciencedirect.com/science/article/pii/S0023683722022851]
- 99. CRISPR-Cas9: A fascinating journey from bacterial ... [https://www.sciencedirect.com/science/article/abs/pii/S1877117321000016]
- 100. ZFN, TALEN and CRISPR/Cas-based methods for genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3694601/]
- 101. Genome-Editing Technologies: Concept, Pros, and Cons of ... [https://www.sciencedirect.com/science/article/pii/S2162253119300587]
- 102. Expanding the genetic editing tool kit: ZFNs, TALENs, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4191047/]
- 103. CRISPR-Cas9, TALENs and ZFNs - the battle in gene editing [https://www.ptglab.com/news/blog/crispr-cas9-talens-and-zfns-the-battle-in-gene-editing/?srsltid=AfmBOoqzK2nAhteCc9n9yjsK7Q1w-qLziku0ghJ1Pix_Ap92nIgT3_lv]
- 104. Exploring CRISPR-Cas: The transformative impact of gene ... [https://pubmed.ncbi.nlm.nih.gov/41069986/]
- 105. Comparing Gene Editing Platforms: CRISPR vs. Traditional ... [https://blog.crownbio.com/comparing-gene-editing-platforms-crispr-vs-traditional-methods]
- 106. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-present-preclinical-data-alpha-1-antitrypsin]
- 107. ICH S2 (R1) Genotoxicity testing and data interpretation for ... [https://www.ema.europa.eu/en/ich-s2-r1-genotoxicity-testing-data-interpretation-pharmaceuticals-intended-human-use-scientific-guideline]
- 108. S2(R1) Genotoxicity Testing and Data Interpretation for ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/s2r1-genotoxicity-testing-and-data-interpretation-pharmaceuticals-intended-human-use]
- 109. FDA officials offer roadmap for gene-editing cases like Baby KJ's [https://www.statnews.com/2025/11/12/fda-roadmap-how-to-scale-baby-kj-custom-gene-editing-treatment/]
- 110. FDA unveils new regulatory roadmap for bespoke drug ... [https://www.biopharmadive.com/news/fda-plausible-mechanism-pathway-n-of-1-crispr/805235/]
- 111. Implementing Alternative Methods [https://www.fda.gov/science-research/advancing-alternative-methods-fda/implementing-alternative-methods]
- 112. Genotoxicity: OECD guidelines & future of genetic safety ... [https://genevolution.fr/2025/07/01/from-oecd-guidelines-to-innovation-future-genotoxicity-testing/]
- 113. Genome Editing Market to Grow at 16.9% CAGR [https://www.bccresearch.com/pressroom/bio/genome-editing-market-to-grow-at-169-cagr?srsltid=AfmBOorD0ttw9v89ZvCefPXp3JqFfWvhynC4sp68yEmOMZOCEtCbDLKA]
- 114. Genome Editing: Technologies and Global Markets [https://www.bccresearch.com/market-research/biotechnology/genome-editing.html?srsltid=AfmBOopMkWQf7TkZ4dOoFrUIjkXJ_zXrWYsxkq0dou9JnUKcp1jY6K2b]
- 115. Gene Editing Market Size and Share | Industry Statistics [https://www.gminsights.com/industry-analysis/gene-editing-market]
- 116. Genome Editing Market Forecast Report 2025-2030, with ... [https://finance.yahoo.com/news/genome-editing-market-forecast-report-131200315.html]
- 117. The Basics | National Institutes of Health (NIH) [https://www.nih.gov/health-information/nih-clinical-research-trials-you/basics]
- 118. Step 3: Clinical Research [https://www.fda.gov/patients/drug-development-process/step-3-clinical-research]
- 119. Dynamic clinical trial success rates for drugs in the 21st ... [https://www.nature.com/articles/s41467-025-64552-2]
- 120. Phases of Clinical Trials [https://www.mdanderson.org/patients-family/diagnosis-treatment/clinical-trials/phases-of-clinical-trials.html]
- 121. Clinical Trial Phases Explained: All 4 Stages (2025) [https://collectiveminds.health/articles/clinical-trial-phases-complete-guide-to-all-4-stages]
- 122. The Roadmap to Clinical Trials Success (2024-2025) [https://www.linkedin.com/pulse/roadmap-clinical-trials-success-2024-2025-data-driven-alex-benjamin-h8wue]
- 123. An updated evolutionary classification of CRISPR–Cas ... [https://www.nature.com/articles/s41564-025-02180-8]
- 124. Exploring CRISPR-Cas: The transformative impact of gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506487/]
- 125. Reprogrammable RNA-targeting CRISPR systems evolved ... [https://www.sciencedirect.com/science/article/pii/S0092867425001035]
- 126. Emerging trends in prime editing for precision genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322275/]
- 127. A more precise way to edit the genome [https://news.mit.edu/2025/more-precise-way-edit-genome-0917]
- 128. CRISPR Therapeutics Highlights Strategic Priorities and ... [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-highlights-strategic-priorities-and]
- 129. Revolutionizing CRISPR technology with artificial intelligence [https://www.nature.com/articles/s12276-025-01462-9]