Decoding Antimicrobial Resistance: A Comprehensive Guide to Metagenomic NGS Analysis
The escalating global health crisis of antimicrobial resistance (AMR) demands advanced surveillance tools.
Decoding Antimicrobial Resistance: A Comprehensive Guide to Metagenomic NGS Analysis
Abstract
The escalating global health crisis of antimicrobial resistance (AMR) demands advanced surveillance tools. Metagenomic Next-Generation Sequencing (mNGS) offers a powerful, culture-independent approach for comprehensively profiling antibiotic resistance genes (ARGs) within complex microbial communities, from clinical to environmental samples. This article provides a foundational understanding of mNGS for AMR analysis, explores diverse methodological workflows and their real-world applications, addresses key technical challenges and optimization strategies, and critically evaluates the technology's performance against traditional diagnostic methods. Aimed at researchers, scientists, and drug development professionals, this review synthesizes current advancements and practical insights, empowering the scientific community to harness mNGS for precise AMR monitoring and the development of targeted countermeasures.
The mNGS Revolution in AMR Surveillance: Principles and Promise
Metagenomic Next-Generation Sequencing (mNGS) represents a transformative approach in clinical microbiology, enabling hypothesis-free detection of pathogens directly from clinical specimens. Unlike traditional culture and targeted molecular assays, mNGS can simultaneously identify bacteria, viruses, fungi, and parasites without prior knowledge of the causative agent [1]. This "unbiased" detection capability is particularly valuable for diagnosing polymicrobial infections, fastidious organisms, and cases where conventional methods fail [1] [2].
The fundamental principle of mNGS involves comprehensive sequencing of all nucleic acids (DNA and/or RNA) in a clinical sample, followed by bioinformatic analysis to classify sequences against microbial reference databases [2]. This culture-independent approach bypasses the limitations of traditional methods that require specific growth conditions or targeted primer designs. A key advantage of mNGS lies in its dual capability to not only identify pathogens but also detect antimicrobial resistance (AMR) genes, providing critical information for treatment decisions [3] [4]. However, it is important to recognize that mNGS workflows are subject to various sources of bias introduced during sample preparation, library construction, and bioinformatic analysis, all of which can affect sensitivity and taxonomic resolution [1].
Diagnostic Performance and Comparative Analysis
Multiple clinical studies have demonstrated the superior sensitivity of mNGS compared to conventional methods across various infection types. In central nervous system infections, mNGS has demonstrated diagnostic yields as high as 63%, compared to less than 30% for conventional approaches [1]. For lower respiratory tract infections, mNGS detected bacteria in 71.7% of cases, significantly higher than culture (48.3%) [5].
Table 1: Comparative Diagnostic Performance of mNGS Across Infection Types
| Infection Type | Sensitivity (%) | Specificity (%) | Comparative Method | Clinical Context |
|---|---|---|---|---|
| Periprosthetic Joint Infection | 89 | 92 | Culture | Meta-analysis of 23 studies [6] |
| Pediatric Severe Pneumonia | 96.6 | 51.6 | Culture | Bronchoalveolar lavage fluid [5] |
| Central Nervous System Infections | ~63 | ~90 | Conventional methods | Diagnostically challenging cases [1] |
| Culture-negative PJI | Significantly higher | ~60 | Culture | Detects additional rare pathogens [2] |
For periprosthetic joint infection (PJI), a systematic review and meta-analysis demonstrated that mNGS exhibits higher sensitivity than targeted NGS (tNGS) while maintaining adequate specificity, confirming its clinical value for infection detection [6]. The pooled sensitivity and specificity for diagnosing PJI were 0.89 and 0.92 for mNGS, compared to 0.84 and 0.97 for tNGS [6].
In respiratory infections, mNGS has proven particularly valuable for immunocompromised patients and those with complex clinical presentations. One study on lower respiratory tract infections established that the logarithm of reads per kilobase per million mapped reads [lg(RPKM)] showed the best performance for identifying true-positive pathogenic bacteria, with an area under the curve (AUC) of 0.99 and an optimal lg(RPKM) threshold of -1.35 [7].
Antimicrobial Resistance Detection Capabilities
The ability to predict antimicrobial resistance simultaneously with pathogen detection represents one of the most significant advantages of mNGS technology. By identifying resistance genes and mutations in clinical samples, mNGS provides early insights into antimicrobial susceptibility patterns before traditional phenotypic results are available [3] [4].
Table 2: Performance of mNGS for Antimicrobial Resistance Prediction
| Pathogen | Antibiotic Class | Sensitivity (%) | Specificity (%) | Study Context |
|---|---|---|---|---|
| Various bacteria | Carbapenems | 67.74 | 85.71 | Pediatric severe pneumonia [5] |
| Various bacteria | Penicillins | 28.57 | 75.00 | Pediatric severe pneumonia [5] |
| Various bacteria | Cephalosporins | 46.15 | 75.00 | Pediatric severe pneumonia [5] |
| Acinetobacter baumannii | Carbapenems | 94.74 | N/R | Clinical isolates [5] |
| Acinetobacter baumannii | β-lactams | >80 | N/R | 53 clinical samples [4] |
| Acinetobacter baumannii | Aminoglycosides | >80 | N/R | 53 clinical samples [4] |
The detection performance varies significantly among different pathogens and antibiotics. For instance, mNGS shows higher sensitivity for predicting carbapenem resistance compared to penicillins and cephalosporins [5]. In Acinetobacter baumannii, mNGS demonstrated excellent performance for detecting resistance to β-lactams, aminoglycosides, quinolones, and minocycline, with class-specific accuracy exceeding 80% [4].
Recent advances in bioinformatic tools have enhanced AMR detection capabilities. The Chan Zuckerberg ID (CZ ID) AMR module represents an open-access, cloud-based workflow designed to integrate detection of both microbes and AMR genes in mNGS and single-isolate whole-genome sequencing data [3]. This tool leverages the Comprehensive Antibiotic Resistance Database (CARD) and associated Resistance Gene Identifier software, enabling broad detection of both microbes and AMR genes from Illumina data [3].
Detailed Experimental Protocols
Sample Processing and Nucleic Acid Extraction
The standard workflow for mNGS begins with sample collection, typically from sterile sites (CSF, blood, tissue) or non-sterile sites (BALF, sputum) with different contamination control measures [1] [7]. For bronchoalveolar lavage fluid samples, the protocol involves:
- Sample Preparation: Centrifuge 1 mL of BALF at 12,000 × g for 5 minutes to collect microorganisms and human cells [5].
- Host DNA Depletion: Resuspend the precipitate in 50 μL and treat with Benzonase (1 U) and 0.5% Tween 20, followed by incubation at 37°C for 5 minutes [5]. This critical step improves microbial signal by reducing host nucleic acid contamination.
- Nucleic Acid Extraction: Transfer 600 μL of the mixture to tubes containing ceramic beads for bead beating using a homogenizer. Extract nucleic acid from 400 μL of pretreated samples using a commercial pathogen DNA kit, eluting in 60 μL of elution buffer [5].
- RNA Processing: For RNA extraction, use a viral RNA kit followed by removal of ribosomal RNA. Synthesize cDNA using reverse transcriptase and dNTPs [5].
For plasma samples, collect 3 mL of peripheral blood, process within 8 hours with centrifugation at 4,000 rpm for 10 minutes at 4°C [4]. The plasma is then transferred to sterile tubes for processing.
Library Preparation and Sequencing
Library preparation follows standardized protocols with some variations between platforms:
- Library Construction: Use library construction kits according to manufacturer's instructions. For Illumina platforms, DNA/cDNA libraries are constructed using the KAPA low throughput library construction kit [5].
- Enrichment: For targeted approaches, aliquot 750 ng of library from each sample for hybrid capture-based enrichment of microbial probes through one round of hybridization [5].
- Quality Control: Assess library quality using the Qubit dsDNA HS Assay kit followed by the High Sensitivity DNA kit on an Agilent 2100 Bioanalyzer [5].
- Sequencing: Load library pools onto sequencers (e.g., Illumina Nextseq CN500) for 75 cycles of single-end sequencing, generating approximately 20 million reads for each library [5].
For BGI platforms, the process includes enzymatic digestion, end repair, adapter ligation, and PCR amplification to generate sequencing libraries. Verify fragment sizes (approximately 300 bp) using an Agilent 2100 Bioanalyzer and determine library concentrations using the Qubit dsDNA HS Assay Kit [4].
Bioinformatic Analysis Pipeline
The computational analysis of mNGS data involves multiple steps to distinguish true pathogens from background noise and contaminants:
- Quality Control and Preprocessing: Raw sequencing reads undergo deduplication, trimming, and quality filtering using tools like fastp [5] [4].
- Host Read Removal: Map reads to the human genome (GRCh38) using alignment software such as Bowtie2 or BWA, then remove matching sequences [5] [3] [4].
- Taxonomic Classification: Classify remaining reads using tools like Centrifuge against comprehensive microbial databases containing bacterial, viral, fungal, and parasitic reference genomes [5].
- AMR Gene Detection: Two parallel approaches are commonly used:
- Pathogen-of-Origin Prediction: Use k-mer-based approaches to link AMR genes to specific pathogen species and predict chromosomal versus plasmid location [3].
The CZ ID platform automates this workflow in a cloud-based environment, making analysis accessible to researchers with limited bioinformatics expertise [3]. A sample with 50 million reads typically takes less than 5 hours to process after upload [3].
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for mNGS Workflow
| Category | Specific Product/Kit | Function/Application | Key Features |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp UCP Pathogen Mini Kit | Pathogen DNA extraction from clinical samples | Effective for low-biomass samples [5] |
| Nucleic Acid Extraction | QIAamp Viral RNA Kit | RNA extraction for viral detection | Maintains RNA integrity [5] |
| Host Depletion | Benzonase + Tween 20 | Host nucleic acid degradation | Critical for improving microbial signal [5] |
| Library Preparation | KAPA low throughput library construction kit | Library construction for Illumina platforms | Optimized for low-input samples [5] |
| Target Enrichment | SeqCap EZ Library (Roche) | Hybrid capture-based enrichment | Improves sensitivity for targeted pathogens [5] |
| rRNA Depletion | Ribo-Zero rRNA Removal Kit | Ribosomal RNA removal for RNA sequencing | Enhances non-rRNA transcript detection [5] |
| Quality Control | Qubit dsDNA HS Assay Kit | DNA quantification | Accurate measurement of low-concentration samples [5] [4] |
| Quality Control | Agilent 2100 Bioanalyzer | Fragment size analysis | Quality assessment of libraries [5] [4] |
| Database | Comprehensive Antibiotic Resistance Database (CARD) | AMR gene reference | Curated resistance gene information [3] |
| Analysis Tool | Resistance Gene Identifier (RGI) | AMR gene detection | Matches sequences to CARD database [3] |
Implementation Challenges and Future Directions
Despite its promising capabilities, mNGS implementation faces several technical and operational challenges. Sample processing workflows often require host DNA depletion to improve microbial signal in low-biomass specimens, and bioinformatic pipelines must be standardized to ensure reproducibility [1]. The high abundance of host-derived nucleic acids remains a significant barrier, particularly in blood and tissue samples [1].
Regulatory frameworks are beginning to accommodate metagenomic assays, but validation procedures and reimbursement models remain inconsistent and underdeveloped [1]. Ethical considerations, including incidental findings, patient privacy, and disparities in access, must be addressed to ensure equitable implementation [1].
Future directions involve artificial intelligence and machine learning to automate taxonomic classification, AMR gene detection, and clinical reporting, reducing turnaround times and improving interpretability [1]. Emerging approaches such as host transcriptome profiling and single-cell RNA sequencing are showing promise in differentiating bacterial versus viral infections and predicting disease severity [1]. Combining host immune signatures with microbial sequencing data may enable real-time, precision-guided infectious disease management [1].
Ultra-portable sequencing technologies capable of generating results within hours are being evaluated for use in emergency departments, border surveillance, and field hospitals [1]. These advancements, coupled with open-access platforms like CZ ID that democratize pathogen genomic analysis, represent important steps toward collaborative efforts to combat the growing threat of antimicrobial resistance [3].
Application Note: Overcoming the Limitations of Traditional Antimicrobial Resistance Detection
The pervasive threat of Antimicrobial Resistance (AMR) necessitates a paradigm shift in surveillance and diagnostic strategies. Traditional, culture-based methods are fundamentally limited by their inability to capture the vast majority of environmental microbes, their predisposition toward known pathogens, and their narrow scope [8] [9]. This application note details how metagenomic next-generation sequencing (mNGS) addresses these critical gaps through its three core advantages: culture-independence, hypothesis-free discovery, and comprehensive analysis of the resistome. By providing a direct, unbiased view of the genetic material in any sample, mNGS is transforming our ability to monitor and understand AMR dynamics across human, animal, and environmental ecosystems [10].
Quantitative Advantages of mNGS over Traditional AST
The table below summarizes the performance of mNGS against traditional antimicrobial susceptibility testing (AST) methods across key parameters.
Table 1: A comparative analysis of metagenomic NGS and traditional methods for AMR profiling.
| Feature | Metagenomic NGS (mNGS) | Traditional Culture & AST |
|---|---|---|
| Dependency on Culture | Culture-independent; analyzes genetic material directly from samples [1] | Mandatory; requires isolation and growth of pathogens [9] |
| Discovery Capability | Hypothesis-free; detects novel, unexpected, and co-infecting pathogens and ARGs [11] [1] | Targeted; only identifies pre-selected, cultivable organisms [8] |
| Scope of Analysis | Comprehensive; profiles all ARGs, virulence factors, and mobile genetic elements in the "resistome" [8] [10] | Narrow; typically profiles resistance in a single, isolated pathogen [9] |
| Turnaround Time | ~5-9 hours for pathogen ID and first AMR gene detection with rapid protocols [12] | 16-20 hours for MIC results alone, plus additional time for culture [13] [14] |
| Throughput | High-throughput; capable of processing and sequencing multiple samples in parallel [9] | Low-throughput; intensive manual labor for each isolate [15] |
| Key Limitation | High computational complexity and cost; challenges in genotype-phenotype correlation [11] [14] | Fails for non-culturable, fastidious, or slow-growing organisms [1] [9] |
Protocol: A Detailed Workflow for mNGS-Based Resistome Analysis
This protocol outlines a robust methodology for shotgun metagenomic sequencing to characterize the antibiotic resistome in complex samples, such as clinical specimens or environmental samples. The workflow incorporates best practices for host DNA depletion to ensure sufficient microbial sequencing coverage.
Step-by-Step Experimental Procedure
Sample Collection and Pre-processing
- Sample Types: Collect samples (e.g., fecal matter, water, soil, milk) in sterile containers [10]. Transport immediately in a cold chain (2-8°C) to the laboratory [10].
- Critical Pre-processing for High-Host-DNA Samples: For samples like milk or blood that contain abundant host DNA, a dedicated host DNA depletion step is crucial.
- Method: Use a combination of a commercial host depletion kit (e.g., MolYsis Complete5), 10% bile extract (Ox bile), and micrococcal nuclease treatment [12].
- Rationale: This combination has been shown to effectively enrich bacterial DNA, reducing bovine DNA reads to an average of 17% while increasing pathogen (Staphylococcus aureus) reads to 66.5% [12].
DNA Extraction and Library Preparation
- DNA Extraction: Perform extraction using kits validated for complex samples, such as the QIAamp Fast DNA Stool Mini Kit for fecal samples or the PowerSoil DNA Isolation Kit for environmental samples [10]. Assess DNA concentration and integrity using a fluorometer and agarose gel electrophoresis [10].
- Library Preparation: Use ~1 ng of genomic DNA with a high-throughput library preparation kit (e.g., Illumina Nextera XT DNA Library Preparation Kit). Clean up the libraries using AMPure XP beads [10].
Sequencing and Real-Time Analysis
- Platform Selection: For real-time analysis, use a long-read sequencer like the Oxford Nanopore Technologies (ONT) MinION. For high-accuracy short-read data, use an Illumina platform [1] [9].
- Sequencing Execution: Pool normalized libraries and load onto the sequencer. For rapid results, even a 40-minute MinION run can be sufficient for initial bacterial identification and detection of the first AMR genes [12].
Bioinformatic Analysis Pipeline
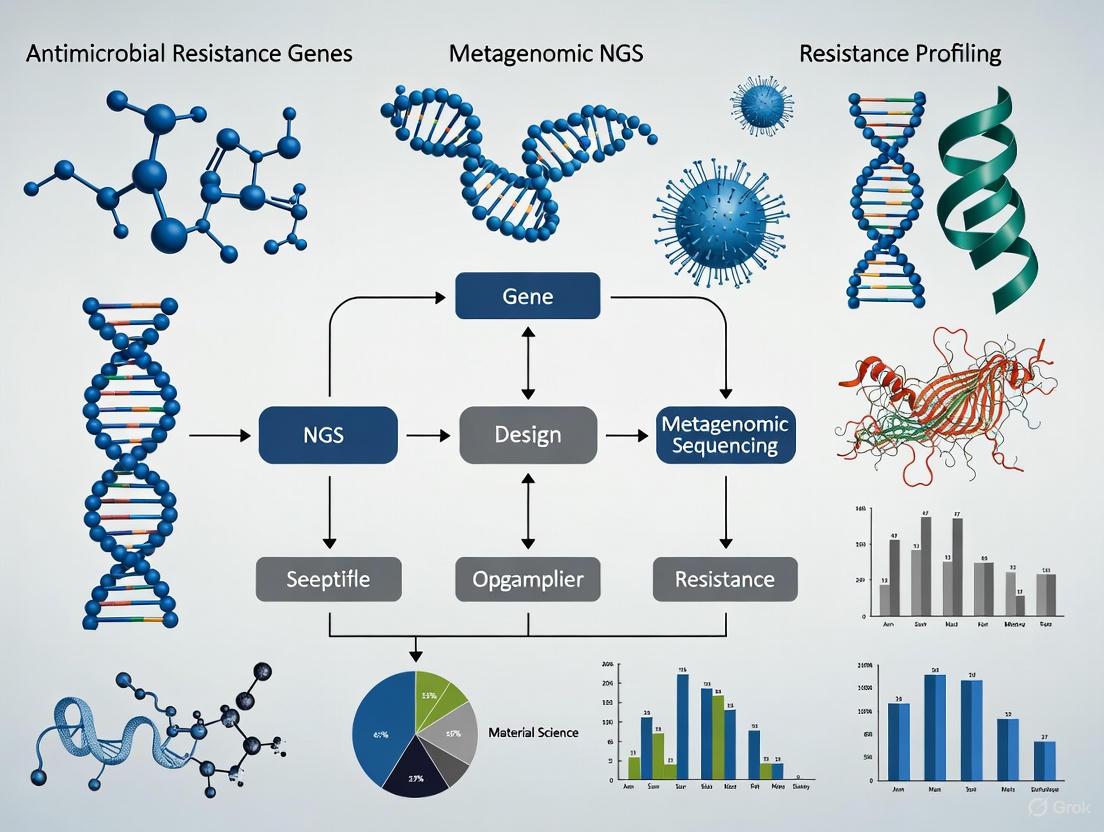
The following diagram illustrates the core bioinformatic workflow for processing mNGS data to profile AMR.
Diagram 1: Bioinformatic workflow for mNGS-based AMR analysis.
- Quality Control: Process raw sequences (e.g., using FASTP) to eliminate low-quality reads and adapters [16].
- Taxonomic Profiling: Use tools like MetaPhlAn to classify the microbial community composition against databases of clade-specific marker genes [10].
- Metagenome Assembly: De novo assemble quality-filtered reads into contigs using assemblers like MEGAHIT [16].
- ARG and MGE Annotation: Predict open reading frames (ORFs) from contigs (e.g., with Prodigal). Annotate these ORFs against curated ARG databases (e.g., deepARG) and MGE databases using BLAST-based tools (e.g., DIAMOND) with strict E-value cut-offs (e.g., ≤ 1e-5) [16] [8].
- Advanced Analysis: For higher-resolution analysis, perform metagenomic binning (e.g., with MetaWRAP) to generate metagenome-assembled genomes (MAGs). This allows for the direct linkage of ARGs with specific bacterial hosts and their pathogenic potential [16].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key reagents, kits, and databases essential for conducting mNGS-based AMR studies.
| Item Name | Function/Application | Specific Example(s) |
|---|---|---|
| Host DNA Depletion Kit | Selectively degrades host DNA to enrich for microbial sequences in high-host-content samples. | MolYsis Complete5, MolYsis Plus [12] |
| DNA Extraction Kits | Isolation of high-quality microbial DNA from complex matrices (stool, soil, water). | QIAamp Fast DNA Stool Mini Kit, PowerSoil DNA Isolation Kit, DNeasy PowerFood Microbial Kit [16] [10] |
| Library Prep Kits | Preparation of sequencing-ready libraries from extracted DNA. | Illumina Nextera XT DNA Library Preparation Kit [10] |
| Sequencing Platforms | High-throughput sequencing of prepared libraries. | Illumina MiSeq/HiSeq (short-read), Oxford Nanopore MinION (long-read) [16] [12] |
| ARG Reference Database | Curated collection of sequences for annotating and identifying antibiotic resistance genes. | deepARG, METABOLIC, VB12Path (for specific metabolic traits) [16] [8] |
| Bioinformatics Tools | Software and pipelines for data QC, assembly, taxonomic profiling, and functional annotation. | FASTP, MEGAHIT, MetaPhlAn, Prodigal, DIAMOND, MetaWRAP [16] [10] |
Integrated Data Analysis and Visualization
The power of mNGS is fully realized in the integration of different data layers. As demonstrated in a study of urban lakes, binning analysis can reconstruct Metagenome-Assembled Genomes (MAGs) that actively participate in specific metabolic processes (like vitamin B12 synthesis) while also carrying ARGs and demonstrating pathogenicity [16]. This level of integration provides unprecedented insight into the hosts and co-factors of resistance dissemination.
From Data to Actionable Insights
The final stage involves synthesizing the analyzed data into a coherent report that includes:
- The Resistome Profile: A list of detected ARGs and their abundances.
- Pathogen Identification: A list of detected pathogenic bacteria, viruses, and fungi.
- Mobility Assessment: Identification of MGEs (plasmids, integrons, transposons) co-located with ARGs, indicating horizontal transfer potential [8].
- Risk Evaluation: Tools like MetaCompare can be employed to estimate resistome risk by evaluating the coexistence of ARGs, MGEs, and human pathogens [16].
Resistome Profiling, Horizontal Gene Transfer, and Mobile Genetic Elements
Resistome profiling refers to the comprehensive analysis of all antibiotic resistance genes (ARGs) within a microbial community (the 'resistome') [17]. This approach leverages metagenomic next-generation sequencing (mNGS) to detect and characterize ARGs directly from clinical or environmental samples, bypassing the need for culturing and enabling the surveillance of resistant pathogens and the discovery of novel resistance mechanisms [10] [1]. A critical force shaping the resistome is horizontal gene transfer (HGT), which allows the rapid sharing of genetic material between bacteria, including ARGs [10]. This process is primarily facilitated by mobile genetic elements (MGEs), such as plasmids, transposons, and integrons, which act as vectors for the acquisition and dissemination of resistance traits among bacterial populations [18] [19]. The interplay between these concepts is fundamental to understanding the evolution and spread of antimicrobial resistance (AMR), a major global health threat causing millions of deaths annually [1].
Table 1: Key Concepts in AMR Research
| Concept | Description | Role in AMR |
|---|---|---|
| Resistome | The full collection of antibiotic resistance genes in a microbial community [17]. | Defines the potential for resistance in a given environment or sample. |
| Horizontal Gene Transfer (HGT) | The movement of genetic material between bacteria that are not in a parent-offspring relationship [10]. | Enables rapid acquisition and spread of ARGs across bacterial populations and species. |
| Mobile Genetic Elements (MGEs) | DNA sequences that can move within or between DNA molecules and cells [18] [19]. | Acts as a vehicle for ARGs during HGT, driving the evolution of multidrug-resistant pathogens. |
Experimental Protocols for Resistome Analysis
This section details standard and emerging wet-lab and computational protocols for resistome profiling, from sample preparation to data analysis.
Sample Processing and Metagenomic Sequencing
The initial phase involves extracting total DNA from diverse samples to prepare sequencing libraries.
Protocol: Metagenomic DNA Sequencing for Resistome Profiling
- Sample Collection: The protocol begins with the collection of samples from targeted environments. For instance, studies have analyzed human and animal fecal samples, soil, drinking water, and riverbed sediments [10]. Samples should be immediately transported on ice or preserved using reagents like RNAlater.
- DNA Extraction: Total genomic DNA is extracted using commercial kits. For fecal samples, the QIAamp Fast DNA Stool Mini Kit is commonly used, while environmental samples like soil may require the PowerSoil DNA Isolation Kit [10]. DNA concentration and integrity are quantified using a fluorometer (e.g., Qubit) and agarose gel electrophoresis.
- Library Preparation and Sequencing: Following extraction, 1 ng of genomic DNA is used as input for library preparation with kits such as the Illumina MiSeq Nextera XT DNA Library Preparation Kit [10]. The constructed libraries are then sequenced on platforms like the Illumina MiSeq to generate paired-end reads (e.g., 2x151 bp). For applications requiring long reads or point-of-care testing, portable Oxford Nanopore Technologies (ONT) sequencers like the MinION can be deployed [1].
Targeted Enrichment for Cost-Effective Resistome Profiling
While shotgun metagenomics is powerful, targeted enrichment can be a more cost-effective strategy for deepening the sequencing of specific genes.
Protocol: Targeted Resistome Profiling using CARPDM-Generated Probe Sets
- Principle: This method uses hybridization probes to enrich metagenomic DNA for ARG sequences prior to sequencing, significantly increasing the number of reads mapping to resistance genes and lowering detection limits [20].
- Probe Set Design: The Comprehensive Antibiotic Resistance Probe Design Machine (CARPDM) software is used to generate open-source, up-to-date hybridization probe sets from the Comprehensive Antibiotic Resistance Database (CARD) [20]. Two example sets are:
- allCARD: Targets all genes in CARD's protein homolog models (n=4,661).
- clinicalCARD: Focuses on a clinically relevant subset of genes (n=323).
- In-House Probe Synthesis: A key feature of this protocol is a method for in-house synthesis of probe sets, which can save up to $350 per reaction, making the technique more accessible [20].
- Enrichment and Sequencing: The synthesized probes are used in a bait-capture hybridization with the metagenomic DNA. The enriched DNA is then sequenced, with demonstrated increases in resistance-gene mapping reads of up to 594-fold for allCARD and 598-fold for clinicalCARD [20].
Targeted Resistome Profiling Workflow
Bioinformatic Analysis for Resistome Characterization
After sequencing, raw data is processed to identify and quantify ARGs and their genetic contexts.
Protocol: Computational Resistome Analysis from mNGS Data
- Gene Prediction: For assembled metagenomic contigs or whole genomes, gene prediction is performed using tools like Prodigal (v2.6.3) with the 'meta' option specified [21].
- ARG Annotation: Predicted genes are compared against specialized ARG databases using BLASTp. Standard parameters include:
- Clustering and Abundance Calculation: To resolve redundancy, ARGs can be clustered into families using algorithms like the Markov Cluster (MCL) algorithm [21]. The relative abundance of ARGs is calculated as the number of ARGs divided by the total number of predicted genes in the sample [21].
- High-Resolution Profiling with GROOT: For unassembled sequencing reads, tools like GROOT (Graphing Resistance Out Of meTagenomes) offer a fast and accurate alternative. GROOT uses a variation graph representation of ARG databases and a locality-sensitive hashing Forest indexing scheme to rapidly classify reads and reconstruct full-length gene sequences, improving accuracy in profiling similar ARG variants [17]. It can process a 2 GB metagenome in approximately 2 minutes on a single CPU [17].
Table 2: Key Research Reagent Solutions for Resistome Profiling
| Category | Item / Tool | Function / Description |
|---|---|---|
| Wet-Lab Reagents | QIAamp Fast DNA Stool Mini Kit | DNA extraction from fecal samples [10]. |
| PowerSoil DNA Isolation Kit | DNA extraction from complex environmental samples like soil [10]. | |
| Illumina MiSeq Nextera XT Kit | Library preparation for shotgun metagenomic sequencing [10]. | |
| CARPDM Probe Sets | Custom hybridization probes for targeted enrichment of ARGs from CARD [20]. | |
| Bioinformatic Tools | Prodigal | Prediction of protein-coding genes in metagenomic and genomic sequences [21]. |
| GROOT | Fast resistome profiling directly from metagenomic reads using variation graphs [17]. | |
| MetaPhlAn | Profiling microbial community composition from metagenomic data [10]. | |
| Reference Databases | Comprehensive Antibiotic Resistance Database (CARD) | Curated repository of ARGs, proteins, and antibiotics [20]. |
| ISfinder | Centralized database for insertion sequences (IS) [18] [19]. |
Investigating Horizontal Gene Transfer and MGEs
Understanding the dynamics of AMR requires moving beyond a simple catalog of ARGs to analyze their mobilization via HGT and MGEs.
Key Mobile Genetic Elements in AMR
MGEs are diverse and facilitate the movement of ARGs through different mechanisms.
- Insertion Sequences (IS): These are the simplest MGEs, typically short sequences ( <3 kb) containing only a transposase gene flanked by inverted repeats [18]. They can insert into genes, potentially inactivating them, or provide promoters that drive the expression of adjacent ARGs [19]. For example, ISAba1 inserted upstream of the blaOXA-51-like gene in Acinetobacter baumannii can lead to carbapenem resistance [19].
- Transposons: These are larger than IS and carry additional genes, such as ARGs. Composite transposons consist of a cargo gene (e.g., an ARG) flanked by two copies of the same or related IS, which can mobilize the entire unit [18] [19]. An example is Tn10, which carries a tetracycline resistance gene [19].
- Integrons: These are genetic platforms that can capture and express gene cassettes, most commonly ARGs [19]. They contain an intI gene encoding an integrase, a recombination site (attI), and a promoter for expressing the captured genes [18].
- Plasmids and ICEs: Plasmids are self-replicating MGEs that can transfer between cells via conjugation and often carry multiple ARGs [18] [22]. Integrative and conjugative elements (ICEs) can excise from the chromosome and transfer to a recipient cell via conjugation [18].
Protocol: Detecting HGT and MGE-Associated ARGs
Long-read sequencing is critical for resolving the genomic context of ARGs, as short reads cannot span repetitive MGE sequences.
Protocol: Resolving ARG Context with Long-Read Sequencing
- Principle: Long-read sequencing technologies, such as those from Oxford Nanopore Technologies (ONT) and Pacific Biosciences (PacBio), generate reads that are thousands of bases long. This allows them to span entire MGEs and resolve whether an ARG is located on a chromosome or a plasmid, and its specific association with IS, transposons, or integrons [22].
- Procedure: High-molecular-weight DNA is extracted and sequenced on a long-read platform. The resulting reads are assembled into complete, closed genomes (for isolates) or higher-quality metagenome-assembled genomes (MAGs). ARGs and MGEs are then annotated in the assembled genomes. The proximity and linkage of ARGs to MGEs are analyzed to provide direct evidence of their mobilizable nature [22].
- Application: This approach has been used to demonstrate that antibiotic selection can drive the duplication of ARGs via transposition in experimental evolution, and that duplicated ARGs are highly enriched in clinical and livestock-associated bacterial isolates, indicating strong ongoing selection [22].
MGEs as ARG Vectors
Integrated Application Notes
The combined application of these protocols provides powerful insights into AMR dynamics across different environments.
- One Health Surveillance: A study in Kathmandu, Nepal, used shotgun metagenomics on human, avian, and environmental samples, identifying 53 ARG subtypes [10]. Poultry samples showed the highest ARG diversity, suggesting intensive antibiotic use in agriculture as a key driver. The study also detected frequent HGT events, identifying gut microbiomes as critical reservoirs for ARGs, thus underscoring the interconnectedness of human, animal, and environmental health in the spread of AMR [10].
- Environmental Monitoring: Resistome profiling of urban gutter ecosystems in India revealed high levels of bacteria resistant to penicillin, cephalosporin, and other antibiotic classes [23]. Beta-lactamase activity was confirmed via a nitrocefin hydrolysis assay. Metagenomic analysis further linked the resistome to specific microbial families like Enterobacteriaceae and Pseudomonadaceae, and to metabolic pathways that may indirectly foster resistance development [23].
- Occupational Risk Assessment: Metagenomic analysis of a composting facility identified airborne human-pathogenic antibiotic-resistant bacteria (HPARB) carrying a greater diversity and abundance of ARGs and virulence factors than those found in the compost itself [24]. Key enriched ARGs in the air included mexF, tetW, and vanS, highlighting an underappreciated route of occupational exposure to enhanced AMR risks [24].
Linking Microbial Community Dynamics to Antibiotic Resistance Gene Abundance
Antimicrobial resistance (AMR) presents a major global threat to public health and ecosystems, with drug-resistant infections projected to cause nearly 2 million deaths annually by 2050 [25]. The resilience and dissemination of antibiotic resistance genes (ARGs) within microbial communities are heavily influenced by complex ecological dynamics and environmental factors. Metagenomic next-generation sequencing (mNGS) has emerged as a transformative tool for analyzing ARGs in diverse microbial communities without cultivation, enabling comprehensive insights into resistance mechanisms and transmission pathways [8] [26].
This Application Note provides detailed protocols for investigating the relationship between microbial community dynamics and ARG abundance using metagenomic approaches. We present standardized methodologies for sample processing, DNA extraction, sequencing, and computational analysis, with particular emphasis on tracking mobile genetic elements (MGEs) that facilitate horizontal gene transfer of resistance determinants [8].
Table 1: Comparison of Metagenomics and qPCR for ARG Analysis
| Parameter | Metagenomic Sequencing | Quantitative PCR (qPCR) |
|---|---|---|
| Gene Coverage | Broad coverage of known and novel ARGs [27] | Limited to targeted ARGs with known sequences [27] |
| Sensitivity | Lower sensitivity for rare ARGs [27] | High sensitivity for detecting low-abundance targets [27] |
| Quantitative Accuracy | Relative abundance based on read mapping [27] | Absolute quantification with high accuracy [27] |
| Throughput | High-throughput, community-wide profiling [8] | Medium throughput, limited by primer availability [28] |
| MGE Detection | Can link ARGs to plasmids, integrons, phages [25] [8] | Requires separate assays for MGE targets [28] |
| Cost per Sample | Higher | Lower |
Table 2: Temporal Dynamics of ARG Classes in Urban Wastewater [28]
| ARG Class | Detection Frequency (%) | Absolute Abundance Range (copies/L) | Dominant Gene Subtypes |
|---|---|---|---|
| Aminoglycosides | 70-90% | 6.94×10⁴ - 9.47×10⁴ | aph, aadA1, strB, aadA-02 |
| β-lactams | 70-87% | 9.36×10³ - 2.17×10⁴ | blaOXY, fox5, blaCTXM-01, blaOXA-30 |
| Sulfonamides/Trimethoprim | 67-83% | 8.83×10³ - 1.09×10⁴ | dfrA, sul2 |
| Multidrug | 50-70% | 3.25×10³ - 5.19×10³ | Multiple efflux pumps |
| MLSB | 50-65% | 1.94×10³ - 4.66×10³ | erm, mef, msr |
| Tetracyclines | 45-60% | 2.07×10³ - 3.20×10³ | tet(M), tet(32), tet(35) |
Metagenomic Co-Assembly Protocol for Enhanced ARG Detection
Principle
Co-assembly merges sequencing data from multiple related samples to improve gene recovery and facilitate detection of low-abundance ARGs that may be missed in individual assemblies. This approach is particularly valuable for low-biomass samples like airborne microbiomes where sequencing depth may be limited [25].
Materials and Reagents
- DNA extraction kit optimized for environmental samples (e.g., DNeasy PowerSoil Pro Kit)
- Quality control reagents: Qubit dsDNA HS Assay Kit, Agilent High Sensitivity DNA Kit
- Library preparation kit: Nextera XT DNA Library Preparation Kit (Illumina)
- Sequencing reagents: Illumina NextSeq or NovaSeq sequencing chemistry
- Bioinformatics software: MEGAHIT or metaSPAdes assembler, BBtools for quality control
Procedure
Sample Grouping Strategy
- Group samples based on taxonomic and functional characteristics
- Ensure similar environmental origins or experimental conditions
- Recommended group size: 5-10 samples for optimal co-assembly [25]
Sequencing Read Pooling
- Pool quality-filtered reads from all samples in the group
- Use consistent normalization approaches to avoid bias
- Recommended sequencing depth: ~30 million reads per group for saturation [25]
Co-assembly Execution
- Run MEGAHIT with metagenomic mode:
megahit -r pooled_reads.fq -o coassembly_output --min-contig-len 500 - Alternatively, use metaSPAdes:
metaspades.py -o coassembly_output -s pooled_reads.fq
- Run MEGAHIT with metagenomic mode:
Quality Assessment
- Compare assembly metrics: genome fraction, duplication ratio, mismatches per 100 kbp
- Evaluate contig length distribution (N50, maximum contig length)
- Validate with reference genomes representing expected taxa
Gene Prediction and Annotation
- Predict open reading frames using Prodigal:
prodigal -i coassembly.fna -a proteins.faa -p meta - Annotate ARGs using RGI with CARD database:
rgi main -i proteins.faa -o arg_annotations -t protein
- Predict open reading frames using Prodigal:
Expected Results
Co-assembly typically produces longer contigs (762,369 contigs ≥500 bp) compared to individual assembly (455,333 contigs), with significantly greater total contig length (555.79 million bp vs. 334.31 million bp) [25]. This enhances the ability to link ARGs to mobile genetic elements and determine genomic context.
Integrated Workflow for Community-ARG Dynamics
Workflow for analyzing microbial community dynamics and ARG abundance
Tracking Mobile Genetic Elements and Horizontal Gene Transfer
MGE Detection Protocol
Principle: Identify plasmids, integrons, transposons, and bacteriophages that facilitate horizontal transfer of ARGs between diverse microbial taxa [8].
Procedure:
Extract Contigs Potentially Encoding MGEs
- Screen assembled contigs using PlasFlow for plasmid identification
- Run geNomad for viral and plasmid sequence detection
- Use IntegronFinder for integron identification
Identify ARG-MGE Linkages
- Detect ARGs and MGEs on same contig using RGI and mobileOG-db
- Calculate linkage probability based on genetic distance
- Apply network analysis to identify ARG-MGE co-occurrence patterns
Validate HGT Potential
- Analyze flanking sequences of ARGs for MGE-associated features
- Identify insertion sequence elements adjacent to ARGs
- Detect integron cassette structures containing ARGs
Expected Results: In atmospheric samples, co-assembly approaches reveal ARGs against aminoglycosides, beta-lactams, fosfomycin, glycopeptides, quinolones, and tetracyclines, though many may not be clearly linked to mobile elements due to community complexity [25].
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Computational Tools
| Category | Product/Tool | Specific Function | Application Notes |
|---|---|---|---|
| Wet Lab | DNeasy PowerSoil Pro Kit | DNA extraction from diverse environmental samples | Optimal for low-biomass samples [25] |
| Wet Lab | Nextera XT DNA Library Prep | Metagenomic library preparation | Compatible with low-input DNA [27] |
| Bioinformatics | ResistoXplorer | Visual, statistical analysis of resistome data | Web-based tool for exploratory analysis [29] |
| Bioinformatics | AMRViz | Genomics analysis & visualization of AMR | Provides end-to-end pipeline management [30] |
| Bioinformatics | MEGAHIT | Metagenome assembly | Efficient for complex communities [25] |
| Database | CARD Database | Reference ARG sequences | Comprehensive resistance gene database [26] |
| Database | ResFinder | ARG detection & subtyping | Specialized for resistance surveillance [27] |
| Analysis | RGI (Resistance Gene Identifier) | ARG annotation from sequences | Integrates with CARD database [26] |
Data Analysis and Visualization Protocol
Statistical Analysis of Community-ARG Associations
Procedure:
Normalization and Transformation
- Apply CSS normalization to account for uneven library sizes
- Use log-ratio transformations for compositional data
- Rarefy to even sequencing depth when comparing alpha diversity
Differential Abundance Testing
- Implement metagenomeSeq with zero-inflated Gaussian model
- Use DESeq2 or edgeR adapted for metagenomic data
- Apply Benjamini-Hochberg correction for multiple testing
Network Analysis
- Construct co-occurrence networks using SparCC or SPIEC-EASI
- Calculate topological features: betweenness centrality, modularity
- Identify keystone taxa influencing ARG distribution
Temporal Analysis
- Track persistent (core) versus transient ARGs across time series
- Calculate ARG turnover rates using Bray-Curtis dissimilarity
- Identify seasonal patterns in resistance prevalence [28]
Visualization with ResistoXplorer
Procedure:
Upload Data Format
- Prepare ARG abundance table with samples as columns, genes as rows
- Include metadata table with experimental factors
- Format according to ResistoXplorer specifications [29]
Composition Profiling
- Generate alpha diversity rarefaction curves
- Create ordination plots (PCoA, NMDS) based on Bray-Curtis distances
- Visualize ARG class distribution across sample groups
Functional Profiling
- Aggregate ARGs by drug class resistance mechanism
- Compare functional profiles across experimental conditions
- Identify enriched resistance mechanisms
Association Network Visualization
- Construct ARG-microbe association networks
- Apply enrichment analysis to identify significant associations
- Export publication-quality figures
Applications and Case Studies
Atmospheric ARG Transport During Dust Storms
Background: Airborne transport represents an understudied pathway for ARG dissemination across geographical barriers [25].
Methods Implementation:
- Sample air during clear weather and dust storm events
- Apply metagenomic co-assembly to enhance gene recovery
- Link detected ARGs to potential bacterial hosts
- Assess mobility potential through MGE association
Key Findings: Co-assembly of atmospheric samples reveals resistance genes against clinically important antibiotics, demonstrating potential for long-range airborne spread of antibiotic resistance [25].
Wastewater-Based Epidemiology of Community AMR
Background: Urban wastewater provides integrated assessment of community-wide resistance patterns [28].
Methods Implementation:
- Collect wastewater samples monthly over 5-month period
- Extract DNA and analyze 123 ARGs and 13 MGEs using qPCR
- Identify persistent (core) versus transient resistance genes
- Correlate ARG abundance with seasonal factors
Key Findings: Approximately 50% of tested ARG subtypes were consistently detected across all months, with maximum absolute abundance in winter months, highlighting persistent core resistome in urban communities [28].
Troubleshooting Guide
Table 4: Common Technical Challenges and Solutions
| Problem | Potential Cause | Solution |
|---|---|---|
| Low ARG detection sensitivity | Insufficient sequencing depth | Increase to ≥30 million reads; implement co-assembly [25] |
| Incomplete MGE linkage | Fragmented assemblies | Apply long-read sequencing; use hybrid assembly approaches |
| High false positive ARGs | Database mismatches | Use curated databases; apply conservative identity thresholds |
| Poor community resolution | Low biomass sample | Optimize DNA extraction; include amplification steps |
| Inconsistent temporal patterns | Sampling frequency | Increase sampling points; align with environmental drivers [28] |
| Compositional data artifacts | Uneven library sizes | Apply proper normalization (CSS, log-ratio) [29] |
This protocol collection provides comprehensive methodologies for investigating the dynamic relationships between microbial communities and antibiotic resistance genes. The integrated approach combining wet lab procedures, bioinformatics analyses, and visualization tools enables researchers to track the emergence and dissemination of resistance determinants across diverse environments. Standardized application of these protocols will enhance comparability across studies and contribute to the global understanding of antimicrobial resistance dynamics within the One Health framework.
The Critical Role of Bioinformatics and Reference Databases in Data Interpretation
The rise of antimicrobial resistance (AMR) presents a critical global health challenge, linked to millions of deaths annually [31]. Metagenomic next-generation sequencing (mNGS) has emerged as a transformative tool for infectious disease diagnostics, enabling the hypothesis-free detection of a broad spectrum of pathogens and their resistance genes directly from clinical samples [31]. However, the power of this culture-independent approach is entirely dependent on robust bioinformatics pipelines and comprehensive reference databases. Without sophisticated computational tools, the vast and complex datasets generated by mNGS are uninterpretable. This application note details the essential protocols and resources for accurately identifying AMR genes from mNGS data, framing them within the critical context of data interpretation for researchers and drug development professionals.
The fundamental challenge in mNGS for AMR analysis lies in distinguishing genuine resistance determinants from background noise and understanding their clinical relevance. Unlike whole-genome sequencing (WGS) of isolated bacterial strains, mNGS involves sequencing all nucleic acids in a sample, resulting in a mixture of host, pathogen, and environmental DNA [31]. This complexity introduces several analytical hurdles, including high levels of host DNA, the need for sensitive detection of low-abundance genes, and the functional annotation of discovered genes. Bioinformatics tools and curated databases are the essential components that overcome these hurdles, translating raw sequence data into actionable insights for managing drug-resistant infections.
Essential Bioinformatics Tools and Databases for AMR Detection
A wide array of bioinformatic tools has been developed to identify AMR genes from sequencing data. These tools primarily function by comparing sequenced DNA or protein fragments against curated databases of known resistance genes and mutations. The selection of the tool and database directly impacts the sensitivity, specificity, and overall accuracy of the analysis. Key tools include ResFinder, the Comprehensive Antibiotic Resistance Database (CARD), AMRFinderPlus, and newer, more comprehensive platforms like AmrProfiler [32] [33].
These tools differ in their algorithms, database composition, and the types of resistance mechanisms they detect. While early tools focused mainly on acquired resistance genes, modern pipelines have expanded to detect chromosomal mutations, ribosomal RNA (rRNA) mutations, and other complex resistance mechanisms. For instance, AmrProfiler is the first tool to systematically report mutations in rRNA genes, which is critical for identifying resistance to antibiotics like macrolides and oxazolidinones in Gram-positive bacteria [32]. The choice of tool often depends on the specific application, the required comprehensiveness, and the user's bioinformatics expertise.
Table 1: Comparison of Key Bioinformatic Tools for AMR Gene Detection
| Tool Name | Primary Function | Database Source & Size | Key Features | Limitations |
|---|---|---|---|---|
| AmrProfiler | Identifies acquired AMR genes, core gene mutations, and rRNA mutations. | Integrates ResFinder, CARD & Reference Gene Catalog; 7,588 unique AMR gene alleles [32]. | Three specialized modules; analyzes ~18,000 bacterial species; reports rRNA copy number mutation ratio. | Web server dependent; may have processing delays with large datasets. |
| ResFinder | Detects acquired antimicrobial resistance genes. | Custom database; 3,150 alleles [32]. | User-friendly online platform; widely used and cited. | Limited coverage for point mutations; can miss known AMR genes [32]. |
| CARD | Comprehensive identification of AMR genes and mutations. | Custom curated database; 4,793 unique AMR gene alleles [32]. | Extensive ontology of resistance terms; includes broad mechanism data. | Confidence in AMR relevance can be low for some entries [32]. |
| AMRFinderPlus | Detects AMR genes, point mutations, and stress resistance elements. | NCBI Reference Gene Catalog; 6,637 AMR gene alleles [32]. | Detects a wide range of mechanisms; stand-alone tool. | Can be challenging for non-bioinformaticians to use [32]. |
Protocol for AMR Gene Detection from mNGS Data
Sample Processing, Sequencing, and Quality Control
The initial steps involve converting a clinical sample into high-quality sequencing data suitable for bioinformatic analysis.
- Sample Collection & Nucleic Acid Extraction: Collect clinical specimen (e.g., blood, bronchoalveolar lavage fluid, cerebrospinal fluid) in appropriate sterile containers. Extract total DNA/RNA using standardized commercial kits, ensuring sufficient yield and integrity. For RNA viruses, include a reverse transcription step to generate cDNA.
- Library Preparation & Host DNA Depletion: Convert the extracted nucleic acids into a sequencing library using library preparation kits. This typically involves fragmentation, end-repair, adapter ligation, and PCR amplification. To significantly improve the detection of microbial content, implement host DNA depletion techniques (e.g., probe-based hybridization) prior to or during library prep, especially for samples with high human host content [31].
- Sequencing: Load the prepared library onto a next-generation sequencer (e.g., Illumina, Oxford Nanopore Technologies (ONT), or PacBio). For short-read platforms, aim for a minimum of 10-20 million reads per sample. ONT's portable devices like the MinION enable real-time, point-of-care sequencing [31].
- Raw Data Quality Control & Preprocessing: Perform initial quality assessment on the raw sequencing reads (FASTQ files). Use tools like FastQC to evaluate per-base sequence quality, GC content, and adapter contamination. Subsequently, preprocess the reads with Trimmomatic or Cutadapt to remove low-quality bases, sequencing adapters, and short reads.
Bioinformatic Analysis for AMR Gene Identification
This core protocol transforms quality-controlled reads into a list of annotated AMR genes.
- Taxonomic Profiling (Optional but Recommended): Classify the sequencing reads to determine the microbial composition of the sample. This provides context for the AMR genes found. Tools like Kraken2 or Centrifuge can be used for rapid taxonomic assignment.
- Resistance Gene Detection: This is the central step for AMR analysis. This protocol uses AmrProfiler as a comprehensive example.
- Input: Preprocessed reads (after step 4 above) should be assembled into contigs using a de novo assembler like MEGAHIT or metaSPAdes. The final assembly (FASTA file) is the input for AmrProfiler.
- Tool Access: Navigate to the AmrProfiler web server at
https://dianalab.e-ce.uth.gr/amrprofiler[32]. - Module 1 - Acquired AMR Genes:
- Upload the genome assembly file.
- Select the "Acquired AMR Genes" module.
- Set user-defined thresholds for identity (e.g., ≥90%) and coverage (e.g., ≥80%) to filter hits. This ensures high-confidence matches.
- Execute the analysis. The tool performs a BLASTX search against its curated database of 7,588 AMR gene alleles [32].
- Module 2 - Core Gene Mutations:
- Select the "Core Gene Mutations" module.
- Specify the bacterial species of interest from the ~18,000 available.
- Run the analysis to detect mutations in resistance-associated core genes (e.g., gyrA, parC) compared to a reference genome.
- Module 3 - rRNA Genes and Mutations:
- Select the "rRNA Genes and Mutations" module.
- This module identifies all 5S, 16S, and 23S rRNA gene copies and detects mutations compared to the species-specific reference, calculating the mutated-to-total rRNA copy number ratio [32].
- Results Interpretation: AmrProfiler generates a table of all identified AMR alleles, core gene mutations, and rRNA mutations, along with metadata such as product names and associated phenotypes [32]. Correlate these findings with the taxonomic profile and clinical data.
The following workflow diagram outlines the key steps for detecting antimicrobial resistance using mNGS, from sample preparation to final analysis.
Diagram 1: mNGS AMR Analysis Workflow: This chart outlines the process from sample to AMR report, highlighting key stages including host DNA depletion and comprehensive bioinformatic analysis.
The Scientist's Toolkit: Key Research Reagents and Materials
Successful execution of the aforementioned protocols requires a suite of reliable laboratory and computational resources. The following table details essential materials and their functions in mNGS-based AMR studies.
Table 2: Essential Research Reagent Solutions for mNGS-based AMR Analysis
| Category | Item / Reagent | Function / Application |
|---|---|---|
| Sample Processing | Total Nucleic Acid Extraction Kits (e.g., Qiagen DNeasy/RNeasy) | Isolates high-quality, PCR-amplifiable DNA/RNA from complex clinical samples. |
| Host Depletion Kits (e.g., NEBNext Microbiome DNA Enrichment Kit) | Selectively removes human host DNA to increase microbial sequencing depth [31]. | |
| Library Prep & Sequencing | Library Preparation Kits (e.g., Illumina Nextera XT, ONT Ligation Kit) | Fragments nucleic acids and attaches platform-specific adapters for sequencing. |
| Sequencing Flow Cells (e.g., Illumina MiSeq, ONT MinION R9) | Solid-phase surface where clonal amplification and sequencing-by-synthesis occur. | |
| Bioinformatics & Databases | AmrProfiler Web Server | Open-access tool for comprehensive AMR gene, mutation, and rRNA analysis [32]. |
| CARD & ResFinder Databases | Curated reference databases of known AMR genes used for sequence alignment and annotation [32] [33]. | |
| RefSeq Genome Database | NCBI's comprehensive collection of reference genomes for mutation analysis and comparison [32]. |
The accurate interpretation of mNGS data for antimicrobial resistance research is fundamentally reliant on the synergistic use of advanced bioinformatics tools and meticulously curated reference databases. As the field progresses, the integration of these computational resources with standardized wet-lab protocols will be paramount for translating raw genomic data into clinically actionable information that can inform stewardship and drug development efforts.
From Sample to Insight: mNGS Workflows and Applications in AMR Research
The rise of antimicrobial resistance (AMR) presents a critical global health threat, directly causing an estimated 1.27 million deaths annually and contributing to nearly 5 million more [8]. Effectively combating this crisis requires robust surveillance strategies that can track the emergence and dissemination of resistance genes across human, animal, and environmental reservoirs—the core principle of the One Health approach [34] [35].
Next-generation sequencing (NGS) has revolutionized AMR surveillance, moving beyond traditional, slower culture-based methods. Two powerful NGS methodologies are now at the forefront: shotgun metagenomics and targeted NGS (tNGS). Shotgun metagenomics provides a comprehensive, unbiased view of all genetic material in a sample, while tNGS uses enrichment techniques to focus sequencing power on specific genomic targets [36]. This application note details the strengths, limitations, and optimal use cases for each method to guide researchers in selecting the right tool for their AMR research objectives.
Shotgun Metagenomics (SMg)
Shotgun metagenomics involves sequencing all nucleic acids in a sample without prior targeting, allowing for the simultaneous detection of a vast array of microorganisms (bacteria, viruses, fungi, archaea) and their genes, including known and novel antimicrobial resistance genes (ARGs) and virulence factors [8] [34]. Its principal strength lies in its unbiased, hypothesis-free approach, making it ideal for pathogen discovery, characterizing complex microbial communities, and comprehensively profiling the "resistome" [34] [10].
Targeted NGS (tNGS)
Targeted NGS employs enrichment techniques to selectively sequence predefined genomic regions of interest before sequencing. The two primary tNGS approaches are:
- Amplification-based tNGS: Uses ultra-multiplex PCR with panels of primers to amplify specific target pathogens and ARGs [36].
- Capture-based tNGS: Uses solution-phase hybrid capture with probe panels to enrich for target sequences [36].
The key advantage of tNGS is its enhanced sensitivity for pre-specified targets, achieved by reducing host and non-target background DNA [37] [38].
Head-to-Head Comparison
The choice between shotgun metagenomics and tNGS involves balancing multiple factors, including scope, sensitivity, cost, and turnaround time. The table below summarizes their comparative performance based on recent studies.
Table 1: Comparative Analysis of Shotgun Metagenomics and Targeted NGS for AMR Surveillance
| Feature | Shotgun Metagenomics (SMg) | Targeted NGS (tNGS) |
|---|---|---|
| Scope & Bias | Unbiased, hypothesis-free; detects expected and novel pathogens/ARGs [34]. | Targeted, hypothesis-driven; limited to predefined pathogens/ARGs on the panel [37]. |
| Sensitivity | Lower sensitivity for low-abundance targets due to high background [36]. | Higher sensitivity for targeted pathogens/ARGs; superior for low-biomass samples [38] [36]. |
| Polymicrobial Infection Detection | Excellent; can characterize complex communities [10]. | Capture-based: Good. Amplification-based: Can struggle with mixed templates [36]. |
| Turnaround Time (TAT) | Longer (~20 hours reported) [36]. | Shorter than SMg; streamlined workflow [37]. |
| Cost | Higher (e.g., ~$840/sample reported) [36]. | Lower cost per sample [36]. |
| Ability to Detect Novel ARGs/Pathogens | Yes [8]. | No, limited to panel content. |
| Typing & Context | Enables strain-level typing, phylogenetic analysis, and ARG linkage to Mobile Genetic Elements (MGEs) [39] [40]. | Primarily for identification; limited contextual genomic information. |
| Ideal Use Case | Discovery, resistome profiling, One Health environmental screening, outbreak investigation of unknown origin [34] [10]. | Routine diagnostics, rapid results, confirming suspected pathogens, testing when resources are limited [38] [36]. |
A 2025 comparative study on lower respiratory infections quantitatively underscored these trade-offs. While SMg identified the most species (80), capture-based tNGS demonstrated the highest diagnostic accuracy (93.17%) and sensitivity (99.43%) against a comprehensive clinical standard. Amplification-based tNGS, though fast and cost-effective, showed poor sensitivity for gram-positive (40.23%) and gram-negative (71.74%) bacteria [36].
Detailed Experimental Protocols
Protocol for Shotgun Metagenomic Analysis of AMR
This protocol is adapted from studies investigating resistomes in human, animal, and environmental samples [10] and periprosthetic infections [39].
Sample Preparation and DNA Extraction:
- Sample Collection: Collect samples (e.g., fecal, tissue, water, soil) in sterile containers. Immediately freeze at -80°C or preserve in RNAlater or glycerol buffer to maintain nucleic acid integrity [10].
- Homogenization: Mechanically homogenize samples using bead beating with vortex adapters to ensure efficient lysis of diverse microorganisms, particularly those in biofilms [39].
- Nucleic Acid Extraction: Use commercial kits designed for complex samples (e.g., QIAamp Fast DNA Stool Mini Kit, PowerSoil DNA Isolation Kit). Include a step to remove host DNA using nucleases (e.g., Benzonase) to increase microbial sequencing depth [36] [10].
- Quality Control: Quantify DNA using a fluorometer (e.g., Qubit) and assess quality/fragment size via agarose gel electrophoresis or Bioanalyzer [10].
Library Preparation and Sequencing:
- Library Construction: Use Illumina Nextera XT or similar library prep kits for double-stranded DNA. For RNA virus detection, include a step for ribosomal RNA depletion and reverse transcription [36].
- Sequencing: Perform shotgun sequencing on an Illumina platform (e.g., MiSeq, NextSeq). Aim for a minimum of 20 million high-quality reads per sample to ensure sufficient depth for detecting low-abundance ARGs [36] [39].
Bioinformatic Analysis for AMR Profiling:
- Quality Control and Host Depletion: Use Fastp to remove adapter sequences and low-quality reads. Map reads to the host genome (e.g., hg38) using BWA and remove aligning reads [36].
- Taxonomic Profiling: Classify remaining reads using Kraken2/Bracken or MetaPhlAn against microbial genome databases [39] [10].
- ARG and MGE Detection: Align reads to AMR databases (e.g., NCBI's Bacterial Antimicrobial Resistance Reference Gene Database, ResFinder, CARD) using tools like SRST2 or ABRicate. For MGEs (plasmids, integrons, transposons), use dedicated databases and tools [8] [39].
- Assembly and Contextual Analysis (Optional but Recommended): For complex analysis, assemble reads into contigs using metaSPAdes. Bin contigs into Metagenome-Assembled Genomes (MAGs) using MaxBin. This allows for linking ARGs to their bacterial hosts and associated MGEs, providing insight into horizontal gene transfer potential [39] [40].
Protocol for Targeted NGS (tNGS) for AMR
This protocol is based on clinical studies using tNGS for pathogen identification and ARG detection in respiratory infections and periprosthetic joint infections (PJI) [38] [36].
Sample Processing and Targeted Enrichment: For Capture-based tNGS:
- DNA Extraction: Extract total nucleic acids from samples (e.g., BALF, sonicate fluid) using kits like MagPure Pathogen DNA/RNA Kit [36].
- Library Preparation: Construct sequencing libraries from extracted DNA.
- Hybrid Capture: Incubate libraries with biotinylated probes designed to target specific genomic regions of pathogens and ARGs. Wash away non-hybridized DNA [36].
- Amplification: Amplify the captured target libraries via PCR.
For 16S rRNA Gene-based tNGS (for Bacterial ID):
- DNA Extraction: As above.
- PCR Amplification: Amplify hypervariable regions of the bacterial 16S rRNA gene (e.g., V1-V3, V3-V4) using broad-range primers [38].
- Library Construction: Prepare sequencing libraries from the amplicons.
Sequencing and Analysis:
- Sequencing: Sequence the enriched libraries on mid-output Illumina platforms (e.g., MiSeq, MiniSeq). Fewer reads are required compared to SMg (e.g., ~100,000 reads/sample) [38] [36].
- Bioinformatic Analysis:
- Demultiplexing: Assign reads to samples based on barcodes.
- Quality Filtering: Remove low-quality reads.
- Pathogen/ARG Identification: For capture-based tNGS, align reads to a curated database of pathogens and ARGs. For 16S tNGS, cluster high-quality sequences into Operational Taxonomic Units (OTUs) and assign taxonomy using a reference database (e.g., SILVA) [38].
- Interpretation: Apply thresholds for positivity. For 16S tNGS, this may include a minimum read abundance (e.g., >10% of total reads) and verification that the species is not a known contaminant [38].
The Scientist's Toolkit: Essential Reagents and Tools
Table 2: Key Research Reagent Solutions for Metagenomic AMR Studies
| Reagent / Tool | Function | Example Products / Kits |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from complex matrices (stool, soil, sonicate fluid). | QIAamp Fast DNA Stool Mini Kit, PowerSoil DNA Isolation Kit, MagPure Pathogen DNA/RNA Kit [36] [10]. |
| Host Depletion Reagents | Selective removal of human/host DNA to increase microbial sequencing depth. | Benzonase, Tween20 [36]. |
| Library Prep Kits | Preparation of sequencing-ready libraries from fragmented DNA. | Illumina Nextera XT DNA Library Prep Kit, Ovation Ultralow System V2 [36]. |
| Targeted Enrichment Panels | Multiplex PCR or hybrid-capture panels for enriching pathogen and ARG sequences. | AmpliSeq for Illumina Antimicrobial Resistance Panel, Respiratory/Urinary Pathogen ID/AMR Enrichment Panels [41]. |
| 16S rRNA PCR Primers | Amplification of conserved bacterial 16S rRNA gene regions for taxonomic profiling. | 515F/806R (targeting V3-V4 regions) [10]. |
| Sequencing Platforms | High-throughput sequencing of prepared libraries. | Illumina MiSeq, NextSeq; Oxford Nanopore Technologies (ONT) platforms [41] [40]. |
| Bioinformatic Databases | Reference databases for taxonomic assignment and ARG/MGE identification. | NCBI AMR Reference Gene Database, CARD, ResFinder, SILVA (16S rRNA) [38] [39]. |
Application within a One Health Framework
Genomic AMR surveillance is most effective when implemented within a One Health framework, integrating data from human, animal, and environmental sectors [34] [35]. Shotgun metagenomics and tNGS play complementary roles in this endeavor.
Shotgun metagenomics is exceptionally well-suited for initial environmental reconnaissance and resistome profiling. For instance, a 2025 study in Nepal used SMg on human and animal feces, soil, and water, identifying 53 ARG subtypes and demonstrating that poultry samples served as significant resistance reservoirs. This approach revealed frequent horizontal gene transfer events, highlighting the interconnectedness of resistomes across different ecosystems [10].
Targeted NGS finds its strength in focused surveillance and clinical diagnostics. Its high sensitivity is crucial for monitoring specific high-priority pathogens (e.g., WHO priority pathogens) and their associated resistance mechanisms in clinical or veterinary settings [34]. For example, tNGS showed a positive percent agreement of 72.1% for diagnosing periprosthetic joint infection, significantly outperforming culture (52.9%) and proving invaluable in culture-negative cases [38].
The decision between shotgun metagenomics and targeted NGS is not a matter of choosing the universally superior technology, but rather the right tool for the specific research question and context.
- Choose Shotgun Metagenomics for exploratory studies, comprehensive resistome characterization, pathogen discovery, and when investigating the genetic context of ARGs (e.g., linkage to MGEs) is a priority [8] [39] [10].
- Choose Targeted NGS for routine surveillance of known pathogens, rapid clinical diagnostics, when sample input or pathogen biomass is low, and when cost and turnaround time are critical factors [38] [36].
Future advancements will see greater integration of these approaches, such as using SMg for broad surveillance to inform the design of more comprehensive tNGS panels. Furthermore, the adoption of long-read sequencing technologies (e.g., Oxford Nanopore, PacBio) is overcoming historical limitations in metagenomics. These technologies enable more complete genome assemblies, precise plasmid reconstruction, and novel methods for linking ARG-carrying plasmids to their bacterial hosts through DNA methylation profiling, thereby providing a more holistic view of AMR transmission dynamics [40]. As these tools evolve and standardize, they will profoundly enhance our ability to conduct proactive, integrated AMR surveillance across the One Health spectrum.
Within metagenomic next-generation sequencing (mNGS) research on antimicrobial resistance (AMR), the choice between whole-cell DNA (wcDNA) and cell-free DNA (cfDNA) analysis is a critical determinant of experimental success. This sample preparation decision significantly impacts the sensitivity, specificity, and representativeness of detected pathogens and their resistance genes. wcDNA provides a comprehensive view of intact microorganisms, whereas cfDNA offers a snapshot of recently lysed cells and extracellular genetic material, each with distinct advantages for specific clinical and research scenarios. Framed within the broader objective of analyzing antimicrobial resistance genes, this document provides detailed application notes and protocols to guide researchers in selecting and implementing the most appropriate sample preparation methodology.
Performance Comparison: wcDNA vs. cfDNA
The choice between wcDNA and cfDNA extraction methods leads to significant differences in performance metrics, influenced by the sample type and the target pathogens. The following table summarizes key comparative data from recent clinical studies.
Table 1: Comparative Performance of wcDNA and cfDNA mNGS in Clinical Studies
| Study & Sample Type | Metric | wcDNA mNGS | cfDNA mNGS | Conventional Methods |
|---|---|---|---|---|
| Pulmonary Infections (BALF) [42] | Detection Rate | 83.1% | 91.5% | 26.9% |
| Total Coincidence Rate | 63.9% | 73.8% | 30.8% | |
| CNS Infections (CSF) [43] | Sensitivity | 32.0% | 60.2% | 20.9% |
| Body Fluid Samples [44] | Concordance with Culture | 63.33% | 46.67% | (Benchmark) |
| Mean Host DNA Proportion | 84% | 95% | Not Applicable |
- Pathogen-Specific Efficiency: The superiority of cfDNA is particularly pronounced for certain pathogen types. In pulmonary infections, cfDNA detected a significantly higher proportion of fungi (31.8% vs 19.7% for wcDNA), viruses (38.6% vs 14.3%), and intracellular microbes (26.7% vs 6.7%) that would have been missed by the other method [42]. Similarly, for central nervous system (CNS) infections, most viral (72.6%) and mycobacterial (68.8%) pathogens were detected exclusively by cfDNA mNGS [43].
- Microbial Load Considerations: The advantage of cfDNA is most evident for pathogens with low microbial loads. For microbes with low reads per million (RPM), cfDNA detects a greater number and diversity of fungi, viruses, and intracellular organisms. In contrast, the ability of both methods to detect microbes with high loads is comparable [42].
- Host DNA Contamination: A critical technical consideration is the higher proportion of host DNA in cfDNA extracts from body fluids, averaging 95% compared to 84% in wcDNA extracts. This high background of host nucleic acids can potentially impact the sensitivity of pathogen detection by reducing the sequencing depth available for microbial reads [44].
Detailed Experimental Protocols
Sample Collection and Preprocessing
- Bronchoalveolar Lavage Fluid (BALF) / Cerebrospinal Fluid (CSF): Collect samples into sterile containers. Transport immediately on ice for processing [42] [43].
- Urine Samples: Centrifuge 1 mL of urine at 20,000 × g for 5 minutes. Discard 800 μL of supernatant and resuspend the pellet in the remaining 200 μL [45].
- Stool Samples: For gut microbiome analysis, standardize handling using a stool preprocessing device (SPD) prior to DNA extraction to improve yield, standardization, and recovery of Gram-positive bacteria [46].
DNA Extraction Protocols
A cfDNA Extraction Protocol
This protocol is adapted for BALF or CSF samples using the QIAamp DNA Micro Kit [42] [43].
- Centrifugation: Centrifuge the BALF or CSF sample to remove cells and debris. Use the resulting supernatant for extraction.
- cfDNA Extraction: Extract DNA from the supernatant using the QIAamp DNA Micro Kit, following the manufacturer's instructions.
- DNA Quantification: Measure the concentration and quality of the extracted cfDNA using a fluorometer (e.g., Qubit 4.0).
This gentle extraction avoids the DNA shearing associated with vigorous cell lysis, making it suitable for recovering fragmented cfDNA from pathogens.
B wcDNA Extraction Protocol
This protocol is for comprehensive lysis of all cells in a sample and is suitable for various body fluids [42] [43] [44].
- Direct Processing: Use the total BALF or CSF sample without preliminary centrifugation.
- Bead-Beating Lysis: Subject the sample to mechanical lysis using a bead-beating method with ceramic, glass, or zirconia beads to ensure rupture of tough cell walls (e.g., Gram-positive bacteria).
- DNA Purification: Extract and purify total DNA using a kit such as the QIAamp DNA Micro Kit or the DNeasy PowerLyzer PowerSoil Kit.
- Alternative: Enzymatic Lysis: For long-read sequencing applications where DNA integrity is paramount, enzymatic lysis can be employed. Incubate the sample with a lytic enzyme solution (e.g., MetaPolyzyme) at 37°C for 1 hour with gentle shaking [45].
Library Construction and Sequencing
- Library Preparation: Construct DNA libraries using a low-input library preparation kit (e.g., QIAseq Ultralow Input Library Kit). For AMR-focused studies, hybrid capture-based enrichment with probes designed for microbial genomes and resistance genes can be employed [5].
- Quality Control: Assess library quality using an Agilent 2100 Bioanalyzer.
- Sequencing: Sequence qualified libraries on a next-generation platform (e.g., Illumina Nextseq 550) to a depth of approximately 20 million reads per library [5].
Bioinformatic Analysis for AMR Gene Detection
- Preprocessing: Remove adapter sequences and low-quality reads from the raw sequencing data.
- Host Depletion: Map reads to the host reference genome (e.g., hg38) and subtract them to enrich for microbial sequences.
- Taxonomic Profiling: Align non-host reads to a comprehensive microbial genome database (e.g., NCBI) to identify pathogenic species.
- AMR Gene Identification: Detect known resistance genes by aligning sequences against curated AMR databases such as the Comprehensive Antibiotic Resistance Database (CARD) using tools like the Resistance Gene Identifier (RGI) [47].
The following workflow diagram illustrates the parallel and distinct steps in wcDNA and cfDNA analysis.
Application in Antimicrobial Resistance (AMR) Research
The accurate prediction of AMR phenotypes from mNGS data presents a significant challenge and opportunity. mNGS can simultaneously detect pathogenic species and their resistance-associated genes or mutations directly from clinical samples, providing a culture-independent diagnostic tool [5].
- Performance in Pediatric Pneumonia: A recent study on pediatric severe pneumonia demonstrated that mNGS has variable predictive performance for AMR, which is highly dependent on both the bacterial species and the class of antibiotic. For instance, the sensitivity of mNGS in predicting carbapenem resistance was relatively high (67.74%), particularly for Acinetobacter baumannii (94.74%). However, its sensitivity for predicting resistance to penicillins and cephalosporins was much lower (28.57% and 46.15%, respectively) [5].
- Complementary Role to Phenotypic Testing: These findings indicate that while mNGS shows promise as a rapid supplementary tool for AMR prediction, it currently cannot replace conventional phenotypic susceptibility testing (PST). The correlation between the presence of a resistance gene and the phenotypic expression of resistance is not always absolute, necessitating a combined approach for clinical decision-making [5].
- Benchmarking and Standardization: The development of gold-standard reference datasets, such as those comprising 174 bacterial genomes with known AMR profiles, is vital for benchmarking bioinformatic tools and pipelines used to predict AMR from both genomic and metagenomic sequencing data [47].
The Scientist's Toolkit: Essential Reagents and Equipment
Successful implementation of wcDNA and cfDNA protocols requires specific laboratory reagents and instruments. The following table lists key solutions for the core experimental procedures described in this document.
Table 2: Essential Research Reagents and Equipment
| Item Name | Function / Application | Example Vendor/Kit |
|---|---|---|
| QIAamp DNA Micro Kit | DNA extraction from supernatant (cfDNA) or pellet (wcDNA). | QIAGEN |
| DNeasy PowerLyzer PowerSoil Kit | wcDNA extraction with robust bead-beating for difficult-to-lyse cells. | QIAGEN |
| MetaPolyzyme | Enzymatic lysis for gentle extraction of HMW DNA, suitable for long-read sequencing. | Sigma Aldrich |
| QIAseq Ultralow Input Library Kit | Library construction from low-concentration DNA extracts. | QIAGEN |
| IndiSpin Pathogen Kit | DNA extraction and purification, used in comparative method studies. | Indical Bioscience |
| Quick-DNA HMW MagBead Kit | Isolation of high molecular weight DNA for long-read sequencing. | Zymo Research |
| Benzonase | Enzymatic host nucleic acid depletion to enrich for microbial sequences. | Sigma |
| Nextseq 550 Platform | High-throughput sequencing of constructed libraries. | Illumina |
| MinION Device | Portable, real-time long-read sequencing. | Oxford Nanopore Technologies |
| Qubit 4.0 Fluorometer | Accurate quantification of DNA concentration and quality. | Thermo Fisher Scientific |
The decision to use wcDNA or cfDNA for mNGS-based AMR research is context-dependent. wcDNA, with its rigorous lysis, provides a comprehensive profile of the entire microbial community within a sample and is crucial for detecting intracellular and hard-to-lyse pathogens. In contrast, cfDNA, derived from supernatant, offers high sensitivity for detecting extracellular and recently lysed pathogens, proving particularly advantageous in sterile site infections like pneumonia and meningitis. For a holistic approach to pathogen detection and AMR profiling, especially in polymicrobial infections, a dual-pathway strategy that incorporates both wcDNA and cfDNA analysis may yield the most comprehensive and clinically actionable results.
The accurate detection and characterization of antimicrobial resistance (AMR) genes through metagenomic next-generation sequencing (mNGS) is a critical component in the global effort to combat multidrug-resistant pathogens. The precision of this genotypic analysis is fundamentally dependent on the wet-lab workflow, including DNA extraction, library preparation, and the selection of sequencing platforms [48] [49]. Variations in these initial steps can significantly impact parameters such as sequencing depth, genome assembly quality, and the subsequent ability to detect single nucleotide polymorphisms (SNPs) and AMR genes with high confidence [50]. This application note provides detailed, actionable protocols for these foundational procedures, contextualized within AMR-focused metagenomic research, to ensure the generation of highly reliable and actionable data.
The foundational wet-lab workflow for mNGS-based AMR analysis consists of several critical stages, each with decision points that influence the final result. The schematic below illustrates the complete pathway and the key choices at each step.
Diagram 1: Comprehensive mNGS Wet-Lab Workflow for AMR Research. This workflow outlines the key stages from sample to sequence, highlighting critical methodological choices that influence the detection and accurate characterization of antimicrobial resistance genes. The choice between long- and short-read sequencing is particularly pivotal for resolving mobile genetic elements like plasmids, which are primary vectors for AMR gene dissemination [51].
Detailed Experimental Protocols
DNA Extraction Procedures for Diverse Sample Types
The integrity of the genomic DNA (gDNA) extracted is paramount for successful library preparation and sequencing. The following protocol is adapted for bacterial cultures and environmental samples typical in AMR resistome studies [50] [51].
Protocol: DNA Extraction Using Silica-Membrane Technology
- Objective: To obtain high-quality, high-molecular-weight gDNA from complex microbial communities, preserving both chromosomal and plasmid-borne AMR genes.
- Sample Input: Bacterial pellet from 1-5 mL of culture (for pure cultures) or concentrated biomass from environmental/clinical samples (e.g., water, soil, stool).
Reagents & Equipment:
- Lysis buffer (e.g., containing Tris-HCl, EDTA, SDS)
- Proteinase K
- RNase A
- Ethanol (96-100%)
- Silica-membrane spin columns (e.g., DNeasy Blood & Tissue Kit)
- Collection tubes (2 mL)
- Microcentrifuge
- Water bath or incubator (56°C)
- Elution buffer (10 mM Tris-HCl, pH 8.5)
Step-by-Step Procedure:
- Cell Lysis: Resuspend the pellet in the lysis buffer. Add Proteinase K and mix thoroughly by vortexing. Incubate at 56°C for 30-60 minutes or until the sample is completely lysed.
- RNase Treatment: Add RNase A and incubate at room temperature for 5 minutes.
- Conditioning: Add ethanol to the lysate and mix thoroughly by vortexing.
- Binding: Transfer the mixture to the silica-membrane spin column. Centrifuge at ≥6000 × g for 1 minute. Discard the flow-through.
- Washing: Add the provided wash buffer to the column. Centrifuge at ≥6000 × g for 1 minute. Discard the flow-through. Repeat this step with a second wash buffer if provided.
- Drying: Centrifuge the empty column for 1-2 minutes to remove residual ethanol.
- Elution: Place the column in a clean 1.5 mL microcentrifuge tube. Apply 50-200 µL of pre-warmed elution buffer directly onto the center of the membrane. Incubate for 5 minutes at room temperature. Centrifuge at ≥6000 × g for 1 minute to elute the pure gDNA.
- Quality Control: Assess DNA concentration using a fluorometric method (e.g., Qubit). Evaluate DNA integrity and fragment size distribution using a Fragment Analyzer or agarose gel electrophoresis. The optimal 260/280 ratio is ~1.8.
Special Consideration for Plasmid Reconstruction: For studies focusing on plasmid-borne AMR gene transfer, a plasmid-specific DNA extraction is recommended, although it may be less effective for large plasmids (>150 kb). Alternatively, using whole-genome DNA extraction followed by hybrid sequencing (short- and long-reads) has been shown to provide the most complete plasmid reconstruction [51].
Library Preparation Protocols
Library preparation converts the purified gDNA into a format compatible with the sequencing platform. The choice between fragmentation-based and tagmentation-based methods depends on DNA input and application needs [50] [52].
Protocol A: TruSeq Nano DNA Library Prep (Fragmentation-Based)
- Principle: This protocol uses acoustic shearing for unbiased DNA fragmentation, followed by end-repair, adapter ligation, and PCR enrichment [50].
- Best For: Applications requiring high sequencing uniformity, such as SNP calling and quantitative AMR gene analysis.
- Input: 1-4 μg of high-quality gDNA.
- Procedure Summary:
- Fragmentation: Dilute gDNA and fragment using adaptive focused acoustics (Covaris) to a target size of 350-550 bp.
- End-Repair: Convert the overhangs resulting from fragmentation into blunt ends using a proprietary enzyme mix.
- Adenylation: Add a single 'A' nucleotide to the 3' ends of the blunt fragments to prevent self-ligation.
- Adapter Ligation: Ligate indexing adapters containing a single 'T' nucleotide overhang to the 'A'-tailed DNA fragments.
- Purification: Clean up the ligation product using magnetic beads.
- PCR Enrichment: Amplify the adapter-ligated DNA using a PCR program to enrich for DNA fragments with correctly bound adapters on both ends.
- Notes: This method is robust but requires a high amount of input DNA, which can be a limitation for low-biomass samples [50].
Protocol B: Nextera XT DNA Library Prep (Tagmentation-Based)
- Principle: This protocol uses a transposase enzyme to simultaneously fragment and tag ("tagment") DNA with adapter sequences in a single reaction [50].
- Best For: Rapid preparation of multiple libraries from low DNA input, ideal for high-throughput AMR surveillance.
- Input: As low as 1 ng of gDNA.
- Procedure Summary:
- Tagmentation: Incubate gDNA with the bead-linked transposome. The transposase fragments the DNA and inserts adapter sequences simultaneously.
- Neutralization: Add a neutralizing tagment buffer to stop the reaction.
- PCR Amplification: Amplify the tagmented DNA using limited-cycle PCR. This step also adds unique index sequences (barcodes) to each sample for multiplexing.
- Purification: Clean up the final library using magnetic beads.
- Notes: While fast and requiring low input, tagmentation can be sensitive to the transposase-to-DNA ratio and may exhibit some sequence bias [50] [52].
Sequencing Platform Operation
The choice of sequencing platform dictates the read length and data type, which is critical for de novo assembly and resolving complex AMR gene contexts [50] [51].
Protocol: Sequencing on Illumina MiSeq and Oxford Nanopore Platforms
- Objective: To generate high-fidelity sequence data for metagenomic assembly and AMR gene profiling.
Table 1: Key Specifications and Protocols for Sequencing Platforms
| Parameter | Illumina MiSeq | Oxford Nanopore Technologies |
|---|---|---|
| Read Type | Short-read (paired-end) | Long-read (single-molecule) |
| Typical Run Output | 15 Gb | 10-30 Gb (MinION) |
| Typical Read Length | 2 × 250 bp | >10,000 bp (N50) |
| Primary AMR Application | High-accuracy AMR gene detection and SNP identification | Resolving mobile genetic elements (plasmids, transposons) and structural variants |
| Library Loading | Denature and dilute the final library according to the MiSeq System Guide. Load at a specified pmol concentration. | Prepare the flow cell by priming with flush buffers. Load the prepared library onto the SpotON sample port. |
| Run Setup | Select the appropriate reagent kit (e.g., MiSeq Reagent Kit v3, 600-cycle) and input the sample sheet with index sequences. | Initiate the sequencing run via the MinKNOW software, which manages data acquisition in real-time. |
| Data Output | Binary Base Call (BCL) files are automatically converted to FASTQ after the run. | FAST5 or POD5 files containing raw signal data, which are basecalled in real-time or post-run to FASTQ. |
- Quality Control Post-Run:
- Illumina: Assess sequencing quality metrics using FastQC, including Q-score distribution (>Q30 is excellent) and adapter content.
- Nanopore: Evaluate read quality (average Q-score) and read length distribution (N50) using NanoPlot.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Kits for mNGS-based AMR Workflows
| Item | Function in Workflow | Example Product(s) |
|---|---|---|
| DNA Extraction Kit | Isolation of high-molecular-weight genomic and plasmid DNA from complex samples. | DNeasy Blood & Tissue Kit, ChargeSwitch gDNA Mini Bacteria Kit, Easy-DNA Kit [50] |
| Library Prep Kit | Preparation of sequencing-ready libraries from gDNA. | Nextera XT DNA Library Prep Kit, TruSeq Nano DNA Library Prep Kit [50] |
| Targeted AMR Panels | Enrichment of specific AMR genes and pathogens from complex samples. | AmpliSeq for Illumina Antimicrobial Resistance Panel, Respiratory Pathogen ID/AMR Enrichment Panel [41] |
| Sequencing Reagents | Chemistry for performing the sequencing run on the respective platform. | MiSeq Reagent Kits, Nanopore Flow Cells (MinION, Flongle) [50] [51] |
| Validation Control | Certified reference material for validating AMR gene detection pipelines. | Used in proficiency tests (e.g., GMI PT) and for validating tools like abritAMR [50] [49] |
Technology Selection Guide for AMR Applications
The optimal combination of wet-lab methods depends on the specific research question. The decision tree below guides the selection of the most appropriate workflow.
Diagram 2: Technology Selection Guide for AMR Research Questions. This decision tree links the primary research objective to the most suitable wet-lab workflow. For instance, the hybrid sequencing approach is critical for understanding the horizontal transfer of AMR genes via plasmids, a key mechanism in the global spread of resistance [51].
A meticulously executed wet-lab workflow, from DNA extraction through sequencing, is the bedrock of reliable and insightful metagenomic analysis of antimicrobial resistance. The protocols and guidelines provided here are designed to empower researchers to generate data that can accurately reconstruct AMR gene contexts, distinguish chromosomal from mobile determinants, and ultimately contribute to effective AMR surveillance and risk assessment. As the field progresses towards standardized, ISO-certified genomic workflows [49], the robustness of these initial wet-lab steps will remain paramount.
The rapid and precise identification of pathogen transmission routes and the characterization of emerging variants are critical components of effective public health responses to infectious disease outbreaks. Conventional diagnostic methods, such as culture and targeted molecular assays, are often limited by prolonged turnaround times, the inability to detect novel or co-infecting pathogens, and poor performance with non-culturable or fastidious organisms [31] [1]. Metagenomic Next-Generation Sequencing (mNGS) has emerged as a transformative, hypothesis-free tool that enables simultaneous detection of a broad array of pathogens—including bacteria, viruses, fungi, and parasites—directly from clinical specimens [31] [1]. This application note details the use of mNGS for tracking transmission routes and variants of concern (VOCs) within the broader context of a research thesis focused on analyzing antimicrobial resistance (AMR) genes. By providing detailed protocols and data frameworks, this document serves as a guide for researchers, scientists, and drug development professionals engaged in genomic epidemiology and antimicrobial resistance surveillance.
mNGS Applications in Outbreak Management
Tracking Antimicrobial Resistance (AMR) Transmission
The genotypic characterization of AMR is a paramount application of mNGS in clinical outbreaks. Unlike phenotypic susceptibility testing, which can be slow and is limited to cultivable bacteria, mNGS can simultaneously identify pathogenic species and their associated resistance genes directly from complex samples, providing invaluable data for infection control and antimicrobial stewardship [53] [9].
Key Applications:
- Outbreak Response: Sequencing enables the tracking of transmission routes and monitoring of variants of concern during outbreaks. For instance, screening bacterial genomes from healthcare-associated infections has demonstrated the in-hospital transfer of genetic elements conferring multidrug resistance [41].
- Resistome Monitoring: Metagenomic sequencing allows for the real-time detection of plasmid-mediated resistance genes (e.g., mcr-1, blaNDM-5) that often evade routine phenotypic methods [31] [1]. This is crucial for surveilling the horizontal gene transfer of resistance determinants within bacterial populations.
- Global Surveillance: International initiatives like the Global Antimicrobial Resistance Surveillance System (GLASS) and the 100K Pathogen Genome Project leverage NGS to monitor AMR trends and the global spread of multidrug-resistant clones [31] [1].
The table below summarizes the quantitative outcomes of large-scale, real-world mNGS trials that have demonstrated its utility in clinical diagnostics and outbreak settings.
Table 1: Outcomes from Large-Scale mNGS Implementation Trials
| Trial Name | Key Findings and Diagnostic Impact | Context/Setting |
|---|---|---|
| MATESHIP | Provided real-world evidence for mNGS utility in pathogen detection and AMR profiling. | Large-scale clinical trial [31] [1] |
| GRAIDS | Demonstrated high diagnostic yield and capability for identifying rare/novel pathogens. | Large-scale clinical trial [31] [1] |
| DISQVER | Illustrated the role of mNGS in enhancing diagnostic accuracy in complex cases. | Large-scale clinical trial [31] [1] |
| NGS-CAP | Contributed to evidence base for integrating NGS into standard clinical practice. | Large-scale clinical trial [31] [1] |
| Central Nervous System (CNS) Infections | mNGS demonstrated a diagnostic yield as high as 63%, compared to <30% for conventional approaches [31] [1]. | Clinical diagnostics |
Characterizing SARS-CoV-2 Variants of Concern
The COVID-19 pandemic underscored the critical importance of genomic surveillance in tracking the evolution and spread of VOCs. VOCs are characterized by mutations that can confer increased transmissibility, immune evasion, and altered virulence [54] [55].
Defining Variants of Concern (VOCs): VOCs are SARS-CoV-2 variants with demonstrated increases in transmissibility, detrimental changes in COVID-19 epidemiology, increased virulence, or decreased effectiveness of public health measures, diagnostics, vaccines, or therapeutics [55]. The World Health Organization (WHO) and other national public health agencies continuously monitor and designate VOCs, such as Alpha (B.1.1.7), Delta (B.1.617.2), and Omicron (B.1.1.529) with its sublineages [54] [55].
Role of mNGS: mNGS and whole-genome sequencing (WGS) were pivotal in identifying the specific mutation profiles of these VOCs. For example, the Omicron variant is defined by over 15 spike protein receptor-binding domain mutations, which explain its significant ability to escape neutralizing antibodies from vaccination or prior infection [54]. The table below summarizes the biological properties of major SARS-CoV-2 VOCs that were characterized using genomic sequencing.
Table 2: Characteristics of Major SARS-CoV-2 Variants of Concern (VOCs)
| Variant (Pango Lineage) | Key Spike Protein Mutations | Impact on Virus Biology |
|---|---|---|
| Alpha (B.1.1.7) | N501Y, P681H | ~65% higher relative transmissibility; optimized furin cleavage [54] |
| Delta (B.1.617.2) | L452R, T478K, P681R | ~55% higher relative transmissibility; enhanced fusogenicity and replication [54] |
| Omicron (B.1.1.529) | G339D, S371L, S373P, S375F, K417N, N440K, S477N, T478K, E484A, Q493R, G496S, Q498R, N501Y, Y505H | Significant immune escape; altered cellular tropism with reduced lung infection [54] |
Experimental Protocols for Outbreak Sequencing
Sample Processing and Library Preparation
Principle: The goal is to extract all nucleic acids (DNA and/or RNA) from a clinical sample, convert them into a sequencing-ready library, and maximize the signal from microbial pathogens while minimizing host-derived nucleic acids [31] [1].
Detailed Protocol:
- Nucleic Acid Extraction:
- Use a bead-beating or enzymatic lysis method suitable for a broad range of pathogens (bacteria, viruses, fungi).
- For swabs, tissue, or sputum, use enzymatic pre-treatment (e.g., with mucolytics) to improve yield.
- Extract both DNA and RNA. For RNA viruses (e.g., SARS-CoV-2), include a reverse transcription step to generate cDNA.
Host Depletion (Critical for low-biomass samples):
- To increase the sensitivity for pathogen detection, selectively deplete abundant host (human) DNA.
- Methods: Use commercial kits employing probes that hybridize to human DNA followed by nuclease digestion, or saponin-based treatment to selectively lyse human cells without damaging microbial cell walls [31] [1].
Library Preparation:
- Fragment the DNA/cDNA to a desired size (e.g., 200-500 bp). This can be done enzymatically or via ultrasonication.
- Repair DNA ends and ligate platform-specific sequencing adapters. For Illumina platforms, this often involves indexing (barcoding) samples to enable multiplexing.
- Amplify the library via limited-cycle PCR to generate sufficient material for sequencing.
- Purify the final library and quantify using fluorometric methods (e.g., Qubit) and qualitative sizing (e.g., Bioanalyzer).
Metagenomic Sequencing
Principle: Sequence all nucleic acids in the prepared library in a high-throughput, parallel manner to generate millions of short reads representing the metagenomic content of the sample.
Detailed Protocol:
- Platform Selection:
- Illumina (Short-Read): Offers high accuracy and depth, ideal for detecting single nucleotide variants (SNVs) and low-frequency pathogens. Systems like MiSeq or NextSeq are commonly used [41] [53].
- Oxford Nanopore Technologies (ONT - Long-Read): Provides long read lengths, portability (MinION), and real-time sequencing, enabling rapid outbreak response in field settings [31] [1]. The trade-off is a higher raw read error rate compared to Illumina.
- Sequencing Run:
- Pool multiplexed libraries according to manufacturer guidelines.
- Load the pool onto the sequencing cartridge or flow cell.
- Execute the sequencing run. For ONT, base calling can be performed in real-time.
Bioinformatic Analysis for Pathogen and VOC Identification
Principle: The raw sequencing reads are processed through a bioinformatics pipeline to identify pathogens, determine their abundance, and characterize genetic features like mutations and AMR genes.
Detailed Protocol:
- Quality Control and Pre-processing:
- Use tools like FastQC to assess read quality.
- Trim adapters and low-quality bases using Trimmomatic or Cutadapt.
Host Read Removal:
- Align reads to the human reference genome (e.g., GRCh38) using a rapid aligner like Bowtie2 or BWA.
- Discard reads that map to the host genome to enrich for microbial data.
Taxonomic Classification:
- Assembly-based approach: De novo assemble quality-filtered, host-depleted reads into contigs using assemblers like SPAdes or MEGAHIT. Then, annotate contigs using tools like Prokka or by blasting against public databases (NR, NT).
- Read-based approach: Directly classify reads against comprehensive microbial databases using tools such as Kraken2 or Centrifuge. This is faster and useful for quick pathogen identification.
Variant Calling and Lineage Assignment (for Viruses like SARS-CoV-2):
- Map reads to a reference genome (e.g., Wuhan-Hu-1 for SARS-CoV-2) using Bowtie2 or BWA.
- Call variants (SNVs, indels) using tools like iVar or LoFreq.
- Assign a phylogenetic lineage (e.g., Pango lineage) based on the mutation profile using tools like Pangolin.
AMR Gene Detection:
- Use specialized tools to map reads or assembled contigs against curated AMR databases.
- Common Tools: ResFinder, ARIBA, RGI (Resistance Gene Identifier) from the Comprehensive Antibiotic Resistance Database (CARD) [53] [47].
- Output: A report detailing the detected AMR genes, their predicted resistance phenotypes, and genomic context (e.g., plasmid-borne).
The following diagram illustrates the complete end-to-end workflow for mNGS in outbreak settings, from sample to answer.
Validation and Benchmarking
To ensure the accuracy and reliability of mNGS for outbreak investigations, rigorous benchmarking against gold-standard datasets is essential.
Benchmarking Datasets:
- Publicly available, curated genomic and simulated metagenomic datasets, such as those generated by the Public Health Alliance for Genomic Epidemiology (PHA4GE), provide a "gold standard" for validating AMR detection pipelines [47]. These datasets contain raw sequencing reads from 174 clinically relevant bacterial pathogens, accompanied by validated AMR gene annotations.
Validation Protocol:
- Process the benchmarking dataset through your established mNGS and bioinformatics workflow.
- Compare the AMR genes and variants identified by your pipeline against the validated annotations provided with the dataset.
- Calculate performance metrics such as sensitivity, specificity, and precision to identify potential weaknesses or biases in your workflow.
- Use this analysis to refine and optimize bioinformatic parameters and database choices.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents, tools, and databases essential for successfully implementing the protocols described in this application note.
Table 3: Essential Research Reagents and Resources for mNGS Outbreak Analysis
| Item Name | Function / Application | Specific Examples / Notes |
|---|---|---|
| Host Depletion Kits | Selective removal of human DNA to improve microbial detection sensitivity. | Commercial kits using probe-hybridization or saponin-based methods [31]. |
| Broad-Range Nucleic Acid Extraction Kits | Simultaneous extraction of DNA and RNA from diverse pathogens in clinical samples. | Kits designed for tough-to-lyse organisms (e.g., mycobacteria, spores) are advantageous. |
| Targeted Enrichment Panels | Focused sequencing of predefined pathogen and AMR gene targets for increased sensitivity. | Illumina Respiratory Pathogen ID/AMR Panel; Urinary Pathogen ID/AMR Panel [41]. |
| Comprehensive Antibiotic Resistance Database (CARD) | Curated database of resistance genes, mutants, and associated phenotypes. | Used by tools like RGI for predicting AMR from sequence data [53] [47]. |
| ResFinder | Web/standalone tool for detecting acquired antimicrobial resistance genes. | Often used in tandem with PointFinder for chromosomal mutation detection [53]. |
| Pangolin (Phylogenetic Assignment of Named Global Outbreak Lineages) | Tool for assigning SARS-CoV-2 genome sequences to phylogenetic lineages. | Critical for tracking the spread of VOCs [55]. |
| ARIBA (Antimicrobial Resistance Identification By Assembly) | Tool for rapid resistance genotyping directly from sequencing reads. | Uses curated public databases (e.g., CARD, ResFinder) for fast results [53]. |
| Gold-Standard Benchmarking Datasets | Validated sequence datasets for benchmarking and validating AMR detection pipelines. | PHA4GE/JPIAMR genomic and simulated metagenomic datasets [47]. |
Metagenomic NGS represents a powerful and versatile platform for addressing the dual challenges of tracking pathogen transmission and characterizing variants of concern in clinical outbreaks. Its ability to provide hypothesis-free, genomic-level data directly from clinical samples enables a depth of analysis far beyond conventional methods. For AMR research, it offers a comprehensive view of the resistome, uncovering transmission networks of resistant clones and mobile genetic elements. For viral threats like SARS-CoV-2, it is the foundational technology for identifying and tracking the global spread of VOCs. As sequencing technologies continue to evolve towards greater speed, accuracy, and portability, and as bioinformatic tools and databases become more standardized, the integration of mNGS into routine public health and clinical practice will be indispensable for guiding effective interventions, informing antimicrobial stewardship, and mitigating the impact of future infectious disease outbreaks.
Antimicrobial resistance (AMR) is projected to cause up to 10 million deaths annually by 2050, representing one of the most pressing global health threats of the 21st century [56] [57]. Environmental surveillance of antibiotic resistance genes (ARGs) through metagenomic next-generation sequencing (mNGS) provides critical insights into resistance patterns, dissemination pathways, and emerging threats within complex microbial ecosystems [56] [1]. Wastewater treatment plants (WWTPs) and agricultural soils represent crucial interception points for monitoring ARG flow at the human-environment interface [57] [58]. This application note details standardized protocols for tracking ARG dynamics within these environments, enabling researchers to establish comprehensive AMR surveillance frameworks aligned with One Health principles that integrate human, animal, and environmental monitoring [56] [59].
The application of mNGS in environmental AMR surveillance allows for culture-independent, hypothesis-free detection of resistance determinants, including novel ARGs, those carried on mobile genetic elements (MGEs), and genes associated with specific pathogens [56] [1]. This approach has revealed that WWTPs serve as significant reservoirs and dissemination points for ARGs, where emerging contaminants (ECs) such as pharmaceuticals, heavy metals, and microplastics exert selective pressure that drives AMR development through co-selection mechanisms [57]. Similarly, land-use changes from forest to pastureland have been shown to significantly alter soil bacterial composition and select for specific ARG profiles in agricultural settings [60].
Quantitative ARG Profiles Across Environmental Matrices
ARG Abundance in Wastewater Treatment Systems
Table 1: Dominant ARG Classes and Their Relative Abundance in WWTPs
| ARG Class | Target Antibiotics | Most Prevalent Genes | Relative Abundance in Influent | Removal Efficiency by Biological Filters |
|---|---|---|---|---|
| Sulfonamide | Sulfamethoxazole, Sulfisoxazole | sul1, sul2 | 8.2-9.1 log10 copies/L [57] | 1.5-2.5 log reduction [58] |
| Tetracycline | Tetracycline, Doxycycline | tet(A), tet(O), tet(W) | 7.8-8.7 log10 copies/L [57] | 1.2-2.1 log reduction [58] |
| Macrolide-Lincosamide-Streptogramin (MLS) | Erythromycin, Azithromycin | erm(B), erm(F), mph(A) | 7.1-7.9 log10 copies/L [58] | 1.0-1.8 log reduction [58] |
| Beta-lactam | Penicillins, Cephalosporins | blaTEM, blaCTX-M, blaKPC | 6.5-7.3 log10 copies/L [61] | 0.8-1.5 log reduction [58] |
National-scale surveillance of 47 WWTPs across Wales demonstrated that biological filter beds achieved superior ARG removal compared to activated sludge processes, with significantly greater reductions in sul1, tet(O), and erm(B) genes [58]. The abundance and composition of the influent resistome directly correlated with catchment population size and density, highlighting the utility of wastewater surveillance for community-level AMR monitoring [56] [58].
ARG Distribution in Agricultural and Natural Soils
Table 2: ARG Profiles Across Land-Use Types in Amazonian Agroecosystems
| Land Use Type | Dominant Bacterial Species | Most Abundant ARG Classes | Notable ARG Patterns | Transposable Element Abundance |
|---|---|---|---|---|
| Native Forest | Diverse native microbiota | Aminoglycosides, Glycopeptides | Lower overall ARG abundance | Baseline levels [60] |
| Pasture (Fertilized) | Staphylococcus aureus, Bacillus coagulans | Macrolides, Tetracyclines | 2.3x increase in tet(W) vs forest | Moderate increase [60] |
| Pasture (Unfertilized) | Staphylococcus cohnii, Aeromonas spp. | Aminoglycosides, Sulfonamides | 1.8x increase in sul1 vs forest | Significant increase (p<0.05) [60] |
Metagenomic analysis of Amazonian soils revealed that conversion from forest to pastureland significantly altered bacterial community composition and selected for distinct ARG profiles, with fertilized pastures showing higher abundance of macrolide and tetracycline resistance genes, while unfed pastures exhibited increased sulfonamide resistance and transposable elements [60]. These findings demonstrate how agricultural management practices can shape the soil resistome and potentially facilitate ARG dissemination through enhanced mobility.
Advanced Methodologies for Environmental ARG Detection
Sample Processing and Nucleic Acid Extraction
Wastewater Sampling Protocol:
- Collect 24-hour composite samples from influent streams using automated refrigerated samplers (1-L aliquots every 30 minutes) [58]
- For grab sampling, collect 500 mL mid-stream during peak flow periods (8-10 AM)
- Process samples within 24 hours; store at 4°C during collection and at -80°C for long-term preservation
- Concentrate microbial biomass via centrifugation (10,000 × g, 30 minutes) or filtration (0.22-μm polyethersulfone membranes) [56]
Soil Sampling Protocol:
- Collect composite samples from topsoil (0-15 cm depth) using sterile corers following a zigzag pattern across the sampling area [60]
- Pool 5-10 subsamples per composite sample; homogenize thoroughly by sieving (2-mm mesh)
- Remove visible organic debris and stones prior to DNA extraction
- Store at -80°C in sterile 50-mL Falcon tubes for molecular analysis [60]
Nucleic Acid Extraction:
- Utilize commercial kits: DNeasy PowerSoil Kit (Qiagen) for soil samples [60] and DNeasy PowerWater Kit (Qiagen) for wastewater concentrates [16]
- Include extraction controls to monitor potential contamination
- Assess DNA quality via Nanodrop spectrophotometry (A260/A280 ratio of 1.8-2.0) [60]
- Verify DNA integrity through 1% agarose gel electrophoresis; require concentrations >50 ng/μL for sequencing library preparation [60]
Metagenomic Sequencing and Bioinformatics Analysis
Library Preparation and Sequencing:
- Utilize Illumina Nextera XT DNA Library Preparation Kit with 2 × 150 bp paired-end sequencing on Illumina NextSeq 550 platform [60]
- For enhanced ARG detection, implement CRISPR-Cas9-enriched NGS: design guide RNAs targeting clinically relevant ARGs (e.g., blaKPC, mecA, vanA) to enrich low-abundance targets prior to library preparation [61]
- Sequence to minimum depth of 10 million reads per sample for adequate resistome coverage [56]
Bioinformatic Processing Pipeline:
- Quality filter raw reads using FASTP to remove adapters and low-quality sequences (Q-score <20) [16]
- Perform de novo assembly with MEGAHIT using k-mer sizes 21-149 [16]
- Predict open reading frames (ORFs) using Prodigal [16]
- Create non-redundant gene catalog with CD-HIT (98% identity, 90% coverage) [16]
- Annotate ARGs using deepARG with E-value cutoff of ≤1e-5 [16]
- Normalize gene abundance to transcripts per million (TPM) for cross-sample comparisons [16]
- For advanced analysis: perform metagenomic binning with MetaWRAP, evaluate bin quality with CheckM (>50% completeness, <10% contamination) [16]
CRISPR-Enhanced ARG Detection Methodology
Recent advances in CRISPR-Cas9-modified NGS demonstrate significantly improved detection sensitivity for low-abundance ARGs in complex environmental samples [61]. This protocol enhancement enables researchers to detect clinically important ARGs that conventional metagenomics might miss.
CRISPR Enrichment Protocol:
- Design guide RNAs targeting ARG sequences of interest from curated databases (CARD, deepARG)
- Fragment genomic DNA (500 ng/sample) to 300-500 bp via ultrasonication
- Prepare sequencing libraries using Illumina-compatible adapters
- Hybridize guide RNA-Cas9 complexes to target ARGs (incubate 37°C, 60 minutes)
- Capture and amplify enriched targets using magnetic bead purification
- Sequence enriched libraries alongside conventional metagenomic libraries for comparative analysis
Performance Metrics:
- Detects up to 1,189 additional ARGs compared to conventional NGS [61]
- Lowers detection limit from 10⁻⁴ to 10⁻⁵ relative abundance [61]
- Identifies 61 additional ARG families in low abundances [61]
- Maintains low false negative (2/1208) and false positive (1/1208) rates [61]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Environmental AMR Surveillance
| Reagent/Material | Manufacturer/Supplier | Function | Application Notes |
|---|---|---|---|
| DNeasy PowerSoil Kit | Qiagen | Inhibitor-free DNA extraction from soil/compost | Critical for humic acid removal; enables PCR-amplifiable DNA from complex matrices [60] |
| DNeasy PowerWater Kit | Qiagen | DNA extraction from wastewater filters | Optimized for low-biomass water samples; improves yield from 0.22-μm filters [16] |
| Nextera XT DNA Library Prep Kit | Illumina | Metagenomic library preparation | Enables dual-index multiplexing for high-throughput sequencing [60] |
| Alt-R CRISPR-Cas9 System | Integrated DNA Technologies | ARG target enrichment | Guide RNA design for clinically relevant ARGs; enhances sensitivity 100-fold [61] |
| Illumina NextSeq 550 Reagents | Illumina | High-output sequencing | 2 × 150 bp configuration ideal for metagenomic assembly; 400M reads per flow cell [60] |
| MetaWRAP Pipeline | Open Source | Bioinformatic analysis | Modular pipeline for assembly, binning, and annotation; integrates multiple tools [16] |
| deepARG Database | Open Source | ARG annotation | Curated database with ARG sequences; E-value cutoff ≤1e-5 recommended [16] |
Data Interpretation and Integration into One Health Surveillance
Effective interpretation of environmental AMR data requires contextualization within the broader One Health framework that connects human, animal, and environmental reservoirs [56] [59]. Key analytical approaches include:
Resistome Risk Assessment:
- Apply tools such as MetaCompare to evaluate coexistence of ARGs, mobile genetic elements (MGEs), and human pathogens [16]
- Calculate risk indices based on ARG mobility, host pathogenicity, and clinical relevance
- Identify high-risk environments where intervention may be prioritized
Spatiotemporal Trend Analysis:
- Monitor ARG abundance shifts across seasons, land-use changes, or intervention periods
- Track emerging ARGs (e.g., mcr-1, blaNDM-5) of clinical concern [1]
- Correlate ARG profiles with environmental parameters (e.g., antibiotic residues, heavy metals, nutrient levels) [57]
Source Attribution Modeling:
- Employ compositional analysis to distinguish human versus agricultural ARG sources
- Identify ARG hotspots (WWTPs, hospitals, livestock operations) for targeted interventions [56]
- Model ARG dissemination pathways along the wastewater-environment continuum [58]
Integrating mNGS-based environmental surveillance with clinical AMR data creates a powerful early warning system for emerging resistance threats [56] [1]. This approach enables researchers to detect novel ARGs and mobile genetic elements in environmental reservoirs before they establish in clinical settings, informing proactive containment strategies and antimicrobial stewardship programs [56]. The standardized protocols presented in this application note provide a foundation for reproducible, comparable environmental AMR surveillance across diverse research settings and geographical regions.
Ventilator-associated pneumonia (VAP) represents a significant complication in critically ill patients, accounting for substantial mortality rates within intensive care units (ICUs) globally [62]. The polymicrobial nature and complex resistance patterns of VAP complicate treatment, highlighting the urgent need for rapid, accurate diagnostics that can identify pathogens and their antimicrobial resistance (AMR) profiles [62]. Traditional diagnostic methods, predominantly reliant on microbial cultures, are hampered by lengthy processing times and limited sensitivity, often leading to delayed or empirical treatment [62]. Within the broader context of metagenomic NGS research on AMR genes, this case study examines how targeted next-generation sequencing (tNGS) bridges the critical gap between comprehensive metagenomic approaches and the practical demands of clinical microbiology, offering a balanced solution for rapid AMR detection in critical care settings.
Results
Superior Diagnostic Performance of tNGS
In a recent study analyzing 199 patients with suspected VAP, tNGS demonstrated remarkable performance in pathogen identification, significantly outperforming traditional microbial culture methods [62]. The diagnostic performance metrics are summarized in Table 1.
Table 1: Diagnostic Performance Comparison Between tNGS and Microbial Culture for Pathogen Identification in VAP
| Diagnostic Method | Consistency Rate | Sensitivity Rate | Turnaround Time (Days) |
|---|---|---|---|
| tNGS | 98.49% (196/199) | 98.98% (194/196) | 1.66 (1.63-1.69) |
| Microbial Culture | 66.83% (133/199) | 66.84% (131/196) | 3.00 |
Beyond superior sensitivity, tNGS also demonstrated a significantly shorter turnaround time—nearly half that required for microbial culture (P < 0.05), enabling more timely therapeutic interventions [62]. Common pathogens identified in the VAP patients included Acinetobacter baumannii, Klebsiella pneumoniae, and Pseudomonas aeruginosa [62].
Antimicrobial Resistance Detection Accuracy
For AMR detection, the overall consistency between conventional antimicrobial susceptibility testing (AST) and tNGS was 79.31% across 99 samples analyzed [62]. The performance was particularly strong for specific pathogen-drug combinations, exhibiting excellent detection of carbapenem-penicillin-cephamycin resistance in Acinetobacter baumannii [62].
Comparative studies between different NGS approaches have revealed that capture-based tNGS demonstrates significantly higher diagnostic performance than both metagenomic NGS (mNGS) and amplification-based tNGS, with an accuracy of 93.17% and sensitivity of 99.43% when benchmarked against comprehensive clinical diagnosis [36].
Discussion
The findings from this case study align with broader research on genomic approaches for AMR, which highlight the transformative potential of sequencing technologies in understanding resistance mechanisms, determining transmission patterns, and guiding clinical decision-making [48]. tNGS occupies a crucial niche in this landscape, balancing the comprehensive scope of mNGS with the practical requirements of clinical microbiology—including cost-effectiveness, faster turnaround times, and enhanced sensitivity for targeted pathogens [36].
While genomic AST (gAST) shows significant promise, current limitations must be acknowledged. The technical complexity of gAST needs reduction, data management requires simplification, and clinical validity must be better defined through regulatory frameworks [14]. Furthermore, the detection of AMR genes does not always equate to phenotypic resistance, emphasizing the need for refined databases and interpretation algorithms [14]. For the foreseeable future, routine gAST implementation will likely require combination with rapid phenotypic AST to ensure complete accuracy [14].
Materials and Methods
Study Design and Population
This retrospective study enrolled adult patients (aged ≥18 years) admitted to the ICU of the First Hospital of Jilin University between May 2023 and March 2024 [62]. Eligibility criteria included: (1) sufficient lower respiratory tract samples; (2) results from microbial cultures; and (3) available clinical information [62]. Lower respiratory tract samples were collected within 12 hours of suspected VAP onset, with VAP defined as pneumonia occurring after receiving mechanical ventilation lasting ≥48 hours or within 48 hours of mechanical ventilation withdrawal [62]. Pneumonia diagnosis required at least one compatible symptom and new-onset radiological findings on chest images [62].
Sample Collection and Processing
Lower respiratory tract samples included bronchoalveolar lavage fluid (BALF) and sputum [62]. BALF samples were obtained exclusively from the middle segment, while sputum samples were collected from patients' first deep cough episodes in the early morning following mouth rinsing with sterile saline 2-3 times [62]. Samples were processed immediately for concurrent conventional microbiological tests and tNGS analysis.
Targeted Next-Generation Sequencing Workflow
Table 2: Research Reagent Solutions for tNGS Workflow in AMR Detection
| Reagent/Kit | Manufacturer | Function in Protocol |
|---|---|---|
| VAMNE Magnetic Pathogen DNA/RNA Extraction Kit | Vazyme, Nanjing, China | Co-extraction of DNA and RNA from samples |
| HieffNGSC37P4 OnePot cDNA & gDNA Library Prep Kit | Yeasen, Shanghai, China | cDNA synthesis and sequencing library preparation |
| GenePlus Target Capture Probes | GenePlus, Beijing, China | Enrichment of target pathogen and AMR gene sequences |
| One-Step DNB Preparation Kit | GenePlus, Beijing, China | Generation of DNA nanoballs for sequencing |
The detailed tNGS workflow proceeded as follows:
Nucleic Acid Extraction: A mixture of lysis buffer, protease K, and binding buffer was promptly added to samples within a grinding tube [62]. Mechanical lysis was performed for 30 seconds using a shock breaker [62]. DNA and RNA were co-extracted using the VAMNE Magnetic Pathogen DNA/RNA Extraction Kit per manufacturer's protocol [62].
Nucleic Acid Quantification: Extracted nucleic acids were accurately quantified using a Qubit 3.0 fluorometer with high sensitivity assay kits for both double-stranded DNA and RNA [62].
Library Preparation: Complementary DNA synthesis and sequencing library preparation were performed using the HieffNGSC37P4 OnePot cDNA & gDNA Library Prep Kit following manufacturer's protocols [62].
Target Enrichment: Enrichment of target sequences was conducted by incubating samples with GenePlus probes for approximately four hours, followed by amplification of captured products through an 18-cycle polymerase chain reaction (98°C 15s, 60°C 30s, 72°C 30s) [62].
Sequencing: Processed samples underwent sequencing on the Gene+Seq-100 platform with 100-bp single-end reads, aiming for a sequencing depth of 5 million reads to ensure comprehensive coverage [62].
Diagram 1: tNGS Workflow for AMR Detection. This diagram outlines the key steps in the targeted next-generation sequencing process for pathogen identification and antimicrobial resistance gene detection.
Bioinformatic Analysis
Sequencing data analysis utilized GenePlus's proprietary data analysis solution for initial processing [62]. This included:
- Removal of low-quality sequences, residual adapters, and short reads
- Filtering of microbial ribosomal RNA or human genomic material
- Alignment and annotation against comprehensive databases of pathogenic microorganisms and AMR genes using BLAST for sequence comparison
- Normalization of target reads on a reads per million (RPM) basis for quantitative analyses
- Application of blank control subtraction to minimize environmental or experimental contaminants
Clinically significant microbes were defined using established criteria to distinguish pathogens from background or contaminant signals [62].
Complementary AMR Analysis Frameworks
For researchers implementing tNGS for AMR detection, the Chan Zuckerberg ID (CZ ID) AMR module provides an open-access, cloud-based alternative for analyzing both microbial and AMR gene sequences from sequencing data [63]. This module leverages the Comprehensive Antibiotic Resistance Database (CARD) and Resistance Gene Identifier (RGI) software, enabling broad detection of both microbes and AMR genes from Illumina data [63]. The workflow incorporates two parallel approaches for AMR gene detection: (1) a "contig" approach where short reads are assembled into contiguous sequences using SPAdes before AMR gene detection, and (2) a "read" approach where short reads are directly analyzed for AMR genes [63].
This case study demonstrates that tNGS represents a significant advancement in the rapid diagnosis of VAP, offering superior sensitivity and faster turnaround times compared to conventional microbial cultures. The technology's ability to simultaneously identify pathogens and their AMR profiles makes it particularly valuable for managing critically ill patients, enhancing treatment precision, and supporting antimicrobial stewardship efforts in ICU settings. When framed within the broader thesis of metagenomic NGS research for AMR analysis, tNGS emerges as a balanced solution that maintains the genomic precision of mNGS while addressing clinical needs for speed, sensitivity, and practical implementation. As databases expand and bioinformatic tools become more refined, tNGS is poised to play an increasingly central role in the clinical microbiology landscape, ultimately contributing to improved patient outcomes in the face of the growing AMR threat.
Antimicrobial resistance (AMR) represents one of the most pressing public health crises of the 21st century, with antibiotic-resistant infections causing millions of deaths annually [1]. Urban freshwater lakes, particularly those experiencing eutrophication from anthropogenic activities, have emerged as significant reservoirs and mixing vessels for antibiotic resistance genes (ARGs) [64] [65]. The analysis of these environments using metagenomic next-generation sequencing (mNGS) provides powerful insights into the distribution, dynamics, and drivers of AMR within complex microbial communities. This case study explores the application of mNGS methodologies to investigate the interplay between eutrophication, microbial community structure, and resistome risk in urban lakes, framed within a broader thesis on analyzing AMR with metagenomic NGS research.
Eutrophic urban lakes are characterized by excessive nutrient inputs, often from agricultural runoff, sewage discharge, and other human activities. These conditions create environments where microbial communities undergo rapid shifts, influencing the proliferation and transfer of ARGs [65]. Understanding the internal links and external influences shaping these resistomes is crucial for ecological and human health risk assessment [65]. Metagenomic approaches enable researchers to move beyond culturable organisms to profile the entire genetic potential for resistance within these ecosystems, revealing previously overlooked connections between nutrient cycling, microbial metabolism, and resistance selection.
Key Findings from Metagenomic Studies
Trophic State and Resistome Risk
Comparative analyses of urban lakes across trophic gradients have revealed significant correlations between nutrient enrichment and AMR profiles. Hypereutrophic lakes consistently demonstrate elevated ARG levels despite reduced microbial diversity [65].
Table 1: Relationship between Trophic State and AMR Parameters in Urban Lakes
| Trophic State | Microbial Diversity | ARG Abundance | Dominant ARG Types | Resistome Risk Score |
|---|---|---|---|---|
| Hypereutrophic | Lowest | Highest | sul1, sul2, tetA, tetC | Highest |
| Eutrophic | Moderate | High | sul1, tetB, qnrD | High |
| Mesoeutrophic | High | Moderate | Varied, lower abundance | Moderate |
A study of six urban lakes in Wuhan, China, found that sul1 and sul2 genes dominated the resistome, accounting for 86.28-97.79% of total ARGs detected [64]. Similarly, tetracycline resistance genes encoding efflux pumps (tetA, tetB, tetC, tetG) showed higher relative abundance than those encoding ribosomal protection proteins (tetM, tetQ) [64]. The class I integron (intI1) was identified as a critical mediator for ARG propagation in these environments [64].
Co-selection with Heavy Metals and Environmental Drivers
Metagenomic analyses have revealed that co-selection with heavy metals represents a significant driver of AMR in urban lakes. Redundancy analysis and variation partitioning analysis demonstrated that antibiotics and heavy metals were the major factors governing ARG propagation [64]. The presence of metal resistance genes (MRGs) often correlated with ARG abundance, suggesting cross-resistance mechanisms where metal contamination directly selects for bacterial strains carrying both MRGs and ARGs [65].
Environmental parameters significantly influencing resistome profiles include:
- Nutrient concentrations (nitrate, nitrite, ammonia, orthophosphate)
- Dissolved organic carbon (DOC) content
- Lake morphology and water retention time
- Anthropogenic impact intensity in surrounding areas [64]
Heavily eutrophic lakes located in high-density building areas with substantial human activity exhibited the highest relative abundance of total ARGs [64].
Microbial Community Structure and ARG Hosts
Microbial community composition significantly influences resistome potential, with specific bacterial taxa identified as predominant ARG hosts. Metagenome-assembled genomes (MAGs) analysis has revealed that Aestuariivirga and Limnohabitans (Proteobacteria) serve as primary bacterial hosts of ARGs in urban lake environments [65]. Furthermore, studies have identified connections between microbial metabolic pathways and resistance selection, with vitamin B12 (VB12) synthesis pathways showing intriguing relationships with resistance trends [16].
Table 2: Key Bacterial Hosts of ARGs in Urban Lake Environments
| Bacterial Host | Phylum | ARG Types Carried | Ecological Role | Pathogenic Potential |
|---|---|---|---|---|
| Aestuariivirga | Proteobacteria | Multiple, including sulfonamide | Organic matter degradation | Low |
| Limnohabitans | Proteobacteria | Tetracycline, sulfonamide | Planktonic interactions | Low |
| Pathogenic MAGs | Various | Multiple drug classes | Various | High (≥4 MAGs identified) |
Binning analysis has confirmed that at least 26 MAGs actively participate in VB12 synthesis, with a minimum of 4 MAGs demonstrating both resistance during VB12 synthesis and pathogenicity [16]. This finding highlights the potential dual function of certain microorganisms in nutrient cycling and resistance dissemination.
Experimental Protocols
Sample Collection and Processing
Materials Required:
- DNeasy PowerWater Kit (QIAGEN) or equivalent
- Multi-parameter probe (e.g., WTW 3430) for in situ measurements
- Filtration apparatus with 0.22μm membranes
- Sterile sample containers
Protocol:
- Site Selection: Identify sampling points systematically distributed across the lake at intervals of 1-5 km, adjusted based on lake size [16].
- In Situ Measurements: Record dissolved oxygen (DO), electrical conductivity (EC), pH, and temperature using calibrated multi-parameter probes [16].
- Water Collection: Collect surface water samples (1-2L) in sterile containers, maintaining cold chain during transport.
- Filtration: Filter water samples through 0.22μm membranes to capture microbial biomass.
- Preservation: Either process samples immediately for DNA extraction or store at -80°C for future analysis.
DNA Extraction and Quality Control
Materials Required:
- DNeasy PowerWater Kit (QIAGEN)
- Qubit 3.0 fluorometer (Thermo Fisher Scientific)
- Agarose gel electrophoresis equipment
- Benzonase (Sigma) for host DNA depletion (optional)
Protocol:
- Extraction: Follow manufacturer's instructions for the DNeasy PowerWater Kit to extract genomic DNA from filtered biomass [16].
- Concentration Measurement: Assess DNA concentration and purity using Qubit 3.0 fluorometer [16] or equivalent.
- Quality Assessment: Verify DNA integrity via agarose gel electrophoresis or Bioanalyzer.
- Host Depletion: For samples with high host contamination, implement host DNA depletion using 1U of Benzonase and 0.5% Tween 20, followed by 5-minute incubation at 37°C [5].
Library Preparation and Sequencing
Materials Required:
- Illumina DNA Prep kit
- KAPA low throughput library construction kit
- Hybrid capture probes (e.g., SeqCap EZ Library, Roche)
- Illumina sequencing platform (e.g., HiSeq, NextSeq)
Protocol:
- Library Preparation: Use Illumina DNA Prep kit or KAPA low throughput library construction kit according to manufacturer's specifications [5].
- Library Quality Control: Assess library quality using Qubit dsDNA HS Assay kit followed by High Sensitivity DNA kit on an Agilent 2100 Bioanalyzer [5].
- Target Enrichment (Optional): For targeted resistance gene sequencing, use hybrid capture-based enrichment with microbial probes designed using pipelines like CATCH [5].
- Sequencing: Load library pools onto an Illumina platform for 75-150 cycle paired-end sequencing, generating approximately 20 million reads per library [5].
Bioinformatic Analysis
Materials Required:
- High-performance computing cluster
- Bioinformatics software (detailed in Section 5)
Protocol:
- Quality Control: Process raw sequencing reads with FASTP to eliminate low-quality reads and adapters [16].
- Human Read Removal: Align reads to human reference genome (e.g., hg38) and remove matching sequences [5].
- Assembly: Perform de novo assembly using MEGAHIT with k-mer sizes ranging from 21 to 149 [16].
- ORF Prediction: Predict open reading frames with Prodigal [16].
- Gene Cataloging: Generate non-redundant gene catalog using CD-HIT (98% identity, 90% coverage) [16].
- Functional Annotation:
- Binning and MAG Generation: Use MetaWRAP pipeline with MetaBAT2 for binning, followed by refinement and dereplication with dRep at 99% ANI [16].
- Taxonomic Classification: Classify MAGs using GTDB-Tk [16].
- Statistical Analysis: Perform PCoA, PERMANOVA, and correlation analyses using R packages.
Data Analysis Workflows
The analytical workflow for metagenomic AMR analysis involves multiple steps from raw data processing to ecological interpretation, as visualized below:
AMR Annotation Pipeline Comparison
Multiple tools and databases are available for AMR annotation, each with different strengths and coverage:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for Metagenomic AMR Studies
| Category | Product/Software | Specific Function | Application Note |
|---|---|---|---|
| DNA Extraction | DNeasy PowerWater Kit (QIAGEN) | Environmental DNA extraction | Optimal for low-biomass water samples [16] |
| Host Depletion | Benzonase (Sigma) | Degradation of host nucleic acids | Critical for clinical samples; use at 1U with 0.5% Tween 20 [5] |
| Library Prep | Illumina DNA Prep | Library construction | Compatible with diverse sample types [41] |
| Target Enrichment | SeqCap EZ Library (Roche) | Hybrid capture of target genes | Enables focused resistance gene sequencing [5] |
| Sequencing Platform | Illumina HiSeq/NextSeq | High-throughput sequencing | Standard for metagenomic studies [16] |
| Annotation Tool | AMRFinderPlus | Comprehensive AMR annotation | Includes genes and point mutations; NCBI-curated [66] |
| Annotation Tool | deepARG | ARG annotation | Sensitive detection of resistance genes [16] |
| Reference Database | CARD | Comprehensive ARG reference | Gold standard for resistance gene annotation [67] |
| Reference Database | VB12Path | Vitamin B12 synthesis genes | Specialized metabolic pathway database [16] |
| Assembly Tool | MEGAHIT | Metagenomic assembly | Efficient with variable community complexity [16] |
| Binning Tool | MetaBAT2 | Metagenomic binning | Groups contigs into MAGs [16] |
| Quality Control | CheckM | MAG quality assessment | Evaluates completeness and contamination [16] |
Discussion and Implementation Notes
Technical Considerations
The implementation of mNGS for AMR surveillance in eutrophic lakes presents several technical challenges that require careful consideration. Host DNA depletion is particularly critical when analyzing water samples with high eukaryotic content, as host sequences can dominate libraries and reduce microbial sequence recovery [1]. The use of internal controls, including DNA and RNA phages spiked at known concentrations (e.g., 10^4 copies/mL), enables quality monitoring throughout the sequencing workflow [5].
Database selection significantly impacts annotation completeness and accuracy. Comparative studies have demonstrated that different AMR databases (CARD, ResFinder, DeepARG) and annotation tools (AMRFinderPlus, Abricate, RGI) yield varying results due to differences in curation rules and content [67]. AMRFinderPlus, which utilizes NCBI's curated Reference Gene Database, provides comprehensive coverage of both resistance genes and point mutations [66]. For consistent results, researchers should select tools based on the specific resistance mechanisms of interest and maintain consistent tool-database combinations throughout a study.
Analytical Validation
When applying mNGS for AMR prediction, it is important to recognize that resistome profiling currently demonstrates variable performance compared to phenotypic susceptibility testing. Studies comparing mNGS detection of resistance genes with conventional phenotyping show particularly strong agreement for certain drug-pathogen combinations (e.g., 94.74% sensitivity for predicting carbapenem resistance in Acinetobacter baumannii), but lower performance for other antibiotics [5]. This underscores that while mNGS provides valuable insights into resistance genetic potential, it cannot yet replace conventional phenotypic testing for clinical decision-making [5].
For assessing ecological risk, tools like MetaCompare can evaluate resistome risk by estimating the coexistence of ARGs, mobile genetic elements (MGEs), and human pathogens [16]. This approach allows researchers to prioritize high-risk resistance configurations that have greater potential for transmission to pathogens.
Emerging Applications
The integration of long-read sequencing technologies from Oxford Nanopore and PacBio represents a promising advancement for AMR research in complex environments. These platforms enable nearly full-length 16S rRNA gene sequencing (~1,500 bp), facilitating more robust taxonomic classification at the species level [68]. The portability of devices like MinION further enables field-based sequencing, reducing sample handling biases and potentially accelerating analysis timelines [68] [1].
The application of machine learning approaches to predict resistance phenotypes from genomic features shows increasing promise. "Minimal models" built using known resistance determinants can identify antibiotics where existing knowledge adequately explains resistance patterns, highlighting areas where novel mechanism discovery is most needed [67]. For Klebsiella pneumoniae, a key pathogen in aquatic environments, such models have revealed significant gaps in current knowledge for certain antibiotic classes [67].
Metagenomic NGS approaches provide powerful tools for unraveling the complex dynamics of antimicrobial resistance in eutrophic urban lakes. The protocols and applications outlined in this document demonstrate how comprehensive resistome profiling can illuminate the connections between anthropogenic impact, eutrophication, and AMR emergence. By integrating sample processing, sequencing, bioinformatic analysis, and ecological interpretation, researchers can identify critical control points for intervention and monitor the effectiveness of management strategies aimed at reducing resistome risk in these vulnerable ecosystems.
As sequencing technologies continue to evolve and analytical methods become more sophisticated, metagenomic approaches will play an increasingly important role in both understanding AMR ecology and informing public health responses to this global threat. The frameworks presented here offer a foundation for standardized, reproducible resistome analysis that can be adapted to diverse aquatic environments and research questions.
Navigating the Challenges: Strategies to Optimize mNGS for AMR Detection
The detection and characterization of antimicrobial resistance (AMR) genes using metagenomic next-generation sequencing (mNGS) is fundamentally constrained by a pervasive technical hurdle: the overwhelming abundance of host DNA in clinical samples. Respiratory specimens such as bronchoalveolar lavage fluid (BALF) typically contain a microbe-to-host read ratio of approximately 1:5263, with host DNA content constituting up to 99% of the total sequenced nucleic acids in samples like nasopharyngeal aspirates [69] [70]. This host DNA dominance creates a low microbial biomass environment that severely limits sequencing efficiency, as the majority of sequencing reads and resources are expended on host genetic material rather than on microbial pathogens and their resistance genes. Consequently, the sensitivity for detecting low-abundance pathogens and their associated AMR markers is significantly compromised, potentially obscuring critical resistance patterns and leading to false negatives in clinical diagnostics [69] [1].
Overcoming this host DNA interference is particularly crucial for AMR surveillance, as it enables researchers to achieve the deeper microbial coverage necessary for comprehensive resistome profiling. Effective host depletion methods can increase microbial reads by 7.6 to 1,725.8-fold compared to non-depleted samples, dramatically improving the detection of antibiotic resistance genes (ARGs) and providing a more accurate representation of the resistance potential within microbial communities [70]. This application note provides a systematic evaluation of host DNA depletion strategies and detailed protocols optimized for profiling antimicrobial resistance genes in challenging clinical samples with low microbial biomass.
Comparative Performance of Host DNA Depletion Methods
Efficiency Metrics Across Depletion Techniques
The selection of an appropriate host DNA depletion method requires careful consideration of multiple performance metrics, including depletion efficiency, microbial DNA retention, and practical implementation factors. The table below summarizes the quantitative performance of seven pre-extraction host DNA depletion methods tested on respiratory samples, providing a comparative framework for method selection [69].
Table 1: Performance Comparison of Host DNA Depletion Methods for Respiratory Samples
| Method | Host DNA Removal Efficiency | Microbial Read Increase (Fold-Change) | Bacterial DNA Retention Rate | Key Limitations |
|---|---|---|---|---|
| S_ase (Saponin lysis + nuclease) | 99.99% (BALF) | 55.8× | Moderate | Diminishes some commensals/pathogens |
| K_zym (HostZERO Kit) | 99.99% (BALF) | 100.3× | Low to moderate | Commercial cost |
| F_ase (Filtering + nuclease) | ~99.9% | 65.6× | High | May lose cell-associated microbes |
| K_qia (QIAamp Microbiome Kit) | ~99.9% | 55.3× | 21% (OP samples) | Commercial cost |
| O_ase (Osmotic lysis + nuclease) | ~99.9% | 25.4× | Moderate | Variable efficiency |
| R_ase (Nuclease digestion only) | ~99% | 16.2× | 31% (BALF) | Less effective for intracellular DNA |
| O_pma (Osmotic lysis + PMA) | ~90% | 2.5× | Low | Least effective |
The Sase (saponin lysis with nuclease digestion) and Kzym (HostZERO Microbial DNA Kit) methods demonstrate the highest host DNA removal efficiency, reducing host DNA to approximately 0.01% of original concentrations in BALF samples [69]. However, the Fase method (filtering combined with nuclease digestion) developed more recently shows a balanced performance profile with high microbial read enhancement and potentially reduced taxonomic bias [69]. The Rase method (nuclease digestion alone) provides the highest bacterial DNA retention in BALF samples (median 31%) but offers more modest microbial read enrichment (16.2-fold), making it suitable for samples where maximizing microbial DNA recovery is prioritized [69].
Impact on Microbial Community Representation and AMR Profiling
All host depletion methods introduce some degree of taxonomic bias that must be considered for AMR research applications. Some commensals and pathogens, including Prevotella spp. and Mycoplasma pneumoniae, can be significantly diminished through certain depletion protocols [69]. These biases may potentially skew resistance gene profiles if the affected taxa represent important reservoirs of specific ARGs. The F_ase method demonstrates the most balanced performance across bacterial groups, making it particularly suitable for studies aiming to characterize comprehensive resistomes without significant taxonomic distortion [69].
For AMR surveillance, the dramatically increased microbial sequencing depth achieved through effective host depletion enables detection of low-abundance resistance genes that would otherwise be missed. In nasopharyngeal aspirates from premature infants, host depletion increased the number of bacterial reads by 7.6 to 1,725.8-fold, permitting resistome characterization despite initial host DNA content exceeding 99% [70]. This enhanced sensitivity is crucial for identifying emerging resistance threats and capturing the full diversity of resistance determinants within complex microbial communities.
Detailed Experimental Protocols for Host DNA Depletion
Optimized F_ase Protocol (Filter-Based Depletion)
The F_ase method represents a recently developed approach that combines physical separation via filtration with enzymatic degradation of host DNA, offering balanced performance with minimal special equipment requirements [69].
Table 2: Reagent List for F_ase Protocol
| Reagent/Material | Specification | Function in Protocol |
|---|---|---|
| Sterile PBS | pH 7.4, molecular biology grade | Sample dilution & washing |
| Syringe Filter Units | 10 μm pore size, low protein binding | Removal of host cells & debris |
| DNase I Enzyme | Molecular biology grade, RNase-free | Degradation of free host DNA |
| DNase Buffer | 10× concentration, with Mg²⁺ | Optimal enzyme activity |
| EDTA Solution | 0.5 M, pH 8.0 | Enzyme inactivation |
| Proteinase K | Molecular biology grade | Microbial cell lysis |
| Lysis Buffer | Contains SDS or similar detergent | Membrane disruption |
Step-by-Step Procedure:
Sample Preparation: Dilute 1-2 mL of fresh or preserved respiratory sample (BALF, sputum, or nasopharyngeal aspirate) with 3 volumes of sterile PBS. For cryopreserved samples, add 25% glycerol before storage and ensure complete thawing on ice before processing [69].
Filtration-Based Host Cell Removal:
- Pre-wet a 10 μm pore size syringe filter with 5 mL sterile PBS.
- Pass the diluted sample slowly through the filter using a syringe, collecting the filtrate in a sterile 15 mL tube.
- Wash the filter with 2-3 mL PBS and combine with the initial filtrate [69].
Host DNA Digestion:
- Add MgCl₂ to the filtrate to a final concentration of 5 mM.
- Add DNase I enzyme (5-10 U/mL final concentration).
- Incubate at 37°C for 30 minutes with gentle mixing [69].
Enzyme Inactivation and Microbial Lysis:
- Add EDTA to a final concentration of 10 mM to chelate Mg²⁺ and inactivate DNase.
- Concentrate microbial cells by centrifugation at 10,000 × g for 10 minutes.
- Resuspend pellet in 200 μL of lysis buffer containing Proteinase K.
- Incubate at 56°C for 1 hour to complete microbial lysis [69].
DNA Purification:
- Proceed with standard phenol-chloroform extraction or commercial DNA purification kits.
- For low biomass samples, consider concentrating the final eluate to 20-30 μL to increase DNA concentration [70].
Integrated MolYsis with MasterPure DNA Extraction Protocol
For particularly challenging low-biomass samples such as nasopharyngeal aspirates, the combination of MolYsis host depletion with MasterPure DNA extraction has demonstrated robust performance, increasing bacterial reads by up to 1,725.8-fold compared to non-depleted samples [70].
Step-by-Step Procedure:
MolYsis Host Depletion:
- Add 500 μL of clinical sample to MolYsis Binding Buffer in a DNA LoBind tube.
- Incubate at room temperature for 5 minutes to allow host cell binding.
- Centrifuge at 12,000 × g for 10 minutes to pellet host cells and debris.
- Transfer supernatant containing microbes to a new tube, avoiding disturbance of the pellet [70].
Microbial Concentration:
- Centrifuge the supernatant at 15,000 × g for 15 minutes to pellet microbial cells.
- Carefully remove and discard supernatant, leaving 20-30 μL to resuspend the microbial pellet [70].
MasterPure DNA Extraction:
- Add 300 μL of Tissue and Cell Lysis Solution containing 1 μL Proteinase K (50 μg/mL).
- Incubate at 65°C for 30 minutes with occasional vortexing to ensure complete lysis.
- Add 1 μL of RNase A (5 μg/mL) and incubate at 37°C for 30 minutes.
- Place samples on ice for 3-5 minutes to cool.
- Add 200 μL of MPC Protein Precipitation Reagent, vortex vigorously for 10 seconds.
- Centrifuge at 15,000 × g for 10 minutes to pellet proteins [70].
DNA Precipitation:
- Transfer supernatant to a new tube containing 500 μL of isopropanol.
- Mix by inversion and centrifuge at 15,000 × g for 10 minutes to pellet DNA.
- Wash DNA pellet with 70% ethanol and air dry for 5-10 minutes.
- Resuspend in 20-25 μL of TE Buffer or nuclease-free water [70].
Quality Control and Validation for AMR Studies
DNA Quality and Quantity Assessment
Rigorous quality control is essential for successful mNGS-based AMR studies, particularly when working with host-depleted low biomass samples. Digital droplet PCR (ddPCR) provides accurate quantification of the total 16S rRNA gene copy number, which serves as a reliable measure of total bacterial abundance in metagenomic DNA samples [71]. However, 16S rRNA copy number quantification is strongly affected by DNA quality, with a precise correlation between quantification underestimation and DNA degradation levels as measured by the DNA Integrity Number (DIN) [71]. For degraded metagenomic DNAs (DIN < 5), implement a mass correction factor based on the observed DIN value to prevent inaccurate quantification of 16S copy number [71].
Additional quality metrics should include:
- DNA Purity: Assess using A260/A280 and A260/A230 ratios on NanoDrop, with optimal ranges of 1.8-2.0 and 2.0-2.2 respectively [72].
- DNA Integrity: Evaluate using Agilent TapeStation or similar fragment analysis systems, with DIN > 7 indicating high-quality DNA suitable for mNGS [71].
- Host DNA Residual Quantification: Include qPCR assays targeting single-copy human genes (e.g., RNase P) to determine the efficiency of host depletion [70].
Contamination Control and Process Validation
Low microbial biomass samples are exceptionally vulnerable to contamination and technical artifacts. Implement the following controls to ensure results reliability:
Negative Controls: Include extraction blanks (reagents only) and process controls throughout the workflow to identify potential contamination sources [70].
Mock Communities: Utilize defined microbial mock communities (e.g., ZymoBIOMICS standards) spiked into sample matrices to validate both host depletion efficiency and taxonomic accuracy [69] [70].
Internal Standards: Add spike-in controls (e.g., non-human commensal bacteria or synthetic DNA sequences) before DNA extraction to monitor technical variation and normalize across samples [70].
Bioinformatic Filtering: Employ stringent post-sequencing filters to remove contaminants identified in negative controls, and utilize tools like Decontam (R package) for statistical identification of contaminant sequences [1].
Application to Antimicrobial Resistance Gene Profiling
Bioinformatics Pipeline for AMR Detection
Following successful host depletion and sequencing, implement a robust bioinformatic workflow specifically designed for comprehensive AMR gene detection:
Read Quality Control: Use FastP or Trimmomatic to remove adapters and low-quality sequences [16].
Host Read Removal: Align reads to human reference genome (hg38) using BWA or Bowtie2 and remove aligning reads [1].
Metagenomic Assembly: Perform de novo assembly using MEGAHIT or metaSPAdes with k-mer-based approaches [16].
ORF Prediction and Gene Cataloging: Predict open reading frames using Prodigal and create non-redundant gene catalogs with CD-HIT [16].
ARG Annotation: Align predicted genes against AMR databases (CARD, ARDB, DeepARG) using BLAST or DIAMOND with E-value ≤ 1e-5 [16] [8].
Mobile Genetic Element Detection: Screen for plasmids, integrons, and transposons using dedicated databases (mobileOG) to assess horizontal gene transfer potential [8].
Quantification and Normalization: Normalize ARG abundance to transcripts per million (TPM) or similar metrics to enable cross-sample comparisons [16].
Research Reagent Solutions for Host Depletion and AMR Studies
Table 3: Essential Research Reagents for Host DNA Depletion and AMR Analysis
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Commercial Host Depletion Kits | MolYsis Basic kit, QIAamp DNA Microbiome Kit, HostZERO Microbial DNA Kit | Integrated protocols for selective host DNA removal; optimal for standardized workflows [69] [70]. |
| DNA Extraction Kits (Low Biomass) | MasterPure Complete DNA & RNA Purification Kit, QIAamp PowerFecal Pro DNA Kit, Macherey Nucleospin Soil Kit | Effective lysis of Gram-positive bacteria; high yield from limited starting material [70] [72]. |
| Enzymatic Reagents | DNase I (RNase-free), Proteinase K, Lysozyme | Host DNA degradation (DNase I) and microbial cell wall lysis (Lysozyme, Proteinase K) [69]. |
| Microbial Standards | ZymoBIOMICS Microbial Community Standards, Spike-in Control II for Low Microbial Load | Process validation and quantification normalization [70]. |
| NGS Library Preparation | Illumina DNA Prep, NEBNext Ultra II DNA Library Prep | Efficient library construction from low-input DNA [41]. |
| Targeted Enrichment Panels | Respiratory Pathogen ID/AMR Enrichment Panel, AmpliSeq for Illumina Antimicrobial Resistance Panel | Focused sequencing of AMR genes and pathogens; cost-effective for high-throughput screening [41]. |
Effective host DNA depletion is not merely an optional optimization step but a fundamental requirement for comprehensive antimicrobial resistance gene profiling using metagenomic NGS in low microbial biomass clinical samples. The methods detailed in this application note, particularly the F_ase and MolYsis with MasterPure protocols, provide robust frameworks for significantly enhancing microbial sequencing depth and consequently improving ARG detection sensitivity. As the field advances, integration of these wet-lab methodologies with emerging computational approaches and long-read sequencing technologies will further transform our ability to monitor and understand the complex dynamics of antimicrobial resistance in clinical settings [1] [8].
Researchers should select host depletion strategies based on their specific sample types, biomass levels, and research objectives, recognizing that method choice involves trade-offs between depletion efficiency, microbial recovery, and taxonomic fidelity. Through systematic implementation of these optimized protocols and quality control measures, the scientific community can overcome the host DNA problem and unlock the full potential of metagenomic NGS for antimicrobial resistance surveillance and management.
In metagenomic next-generation sequencing (mNGS) research focused on antimicrobial resistance (AMR), the overwhelming abundance of host DNA in clinical samples presents a significant analytical challenge. This high background of host nucleic acids consumes sequencing resources and obscures microbial signals, thereby reducing the sensitivity for detecting low-abundance pathogens and their associated antibiotic resistance genes (ARGs) [69] [1]. Host depletion techniques have emerged as essential sample preparation strategies to mitigate this issue, with filtration- and enzymatic-based methods representing two prominent approaches. This Application Note provides a systematic evaluation of these techniques, presenting structured quantitative data, detailed experimental protocols, and practical workflows tailored for research on antimicrobial resistance genes using metagenomic sequencing.
Performance Comparison of Host Depletion Methods
Quantitative Metrics for Method Evaluation
The effectiveness of host depletion techniques is measured through multiple performance metrics, including host DNA removal efficiency, microbial DNA retention rate, and the subsequent enrichment of microbial reads in sequencing data. These parameters collectively determine the suitability of a method for sensitive AMR gene detection [69] [73].
Table 1: Comprehensive Performance Comparison of Host Depletion Methods for Respiratory Samples
| Method Category | Specific Method | Host DNA Removal Efficiency | Microbial DNA Retention | Microbial Read Enrichment (Fold Increase) | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Enzymatic | Saponin lysis + nuclease (S_ase) | 99.89% (BALF) [69] | Not specified | 55.8× (BALF) [69] | High host depletion efficiency | Potential taxonomic bias; diminishes some commensals/pathogens |
| Enzymatic | HostZERO Kit (K_zym) | 99.91% (BALF) [69] | Lower retention rate | 100.3× (BALF) [69] | Commercial standardization; high depletion | Lower bacterial retention |
| Filtration | 10μm filtering + nuclease (F_ase) | High (specific % not provided) [69] | Good retention balance | 65.6× (BALF) [69] | Balanced performance; minimal bias | Requires optimization for sample types |
| Filtration | ZISC-based filtration | >99% WBC removal [73] | Preserves microbial integrity | >10× vs. unfiltered (blood) [73] | High WBC removal; minimal clogging; preserves composition | Newer technology; less extensively validated |
| Chemical/Enzymatic | Osmotic lysis + PMA (O_pma) | Moderate | Low retention | 2.5× (BALF) [69] | Targets cell-free DNA | Least effective for enrichment; may damage fragile microbes |
| Enzymatic | Nuclease digestion only (R_ase) | Moderate | 31% (BALF - highest retention) [69] | 16.2× (BALF) [69] | Highest bacterial DNA retention | Lower host depletion efficiency |
Impact on Microbial Community Representation and AMR Detection
Beyond quantitative enrichment metrics, different host depletion methods introduce varying degrees of taxonomic bias, which directly impacts downstream resistance gene analysis. Studies demonstrate that some commensals and pathogens, including Prevotella spp. and Mycoplasma pneumoniae, can be significantly diminished by certain depletion methods, potentially altering the perceived resistome structure [69]. The fidelity of microbial community representation must therefore be considered when selecting a depletion strategy for AMR surveillance studies. Method-induced biases may lead to incomplete resistance gene profiles if relevant bacterial carriers are selectively depleted during processing.
Detailed Experimental Protocols
Filtration-Based Host Depletion Protocol (F_ase Method)
This protocol utilizes a 10μm filter followed by nuclease digestion to remove host cells and cell-free DNA, demonstrating balanced performance for respiratory samples with minimal taxonomic bias [69].
Materials Required:
- 10μm pore size filters (e.g., polycarbonate membrane filters)
- Nuclease enzyme (e.g., Benzonase or DNase I)
- Appropriate buffer solutions (PBS, Tris-HCl)
- Centrifuge and compatible tubes
- DNA extraction kit suitable for low biomass samples
Procedure:
- Sample Preparation: Centrifuge bronchoalveolar lavage fluid (BALF) or respiratory samples at 500× g for 10 minutes to remove large debris.
- Primary Filtration: Pass supernatant through a 10μm pore size filter using gentle vacuum or centrifugation to retain host cells while allowing microbial cells to pass through.
- Filter Retentate Processing: Discard the filter containing host cells, or preserve for alternative analysis if required.
- Nuclease Treatment: To the filtrate, add nuclease enzyme (optimized concentration: 5-10 U/mL) with appropriate Mg²⁺ concentration and incubate at 37°C for 30-60 minutes to degrade cell-free host DNA.
- Microbial Collection: Centrifuge the nuclease-treated filtrate at 16,000× g for 30 minutes to pellet microbial cells.
- DNA Extraction: Proceed with standard DNA extraction protocols optimized for microbial cells, ensuring complete nuclease inactivation during lysis.
- Quality Control: Assess DNA yield and host DNA contamination using qPCR targeting single-copy human genes (e.g., β-actin) and bacterial markers (e.g., 16S rRNA genes).
Optimization Notes:
- Filter pore size may require adjustment based on specific sample matrix (e.g., sputum may require pre-treatment with mucolytics).
- Nuclease concentration and incubation time should be titrated for different sample types to maximize host DNA degradation while preserving microbial genomic integrity.
- Incorporating a cryopreservation step with 25% glycerol before processing may improve microbial viability and DNA yield for certain sample types [69].
Enzymatic Host Depletion Protocol (S_ase Method)
This method employs saponin-based lysis of host cells followed by nuclease digestion, achieving among the highest host DNA depletion efficiencies for respiratory samples [69].
Materials Required:
- Saponin (molecular biology grade)
- Nuclease enzyme (DNase I or similar)
- Propidium monoazide (PMA) - optional for viability assessment
- Lysis buffer (e.g., Tris-EDTA with detergent)
- DNA extraction reagents
Procedure:
- Host Cell Lysis: Add saponin to the clinical sample at a final concentration of 0.025% (optimized from testing 0.025%-0.50% range) and incubate at room temperature for 15 minutes with gentle mixing [69].
- Optional Viability Staining: For differentiation of intact vs. compromised cells, add PMA to a final concentration of 10μM and incubate in the dark for 10 minutes, followed by photoactivation with a bright light source for 5-10 minutes.
- Nuclease Digestion: Add nuclease enzyme (5-20 U/mL final concentration) with appropriate co-factors and incubate at 37°C for 30-45 minutes to degrade released host DNA.
- Enzyme Inactivation: Heat-inactivate at 75°C for 10 minutes or use specific inhibitor solutions according to manufacturer recommendations.
- Microbial Pellet Collection: Centrifuge at 16,000× g for 30 minutes to collect intact microbial cells.
- DNA Extraction: Proceed with standard DNA extraction protocols.
- Quality Assessment: Quantify host and microbial DNA using targeted qPCR as described in section 3.1.
Technical Considerations:
- Saponin concentration is critical - higher concentrations may lyse some Gram-positive bacteria, introducing taxonomic bias.
- The method predominantly targets intact microbial cells; note that cell-free microbial DNA (representing >68% of total microbial DNA in BALF and >79% in oropharyngeal swabs) will be lost during processing [69].
- Method performance varies significantly between upper and lower respiratory tract samples due to differing host-to-microbe ratios.
Novel ZISC-Based Filtration for Blood Samples
This recently developed method utilizes Zwitterionic Interface Ultra-Self-assemble Coating technology for efficient white blood cell depletion while preserving microbial pathogens in blood samples, demonstrating particular utility for sepsis diagnostics [73].
Materials Required:
- ZISC-based filtration device (e.g., Devin filter from Micronbrane)
- Syringe (compatible with filter unit)
- Blood collection tubes
- DNA extraction kit
Procedure:
- Sample Loading: Transfer 3-13mL of whole blood into a syringe and attach the ZISC-based filter unit according to manufacturer instructions.
- Filtration: Gently depress the syringe plunger to pass the blood sample through the filter into a collection tube.
- Plasma Separation: Centrifuge the filtered blood at 400× g for 15 minutes at room temperature to separate plasma.
- Microbial Pellet Collection: Transfer plasma to a new tube and centrifuge at 16,000× g to pellet microbial cells.
- DNA Extraction: Extract DNA from the pellet using appropriate methods.
- Sequencing Library Preparation: Proceed with mNGS library preparation, potentially incorporating ultra-low input protocols if necessary.
Performance Characteristics:
- Achieves >99% white blood cell removal across various blood volumes [73].
- Allows unimpeded passage of bacteria and viruses, preserving microbial composition.
- In clinical validation, detected expected pathogens in 100% (8/8) of culture-positive sepsis samples with an average of 9,351 microbial reads per million, representing over tenfold enrichment compared to unfiltered samples [73].
Workflow Integration and Visualization
The successful implementation of host depletion methods requires careful integration into the overall mNGS workflow for AMR research. The following diagram illustrates the decision pathway for selecting and applying these techniques:
Advanced Applications: Combined and Sequential Methods
Research indicates that combining different depletion strategies can yield synergistic improvements in microbial enrichment. A study integrating enzymatic host depletion with nanopore adaptive sequencing demonstrated a median 113.41-fold increase in microbial reads compared to standard methods, detecting 6 pathogens in 4 samples with a median read count of 547, versus 5 pathogens with a median of 4 reads using standard approaches [74].
This combined methodology leverages both physical/enzymatic removal of host DNA and computational rejection of host-derived reads during real-time sequencing, substantially enhancing sensitivity for low-abundance pathogens and their resistance genes. The implementation of such integrated approaches represents a promising direction for AMR surveillance studies requiring maximum detection sensitivity.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Host Depletion Protocols
| Reagent/Category | Specific Examples | Function/Application | Considerations for AMR Studies |
|---|---|---|---|
| Commercial Kits | QIAamp DNA Microbiome Kit (Qiagen) | Differential lysis of host cells | Moderate performance; potential taxonomic bias |
| HostZERO Microbial DNA Kit (Zymo) | Commercial host depletion | High host DNA removal; lower microbial retention | |
| NEBNext Microbiome DNA Enrichment Kit | Methylation-based depletion | Poor performance for respiratory samples | |
| Enzymes | DNase I | Degrades cell-free DNA | Requires optimization for different sample matrices |
| Saponin | Selective host cell lysis | Concentration-critical; may lyse fragile microbes | |
| Specialized Equipment | ZISC-based Filtration Device | Physical host cell depletion | >99% WBC removal; preserves microbes |
| 10μm Filters | Size-based separation | Must optimize pore size for sample type | |
| Molecular Biology Reagents | Propidium Monoazide (PMA) | Viability dye for intact cells | Helps distinguish between viable and free DNA |
| Glycerol-based Cryoprotectants | Sample preservation | 25% glycerol improves microbial viability |
Host depletion techniques, particularly filtration- and enzymatic-based methods, substantially enhance the sensitivity of metagenomic NGS for antimicrobial resistance research by reducing host DNA background and enriching microbial content. The optimal method selection depends on sample type, research priorities (maximal host depletion vs. microbial DNA retention), and practical laboratory considerations. As AMR surveillance increasingly relies on comprehensive resistome characterization, implementing appropriate host depletion strategies becomes essential for accurate detection of low-abundance resistance genes and their bacterial hosts. Future methodological developments will likely focus on combining multiple depletion strategies and optimizing protocols for specific sample matrices to further improve detection sensitivity while minimizing taxonomic bias.
In the field of antimicrobial resistance (AMR) research, metagenomic next-generation sequencing (mNGS) has become a pivotal tool for comprehensively analyzing microbial communities and their resistomes without the need for cultivation [75]. A central challenge in this research is effectively balancing the cost, labor, and efficiency of two fundamentally different enrichment strategies: wet-lab enrichment, which physically selects target genetic material prior to sequencing, and computational enrichment, which uses bioinformatic tools to in silico isolate relevant sequences from complex datasets.
Wet-lab techniques, such as probe-based hybridization capture, aim to increase the sensitivity of detection for low-abundance targets by reducing background noise [76]. In contrast, computational methods leverage the power of data analysis to extract meaningful patterns and genes from large, unbiased sequencing datasets [48]. The choice between these paths significantly impacts the scope, cost, and ultimate success of AMR surveillance and discovery projects. This application note provides a structured comparison and detailed protocols to guide researchers in selecting and implementing the optimal strategy for their specific research context within the broader framework of a thesis on AMR.
Comparative Analysis: Wet-Lab vs. Computational Enrichment
The decision to employ wet-lab or computational enrichment is multifaceted. The table below summarizes the key characteristics of each approach to aid in this strategic choice.
Table 1: Comparative Analysis of Wet-Lab and Computational Enrichment for AMR mNGS Research
| Feature | Wet-Lab Enrichment | Computational Enrichment |
|---|---|---|
| Primary Objective | Physical selection and amplification of target sequences (e.g., ARGs, pathogen genomes) before sequencing [76]. | In silico identification and analysis of target sequences from complex, non-enriched sequencing data [48]. |
| Typical Workflow | Sample collection → DNA extraction → Target Enrichment (e.g., probe capture) → Library Prep → Sequencing → Data Analysis [76]. | Sample collection → DNA extraction → Library Prep → Sequencing → Bioinformatic Analysis & Target Identification [75]. |
| Key Techniques | Probe-hybridization capture (e.g., RNA baits); PCR amplification; long-read sequencing for full-length gene recovery [75] [76]. | Bacterial genome-wide association studies (bGWAS); machine learning; resistome mapping; phylogenetic analysis [48]. |
| Cost & Labor Profile | High consumable costs (probes, kits); moderate to high hands-on labor; requires specialized wet-lab equipment [76]. | Lower sequencing consumable cost per sample; high computational infrastructure cost; labor shifted to bioinformatic analysis [77] [78]. |
| Data & Infrastructure | Generates less, but more targeted, data; requires standard molecular biology lab infrastructure [76]. | Generates large, complex datasets; requires high-performance computing (HPC) clusters and data storage [77]. |
| Best-Suited Applications | Detecting low-abundance, high-risk ARGs; attributing ARGs to host species via long reads; surveillance in low-biomass or high-background samples [75] [76]. | Large-scale genomic epidemiology; outbreak investigation; discovery of novel resistance mechanisms; retrospective analysis of existing datasets [48]. |
Experimental Protocols
Protocol 1: Wet-Lab Enrichment via RNA-Probe Hybridization Capture for ARG Detection
This protocol, adapted from a wastewater surveillance study, details a method for the highly sensitive detection of clinically important antimicrobial resistance genes (ARGs) using targeted enrichment [76].
1. Principle Biotinylated RNA probes, designed to complement known ARG sequences, are hybridized to fragmented, adapter-ligated metagenomic DNA. Probe-target hybrids are selectively captured using streptavidin-coated magnetic beads, thereby enriching the sample for ARG sequences prior to sequencing. This method significantly improves detection sensitivity for genes that may be undetectable by standard shotgun metagenomics [76].
2. Reagents and Equipment
- Metagenomic DNA (≥ 1 ng/µL, recommended for library preparation)
- Biotinylated RNA Probe Panel (e.g., probes for blaKPC, blaNDM, blaVIM, blaOXA-48, vanA, mcr-1)
- Streptavidin-Coated Magnetic Beads
- Library Preparation Kit (e.g., Illumina-compatible)
- Hybridization Buffer (e.g., SSC-based buffer with formamide)
- Wash Buffers (Stringent and non-stringent)
- Magnetic Separation Rack
- Thermal Cycler with heated lid
- Qubit Fluorometer or similar for DNA quantification
3. Step-by-Step Procedure A. Library Preparation
- Fragment the metagenomic DNA to a target size of 200-500 bp using acoustic shearing or enzymatic fragmentation.
- Convert the fragmented DNA into a sequencing library using a standard library preparation kit, including end-repair, A-tailing, and adapter ligation. Do not perform PCR amplification at this stage to avoid bias.
- Quantify the final library concentration using a fluorometric method.
B. Hybridization and Capture
- Denature and Hybridize: Combine the library (∼ 100-200 ng) with the biotinylated RNA probe pool and hybridization buffer in a PCR tube. Denature at 95°C for 5-10 minutes and immediately transfer to a thermal cycler for hybridization (e.g., 16-24 hours at 65°C).
- Capture: Add pre-washed streptavidin magnetic beads to the hybridization reaction and incubate at room temperature for 30-45 minutes with gentle mixing to allow the bead-streptavidin/biotin-probe hybrids to form.
- Wash: Place the tube on a magnetic rack to pellet the beads. Carefully remove the supernatant containing non-hybridized DNA.
- Perform 2-3 washes with a pre-warmed stringent wash buffer (e.g., containing SDS and SSC) at 65°C to remove non-specifically bound DNA.
- Perform one wash with a non-stringent buffer at room temperature.
- Elute: Resuspend the beads in nuclease-free water or a low-salt elution buffer. Denature at 95°C for 5-10 minutes to release the captured DNA from the beads. Immediately place the tube on a magnetic rack and transfer the supernatant, which contains the enriched library, to a new tube.
C. Post-Capture Amplification and Sequencing
- Amplify: Perform a limited-cycle (e.g., 12-14 cycles) PCR amplification of the enriched library using primers compatible with your sequencing adapters.
- Quality Control and Sequence: Purify the final PCR product, quantify, and check the size distribution using a Bioanalyzer or Tapestation. Proceed with sequencing on an appropriate platform (e.g., Illumina).
4. Critical Considerations
- Probe Design: The specificity and sensitivity of the assay are entirely dependent on the probe design. Probes must be designed to cover known variants of target ARGs.
- Background Depletion: The use of blockers (e.g., Cot-1 DNA, adapter-specific blockers) during hybridization is crucial to prevent non-specific binding of repetitive sequences and adapter-dimers to the beads.
- Negative Controls: Always include a non-enriched library and a no-probe control to assess the efficiency and specificity of the capture process.
Protocol 2: Computational Enrichment for Resistome Analysis from Shotgun mNGS Data
This protocol outlines a standard bioinformatic workflow for characterizing the resistome—the full complement of ARGs in a metagenomic sample—from shotgun sequencing data.
1. Principle Raw sequencing reads are quality-controlled and assembled. ARGs and other mobile genetic elements (MGEs) are then identified using reference databases, allowing for the analysis of their abundance, diversity, and genetic context without any physical pre-selection [48] [75].
2. Software and Hardware Requirements
- Computational Infrastructure: Access to a high-performance computing (HPC) environment or a powerful workstation with substantial RAM (≥ 64 GB recommended) and multi-core processors.
- Bioinformatic Tools:
- Quality Control: FastQC, Trimmomatic, or FastP
- Metagenomic Assembly: MEGAHIT, metaSPAdes
- Read Classification: Kraken2/Bracken, MetaPhlAn
- Resistome Analysis: ABRicate, AMRPlusPlus, DeepARG, RGI (Resistance Gene Identifier)
- Visualization: R with ggplot2, Pavian, anvi'o
3. Step-by-Step Procedure A. Data Pre-processing and Quality Control (QC)
- Quality Check: Run FastQC on raw FASTQ files to assess per-base sequence quality, adapter contamination, and GC content.
- Trimming and Adapter Removal: Use Trimmomatic or FastP to trim low-quality bases (e.g., Phred score < 20) and remove adapter sequences.
B. Metagenomic Assembly and Gene Calling
- Co-assembly or Single-assembly: Assemble the trimmed reads using a metagenomic assembler like MEGAHIT or metaSPAdes. The choice between co-assembling multiple samples or assembling individually depends on the research question and computational resources.
- Contig Binning (Optional): For more advanced analysis, contigs can be binned into putative Metagenome-Assembled Genomes (MAGs) using tools like MetaBAT2 or MaxBin2.
C. Resistome Profiling
- ARG Identification:
- Read-based: Directly map the quality-filtered reads to a curated ARG database (e.g., CARD, ResFinder, MEGARes) using a aligner like Bowtie2 or BWA. This provides a quantitative measure of ARG abundance.
- Contig-based: Scan the assembled contigs against ARG databases using tools like ABRicate or RGI. This allows for the detection of ARGs in a genomic context and can help link them to specific taxa or MGEs.
- Taxonomic Profiling: Classify reads or contigs using a taxonomic classifier like Kraken2 to understand the microbial community structure and potentially associate ARGs with their bacterial hosts.
D. Data Analysis and Integration
- Normalization: Normalize ARG hit counts (from read-based analysis) by sequencing depth (e.g., reads per kilobase per million mapped reads - RPKM) or by the number of 16S rRNA gene copies to enable cross-sample comparisons.
- Correlation with Metadata: Integrate the resistome and microbiome data with sample metadata (e.g., treatment type, location, time point) using statistical methods in R (e.g., PCA, PERMANOVA) to identify significant associations.
4. Critical Considerations
- Database Selection: The choice of ARG database (CARD, ResFinder, etc.) can significantly impact results, as they vary in scope and curation. It is good practice to use multiple databases or a comprehensive, merged one.
- Limitations of Assembly: Complex metagenomes from highly diverse environments may not assemble well, leading to fragmented contigs that make it difficult to link ARGs to their hosts or MGEs. Long-read sequencing can mitigate this [75].
- Functional Validation: Computational predictions of ARGs should be considered putative. Wet-lab experiments (e.g., functional expression in a vector) are required for definitive confirmation of resistance phenotypes.
Workflow Visualization
The following diagrams illustrate the core procedural and decision-making pathways for the two enrichment strategies.
Wet-Lab Probe Capture Workflow
Wet-Lab ARG Enrichment via Probe Capture
Computational Resistome Analysis Workflow
Computational Resistome Analysis from mNGS
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful implementation of the described protocols requires specific reagents and computational tools. The following table details key solutions for AMR mNGS research.
Table 2: Essential Reagents and Tools for AMR mNGS Research
| Item Name | Function/Application | Specific Example/Note |
|---|---|---|
| Portable DNA Extraction Kit (e.g., Claremont Bio DNAexpress, Zymo Quick-DNA HMW MagBead) | Enables on-site mechanical lysis and purification of high-quality metagenomic DNA, crucial for field surveillance [75]. | Optimized for use with portable bead-beaters (e.g., Omnilyse X); includes all necessary buffers and columns/magnetic beads for purification. |
| Targeted Probe Panels | Custom or pre-designed biotinylated RNA/DNA oligonucleotides for hybridisation capture of specific ARG targets (e.g., carbapenemase genes) [76]. | Probes are designed against sequences from databases like CARD or ResFinder; essential for wet-lab enrichment sensitivity. |
| Streptavidin Magnetic Beads | The solid-phase matrix for capturing and purifying biotinylated probe-DNA hybrids during the enrichment protocol [76]. | Paramagnetic particles that facilitate easy separation and washing in a magnetic rack. |
| Long-read Sequencing Kit (e.g., Oxford Nanopore Technologies Ligation Sequencing Kit) | Facilitates sequencing of long DNA fragments, allowing for recovery of full-length ARGs and their genomic context (e.g., on plasmids) [75]. | Key for determining the genetic location and linkage of ARGs, which is critical for understanding transmission risk. |
| Curated ARG Database (e.g., CARD, ResFinder, MEGARes) | Reference databases used for the in silico identification and annotation of ARG sequences from raw reads or assembled contigs [48]. | The foundation of all computational resistome analysis; database choice directly impacts results. |
| Bioinformatic Pipelines (e.g., AMRPlusPlus, ARIBA) | Integrated software workflows that automate the steps of resistome analysis, from QC and assembly to ARG annotation and reporting [48]. | Standardizes analysis, improves reproducibility, and reduces the bioinformatic burden on researchers. |
The choice between wet-lab and computational enrichment is not a question of which is universally superior, but which is optimal for a given research objective and resource context. Wet-lab enrichment is unparalleled for sensitive, targeted detection of known, high-priority ARGs in complex samples, making it ideal for specific surveillance and diagnostic applications [76]. Computational enrichment, on the other hand, offers a broad, untargeted view of the resistome, enabling discovery and large-scale epidemiological studies from a single, standard sequencing run [48].
For a comprehensive thesis on AMR, the most powerful approach may be a hybrid one. Leveraging computational tools for initial, broad-scale resistome characterization of samples can effectively identify targets of interest. Subsequently, wet-lab enrichment can be deployed for deep, sensitive investigation of those specific targets across a larger sample set or to resolve their genetic context with long-read sequencing. By understanding the strengths, costs, and applications of each method, researchers can design more efficient and impactful metagenomic studies to combat the global threat of antimicrobial resistance.
The rising threat of antimicrobial resistance (AMR) necessitates advanced diagnostic tools capable of rapid and accurate pathogen characterization. Metagenomic next-generation sequencing (mNGS) has emerged as a transformative technology for infectious disease diagnostics, enabling hypothesis-free detection of bacteria, viruses, fungi, and parasites directly from clinical specimens [1]. Unlike traditional culture and targeted molecular assays, mNGS can identify novel, fastidious, and polymicrobial infections while simultaneously characterizing antimicrobial resistance genes [1]. However, the analytical sensitivity of mNGS for AMR detection is critically dependent on two fundamental parameters: sequencing depth and the application of appropriate bioinformatics filters. This application note examines the impact of these parameters within the context of AMR gene analysis, providing evidence-based protocols to optimize detection sensitivity and accuracy for researchers, scientists, and drug development professionals.
The Critical Role of Sequencing Depth in AMR Detection
Sequencing depth, typically measured as the number of reads covering a genomic region, directly determines the ability to detect antimicrobial resistance genes, particularly in complex metagenomic samples or those with low pathogen biomass. Inadequate depth can lead to false negatives, while excessive depth may be economically inefficient without corresponding benefits.
Minimum Depth Requirements for Reliable Detection
Table 1: Sequencing Depth Recommendations for AMR Detection
| Analysis Type | Minimum Coverage | Read Requirements for Metagenomes | Key Findings |
|---|---|---|---|
| Single E. coli Isolate | 15× (300,000 reads) | N/A | Sensitivity and PPV ~1.00 for ARG detection [79] |
| Metagenomic Samples (1% abundance) | 15× target coverage | ~30 million reads | Required for adequate sensitivity in complex communities [79] |
| AMR Gene Family Richness | N/A | 80 million reads/sample | Depth to recover 95% of AMR gene family richness [80] |
| AMR Allelic Diversity | N/A | >200 million reads/sample | Full allelic diversity not captured even at maximum depth [80] |
Research demonstrates that approximately 300,000 reads or 15× genome coverage is sufficient to detect antimicrobial resistance genes in Escherichia coli ST38 with sensitivity and positive predictive value comparable to much higher coverages (~100×) [79]. This threshold reliably detected β-lactamases (blaCTX-M-15, blaTEM-1, blaOXA-1), aminoglycoside transferases, efflux pumps, and resistance-conferring single nucleotide polymorphisms (SNPs) in gyrA and parC [79].
However, metagenomic samples present greater challenges due to microbial complexity and host DNA contamination. For target organisms present at 1% relative abundance in metagenomic communities, assembly of approximately 30 million reads is necessary to achieve the critical 15× target coverage required for reliable ARG detection [79]. Deeper sequencing is essential for comprehensive resistome characterization, with one study finding that 80 million reads per sample were required to recover 95% of AMR gene family richness, while additional allelic diversity continued to be discovered even at 200 million reads [80].
Bioinformatics Filters for Enhanced Specificity
Bioinformatics filtering strategies are essential to distinguish true resistance determinants from background noise and to manage the high dimensionality of mNGS data. These approaches can be broadly categorized into assembly-based and read-based methods, each with distinct advantages.
Assembly-Based Versus Read-Based Approaches
Assembly-based methods involve de novo assembly of raw sequencing reads into contiguous sequences (contigs) followed by alignment to ARG reference databases. This approach generally offers improved accuracy, especially in complex or low-abundance datasets, and provides contextual information about genetic neighborhood [81].
Read-based methods directly align raw sequencing reads to ARG reference databases, enabling faster analysis that is more suitable for rapid screening applications [81]. However, this approach may miss novel genes with lower homology to database sequences.
Studies comparing these approaches for ARG prediction have found that assembly-based methods using tools like the Resistance Gene Identifier (RGI) with the Comprehensive Antibiotic Resistance Database (CARD) can achieve high sensitivity and positive predictive value with appropriate sequencing depth [79]. The choice between methods often involves trade-offs between computational efficiency, sensitivity, and the need for contextual genetic information.
Normalization Strategies and Their Impact
Normalization of ARG abundance data critically affects quantitative assessments of resistance potential. Gene length normalization substantially alters abundance distributions and rank order of AMR variants [80]. Spike-in controls, such as exogenous Thermus thermophilus DNA, enable more accurate cross-sample comparison by estimating absolute gene abundance in a sample [80].
Table 2: Key Bioinformatics Tools for ARG Detection
| Tool Name | Methodology | Primary Application | Key Features |
|---|---|---|---|
| RGI with CARD | Assembly-based | Genomic & metagenomic analysis | Ontology-driven, manual curation, includes Resistance Gene Identifier [81] |
| ResFinder/PointFinder | K-mer alignment | Acquired genes & chromosomal mutations | Integrated platform for genes and point mutations [81] |
| DeepARG | Machine learning | Novel ARG prediction | AI-based approach for identifying novel resistance genes [81] |
| AMRFinderPlus | Sequence homology | Comprehensive detection | Detects acquired genes, chromosomal mutations, and resistance variants [81] |
Experimental Protocols for Optimal AMR Detection
Protocol: Determining Optimal Sequencing Depth for Metagenomic Resistome Profiling
Purpose: To establish the minimum sequencing depth required for comprehensive AMR gene detection in complex microbial communities.
Materials:
- High-quality metagenomic DNA extracts
- Illumina-compatible library preparation kit
- Exogenous control DNA (Thermus thermophilus)
- Computing infrastructure with bioinformatics software (FastQC, Trimmomatic, RGI, CARD database)
Procedure:
- Library Preparation and Sequencing:
- Spike metagenomic DNA with 0.1% T. thermophilus DNA as normalization control
- Prepare sequencing libraries using standardized protocols
- Sequence on Illumina platform to target depth of >200 million 150bp paired-end reads
Bioinformatic Processing:
- Perform quality control using FastQC [82]
- Trim adapters and low-quality bases using Trimmomatic
- Subsample reads to various depths (1M, 10M, 20M, 40M, 80M, 160M, 200M)
- Assemble reads at each depth using metaSPAdes
- Predict ARGs using RGI with CARD database
Analysis and Depth Determination:
- Calculate rarefaction curves for AMR gene families and allelic variants
- Identify sequencing depth where 95% of AMR gene richness is captured (d0.95)
- Establish minimum depth for reliable detection of low-abundance resistance determinants
Troubleshooting: If rarefaction curves fail to plateau, consider additional sequencing or targeted enrichment approaches for low-abundance targets.
Protocol: Bioinformatics Filtering for Enhanced ARG Detection
Purpose: To implement a standardized bioinformatics workflow for sensitive and specific ARG detection from mNGS data.
Materials:
- High-performance computing cluster
- RGI software (v5.0.0+) with CARD database
- Alternative ARG databases (ResFinder, MEGARes)
- Quality assessment tools (FastQC, MultiQC)
Procedure:
- Data Quality Control:
Host DNA Depletion:
- Align reads to host reference genome (e.g., human GRCh38) using BWA
- Retain unmapped reads for downstream analysis
ARG Detection:
- For assembly-based approach:
- For read-based approach:
Result Normalization and Filtering:
- Normalize hit counts by gene length and spike-in control abundance
- Apply minimum identity (90%) and coverage (80%) thresholds
- Filter out putative false positives using bit-score cutoffs
Validation: Compare results across multiple databases and validate key findings with PCR or culture-based methods when possible.
Visualizing Workflows and Relationships
Figure 1: Bioinformatics Workflow for ARG Detection from mNGS Data. This workflow outlines the critical steps for processing metagenomic sequencing data to identify antimicrobial resistance genes, highlighting parallel assembly-based and read-based approaches.
Figure 2: Impact of Sequencing Depth and Bioinformatics Filters on ARG Detection Accuracy. This diagram illustrates how different parameter settings affect the sensitivity and specificity of antimicrobial resistance gene detection in metagenomic analyses.
Table 3: Essential Research Reagents and Computational Resources for mNGS-based AMR Detection
| Category | Resource | Specifications/Requirements | Application in AMR Research |
|---|---|---|---|
| Reference Databases | CARD (Comprehensive Antibiotic Resistance Database) | Requires regular updates; includes ARO ontology | Primary reference for ARG annotation and mechanism classification [81] |
| Bioinformatics Tools | RGI (Resistance Gene Identifier) | Compatible with CARD; assembly and read-based modes | Standardized ARG prediction from genomic and metagenomic data [79] [81] |
| Quality Control Tools | FastQC | Java-based; processes FASTQ files | Initial quality assessment of raw sequencing data [82] |
| Exogenous Controls | Thermus thermophilus DNA | Spike at 0.1-1% concentration | Normalization for cross-sample comparison and quantification [80] |
| Sequencing Platforms | Illumina short-read | 2×150bp configuration; >30M reads per metagenome | High-accuracy sequencing for resistome profiling [79] |
| Analysis Pipelines | ResPipe | Open-source; available via GitLab | Automated processing of metagenomic data for AMR gene detection [80] |
| Specialized Algorithms | Genetic Algorithm-AutoML | Python implementation; requires transcriptomic data | Identification of minimal predictive gene sets for resistance [83] |
Optimizing analytical sensitivity in metagenomic AMR detection requires careful consideration of both experimental and computational parameters. Evidence indicates that 15× coverage provides a reliable minimum for ARG detection in isolate genomes, while metagenomic samples from complex communities may require 30-80 million reads to adequately capture resistance gene diversity, with deeper sequencing needed for comprehensive allelic variant detection [79] [80]. Bioinformatics filters, particularly assembly-based approaches using curated databases like CARD, provide superior accuracy for well-characterized genes, while read-based methods and machine learning approaches offer advantages for rapid screening and novel gene detection [81]. The integration of appropriate normalization strategies, including gene length correction and exogenous spike-in controls, further enhances the quantitative accuracy of resistome analyses [80]. By implementing these evidence-based protocols for sequencing depth optimization and bioinformatics filtering, researchers can significantly enhance the sensitivity and reliability of AMR detection in metagenomic studies, ultimately supporting more effective surveillance and management of antimicrobial resistance across clinical, environmental, and agricultural settings.
In the context of antimicrobial resistance (AMR) research using metagenomic next-generation sequencing (mNGS), distinguishing true infection from mere colonization is a fundamental diagnostic challenge. The respiratory tract, for instance, is not sterile but hosts a rich microbiome, and in immunocompromised patients, nearly any bacterial species can potentially act as a pathogen. Inappropriate or excessive antimicrobial therapy driven by misdiagnosis can lead to adverse outcomes and endanger patient survival. mNGS detects microbial nucleic acids in clinical samples without prior suspicion, but its results must be interpreted with caution. This application note provides structured data, validated protocols, and analytical frameworks to help researchers and clinicians accurately differentiate bacterial colonization from infection in mNGS-based AMR studies.
Quantitative Benchmarks for Differentiation
Critical thresholds for sequencing data have been established to aid in the interpretation of mNGS results. The following table summarizes key metrics validated for distinguishing infection from colonization in lower respiratory tract infections (LRTIs).
Table 1: Quantitative Metrics for Differentiating Bacterial Infection from Colonization via mNGS
| Metric | Technology | AUC Value (95% CI) | Cut-off Value | Sensitivity | Specificity | P-value |
|---|---|---|---|---|---|---|
| Relative Abundance | RNA-mNGS | 0.991 (0.977-1.000) | 26.28% | 0.957 | 0.974 | <0.001 |
| Relative Abundance Ratio (1st/2nd ranked bacterium) | DNA-mNGS | 0.839 (0.749-0.929) | 47.26 | 0.644 | 0.929 | <0.001 |
| Sequencing Reads Ratio (1st/2nd ranked bacterium) | DNA-mNGS | 0.835 (0.742-0.928) | 47.26 | 0.644 | 0.929 | <0.001 |
Interpretation Guidelines:
- RNA-mNGS demonstrates superior diagnostic performance, with a bacterial relative abundance above 26.28% being a strong indicator of true infection [84].
- When only DNA-mNGS is available, the ratio of relative abundance or sequencing reads between the top-ranked bacterium and the second-ranked bacterium is a reliable predictor. A ratio above 47.26 suggests infection, though with lower sensitivity than RNA-based metrics [84].
Wet-Lab Protocol: Integrated DNA & RNA-mNGS Workflow
This protocol is designed for processing bronchoalveolar lavage fluid (BALF) to simultaneously profile both DNA and RNA pathogens, enabling a more accurate assessment of active infection.
Sample Collection & Storage
- Collection: Collect 10-20 mL of BALF via bronchoscopy following standard clinical procedures [84].
- Storage: Immediately transfer the specimen into an EP tube containing DNA/RNA Shield (e.g., from Zymo Research) to preserve nucleic acid integrity. Store and transport at 2-8°C [84].
Nucleic Acid Extraction
- DNA Extraction: Use the TIANGamp Magnetic DNA Kit (TIANGEN) or similar, following the manufacturer's instructions. Quantify DNA using a fluorometer (e.g., Qubit 2.0) [84].
- RNA Extraction: Extract RNA from the supernatant using the QIAamp Viral RNA Mini Kit (QIAGEN). The quality and quantity of extracted RNA should also be assessed [84].
Library Preparation & Sequencing
- DNA Library Prep: Use the Hieff NGS C130P2 OnePot II DNA Library Prep Kit for MGI (Yeasen Biotech) per the manufacturer's protocol [84].
- RNA Library Prep:
- rRNA Depletion: Remove ribosomal RNA (rRNA) from the total RNA using the Hieff NGS MaxUp rRNA Depletion Kit (Yeasen Biotech). This step uses probes that hybridize to rRNA, forming DNA-RNA heteroduplexes that are subsequently degraded by RNase H [84].
- Library Construction: The resulting rRNA-depleted RNA is then subjected to reverse transcription and strand-specific library construction [84].
- Sequencing: Sequence the prepared libraries on an appropriate NGS platform, such as the MGI or Illumina systems.
Dry-Lab Protocol: Bioinformatic Analysis & AMR Detection
Metagenomic Data Processing
- Quality Control & Host Depletion: Remove low-quality sequences and adapter sequences. Subtract reads aligning to the host genome (e.g., human) to enrich for microbial reads [1].
- Taxonomic Profiling: Align non-host reads to comprehensive microbial genome databases using tools like MetaPhlAn for species-level identification [10].
- Calculate Key Metrics:
- Sequencing Reads: The absolute number of reads mapped to a specific bacterial species.
- Relative Abundance: The proportion of a bacterium's reads relative to all microbial reads in its category (bacteria, fungi, viruses, or parasites) after host sequence removal [84].
Antibiotic Resistance Gene (ARG) Analysis
- ARG Identification: Profile the resistome by aligning sequencing data against curated ARG databases.
- Recommended Databases: The Comprehensive Antibiotic Resistance Database (CARD), ResFinder, and ARG-ANNOT are widely used. ARG-ANNOT is particularly noted for its ability to detect both existing and putative new ARGs, including point mutations in chromosomal targets [85] [81].
- Recommended Tools: The Resistance Gene Identifier (RGI) for CARD or AMRFinderPlus are robust tools for this purpose [81].
- Contextualize ARG Findings: The presence of an ARG does not automatically indicate infection. Correlate ARG detection with the quantitative metrics in Table 1. An ARG found in a bacterium with high relative abundance or dominance is of greater clinical concern.
The following workflow diagram illustrates the complete process from sample to clinical interpretation:
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Resources for mNGS-based Infection/Colonization Studies
| Item | Function / Application | Example Product / Kit |
|---|---|---|
| Nucleic Acid Protectant | Preserves DNA and RNA integrity immediately after sample collection, critical for accurate RNA-based assessment of active infection. | DNA/RNA Shield (Zymo Research) [84] |
| DNA Extraction Kit | Isolates microbial genomic DNA from complex clinical samples like BALF. | TIANamp Magnetic DNA Kit (TIANGEN) [84] |
| RNA Extraction Kit | Isolates total RNA, including microbial transcripts, to profile active pathogens. | QIAamp Viral RNA Mini Kit (QIAGEN) [84] |
| rRNA Depletion Kit | Removes abundant ribosomal RNA to enrich for informative messenger and other non-ribosomal RNAs, improving pathogen transcript detection. | Hieff NGS MaxUp rRNA Depletion Kit (Yeasen Biotech) [84] |
| DNA Library Prep Kit | Prepares sequencing libraries from extracted DNA for metagenomic profiling. | Hieff NGS C130P2 OnePot II DNA Library Prep Kit for MGI (Yeasen Biotech) [84] |
| ARG Database | A curated reference for identifying and annotating antibiotic resistance genes from sequence data. | CARD, ResFinder, ARG-ANNOT [85] [81] |
Integrating the quantitative benchmarks and multi-omics protocols outlined in this document is essential for the precise clinical interpretation of mNGS data within AMR research. The superior performance of RNA-mNGS highlights the importance of detecting transcriptional activity to identify active infections. By applying these standardized workflows, thresholds, and bioinformatic tools, researchers and drug developers can more effectively stratify patients, prioritize novel AMR targets, and ultimately contribute to the development of targeted therapies that combat resistant infections while curbing unnecessary antibiotic use.
The fight against antimicrobial resistance (AMR) relies heavily on the ability to accurately profile and monitor resistance genes within microbial communities. Metagenomic next-generation sequencing (mNGS) has emerged as a transformative tool for this purpose, enabling the culture-free detection of antimicrobial resistance genes (ARGs) directly from clinical, environmental, and animal samples [1] [8]. This approach allows researchers to study the resistome—the collection of all ARGs within a microbiome—including genes from non-cultivable organisms, thereby providing a more comprehensive picture of AMR potential [14] [10].
However, the promise of mNGS in AMR research is tempered by significant standardization challenges that affect the reproducibility of both wet-lab procedures and bioinformatics analyses. Variability in sample processing, sequencing platforms, and computational methods can lead to inconsistent results, making cross-study comparisons difficult and hindering the translation of research findings into clinical or public health interventions [1] [86]. This application note details the specific hurdles to achieving reproducible mNGS pipelines for AMR analysis and provides structured protocols and data to guide researchers toward more standardized, reliable practices.
Wet-Lab Standardization Hurdles and Protocols
The initial stages of mNGS workflow introduce substantial variability, which can compromise the quantitative accuracy of downstream AMR gene profiling.
Key sources of pre-analytical variability include:
- Sample Collection and Nucleic Acid Extraction: Inconsistent methods (e.g., use of different commercial kits) can drastically alter microbial community representation and impact DNA yield and quality [10].
- Host DNA Depletion: The efficiency of removing host genetic material (e.g., from human cells) is crucial for enriching microbial DNA, especially in low-biomass samples. Variable depletion efficiency directly affects the sensitivity for detecting low-abundance pathogens and ARGs [1].
- Library Preparation and Sequencing Platforms: Choices between library kits (e.g., Illumina DNA Prep) and sequencing platforms (e.g., Illumina vs. Oxford Nanopore) can introduce biases in coverage, read length, and error profiles [1] [87]. For instance, the high host DNA background in samples like blood or bronchoalveolar lavage fluid necessitates optimized depletion protocols to achieve sufficient sequencing depth for microbial content [1].
Standardized Experimental Protocol for AMR Focused mNGS
Protocol Title: Standardized Metagenomic DNA Preparation for Antimicrobial Resistome Profiling
1. Sample Collection and Storage: * Clinical/Environmental Samples: Collect samples (stool, soil, water) in sterile containers. For stool, homogenize in RNAlater or glycerol buffer. For water, filter a specified volume (e.g., 1L) and retain the filter membrane [10]. * Storage: Immediately freeze samples at -80°C or maintain in a cold chain (2-8°C) during transport to preserve nucleic acid integrity.
2. DNA Extraction: * Use a standardized, bead-beating enhanced kit (e.g., QIAamp Fast DNA Stool Mini Kit for fecal samples, PowerSoil DNA Isolation Kit for environmental samples) to ensure comprehensive lysis of diverse bacterial species, including Gram-positive bacteria [10]. * Quality Control: Quantify DNA using a fluorometer (e.g., Qubit). Assess purity and integrity via spectrophotometry (A260/A280 ratio) and agarose gel electrophoresis (0.8% gel).
3. Host DNA Depletion (for host-associated samples): * Apply a validated host depletion method (e.g., saponin-based lysis or kit-based prokaryote enrichment) to a fixed input amount of DNA (e.g., 1 µg) [1]. * Post-depletion, re-quantify microbial DNA to ensure sufficient yield for library preparation.
4. Metagenomic Library Preparation: * Use 1 ng of genomic DNA as input for library preparation with a standardized kit (e.g., Illumina MiSeq Nextera XT DNA Library Preparation Kit) [10]. * Follow manufacturer's instructions for tagmentation, indexing, and amplification. Clean up libraries using AMPure XP beads. * Pooling and Normalization: Quantify final libraries, normalize to an even concentration (e.g., 4 nM), and pool equimolar amounts for multiplexed sequencing.
5. Sequencing: * Perform paired-end sequencing (e.g., 2x151 bp or 2x300 bp) on an Illumina MiSeq or similar platform to achieve a minimum of 5-10 million reads per sample for adequate resistome coverage [10].
Bioinformatics Standardization Hurdles
Following sequencing, bioinformatics analysis presents another layer of complexity where lack of standardization can severely impact the reproducibility and comparability of AMR gene profiles.
Normalization and Comparative Metagenomics
A primary challenge in bioinformatics is the quantitative comparison of taxa or gene abundances across different samples or studies. Shotgun metagenomic data is inherently compositional and subject to technical biases from sequencing depth and protocol differences [86]. Normalization methods are essential to mitigate these variations.
Table 1: Performance of Normalization Methods in Cross-Study Phenotype Prediction
| Method Category | Example Methods | Reported Performance in Cross-Study Context |
|---|---|---|
| Scaling Methods | TMM, RLE, TSS, UQ, MED, CSS | TMM and RLE show more consistent performance than TSS-based methods when population heterogeneity (background distribution of taxa) exists between training and testing datasets [88]. |
| Transformation Methods | CLR, LOG, Blom, NPN, Rank, VST | Methods that achieve data normality (Blom, NPN) can effectively align distributions across populations. CLR and VST performance decreases with increasing population effects [88]. |
| Batch Correction Methods | BMC, Limma, Combat | Consistently outperform other approaches in removing batch effects and enhancing prediction accuracy for both binary and quantitative phenotypes in heterogeneous datasets [88] [89]. |
Different normalization methods can lead to vastly different biological interpretations. The effectiveness of a method is constrained by the degree of population effects, disease effects, and technical batch effects present in the data [88]. For predicting quantitative phenotypes like bacterial load or resistance levels, no single normalization method has demonstrated significant superiority, though batch correction methods are generally recommended as a first step [89].
Database and Pipeline Inconsistencies
The accurate identification and annotation of ARGs are highly dependent on the reference databases and bioinformatics tools used. Inconsistencies in resistance gene annotation remain a significant hurdle [1]. Different databases may have varying scopes, curation quality, and nomenclature for the same ARG. Furthermore, bioinformatic pipelines for taxonomic profiling (e.g., MetaPhlAn) and ARG detection (e.g., various alignment-based and de novo methods) can produce conflicting results if not standardized and benchmarked [1] [86] [10]. The critical role of mobile genetic elements (MGEs) like plasmids, integrons, and transposons in AMR dissemination adds another layer of complexity, requiring specialized tools for detection and linkage with ARGs [8].
Standardized Bioinformatics Protocol for AMR Analysis
Protocol Title: Bioinformatic Analysis of Metagenomic Data for Antimicrobial Resistance Gene Profiling
1. Raw Data Quality Control and Preprocessing: * Use FastQC to assess raw read quality from FASTQ files [90]. * Perform trimming and adapter removal using tools like Trimmomatic or Cutadapt to retain high-quality reads (e.g., Q-score ≥ 30) [87].
2. Host DNA Read Removal: * Align reads to the host reference genome (e.g., human GRCh38) using a rapid aligner like Bowtie 2. Discard aligned reads to obtain a purified set of microbial reads for downstream analysis [1].
3. Taxonomic Profiling: * Use a standardized profiler such as MetaPhlAn, which leverages a database of clade-specific marker genes, to identify and quantify the microbial composition of the sample [10].
4. Functional Profiling & ARG Identification: * Alignment-based ARG Detection: Align high-quality microbial reads to a curated ARG database (e.g., CARD, ARDB) using tools like Bowtie 2 or BLAST. Use the alignment counts to estimate ARG abundance [86] [41]. * De Novo Assembly and Gene Prediction: As an alternative or complementary approach, perform de novo assembly of reads into contigs using tools like SPAdes or MEGAHIT. Predict open reading frames (ORFs) on the contigs and subsequently align these predicted genes against ARG databases [86] [14]. * MGE Detection: Screen the assembled contigs or reads for key MGEs (integrons, transposons, plasmid-associated genes) using dedicated databases and tools to understand the potential for horizontal gene transfer of identified ARGs [8].
5. Normalization and Comparative Analysis: * Apply a consistent normalization strategy across all samples within a study. Based on current evidence, start with a batch correction method (e.g., BMC, Limma) if combining datasets from different batches or studies [88] [89]. * For cross-study comparisons, carefully select a normalization method from Table 1 that is robust to the expected heterogeneity, and document this choice explicitly.
The following workflow diagram summarizes the key steps in the standardized mNGS pipeline for AMR analysis, highlighting the major standardization hurdles encountered throughout the process.
Diagram: mNGS Workflow and Key Standardization Hurdles in AMR Analysis. This diagram outlines the sequential steps in a typical mNGS pipeline for antimicrobial resistance research, with associated standardization challenges highlighted at each major stage.
Table 2: Key Research Reagent Solutions for mNGS-based AMR Studies
| Category | Item | Function/Application |
|---|---|---|
| Wet-Lab Reagents | QIAamp Fast DNA Stool Mini Kit (Qiagen) | DNA extraction from complex samples like stool, crucial for gut microbiome resistome studies [10]. |
| PowerSoil DNA Isolation Kit (MO BIO) | DNA extraction from environmental samples (soil, sediment) which are key reservoirs of ARGs [10]. | |
| Illumina DNA Prep | A flexible and user-friendly library preparation kit for a wide range of inputs, including microbial DNA [41]. | |
| Illumina MiSeq System | A widely used NGS platform for mid-throughput metagenomic sequencing, suitable for resistome profiling [10] [41]. | |
| Bioinformatics Tools & Databases | MetaPhlAn | For taxonomic profiling of microbial communities from metagenomic shotgun sequencing data [10]. |
| CARD (Comprehensive Antibiotic Resistance Database) | A curated resource containing ARG sequences, ontologies, and associated metadata for resistance gene detection [8] [41]. | |
| Bowtie 2 | A fast and memory-efficient tool for aligning sequencing reads to reference databases (e.g., for host removal or ARG alignment) [86]. | |
| SPAdes | A toolkit for de novo genome assembly, which can be applied to metagenomic data to reconstruct contigs for ARG and MGE discovery [14]. |
Achieving reproducible mNGS pipelines for AMR analysis requires a concerted effort to standardize both wet-lab and bioinformatics practices. Key hurdles include variability in sample processing, host DNA depletion, choice of sequencing platforms, and the selection of bioinformatic tools, databases, and normalization methods. By adopting the detailed protocols and standardized resources outlined in this application note—such as consistent DNA extraction kits, robust normalization strategies like batch correction, and curated ARG databases—researchers can enhance the reliability and comparability of their findings. Overcoming these hurdles is paramount for advancing our understanding of resistome dynamics and for developing effective public health strategies to combat the global threat of antimicrobial resistance.
Benchmarking mNGS: Performance Validation Against Gold Standards
The rapid and accurate identification of pathogens and their antimicrobial resistance profiles is a cornerstone of effective infectious disease management. Traditional culture-based methods and antimicrobial susceptibility testing (AST) have long been the gold standard but face limitations including prolonged turnaround times and reduced sensitivity in patients with prior antibiotic exposure [91] [92]. Metagenomic next-generation sequencing (mNGS) has emerged as a powerful, culture-independent diagnostic tool that can simultaneously detect pathogens and characterize their resistance genes directly from clinical samples [93] [94]. This application note provides a comprehensive comparison of the sensitivity and specificity of mNGS versus conventional culture and AST, with specific focus on analyzing antimicrobial resistance genes (ARGs) within the broader context of antimicrobial resistance research.
Comparative Diagnostic Performance
Multiple clinical studies across diverse patient populations and sample types have demonstrated that mNGS exhibits significantly higher sensitivity but somewhat lower specificity compared to traditional culture methods.
Table 1: Comparative Diagnostic Performance of mNGS vs. Culture
| Study Population | Sample Size | Sensitivity (mNGS vs. Culture) | Specificity (mNGS vs. Culture) | Reference |
|---|---|---|---|---|
| Febrile patients with suspected infections | 368 | 58.01% vs. 21.65% (p<0.001) | 85.40% vs. 99.27% (p<0.001) | [91] |
| Patients with fever of unknown origin (FUO) | 263 | 81.52% vs. 47.28% | 73.42% vs. 84.81% | [95] |
| Critically ill patients supported by ECMO | 62 | 79.6% positive rate vs. 30.4% | Not specified | [96] |
| Various clinical specimens | 134 | 74.2% vs. 57.8% (p<0.001) | Not specified | [94] |
The superior sensitivity of mNGS is particularly evident in challenging clinical scenarios. For instance, in patients with prior antibiotic exposure, mNGS maintains its detection capability while culture performance significantly declines. One study reported statistically significant higher detection rates for mNGS versus culture in puncture fluid (p=0.000) and tissue samples (p=0.000) from patients who had received antibiotics before testing [91].
Impact on Clinical Decision-Making
The enhanced sensitivity of mNGS directly translates to improved clinical management. Among 368 febrile patients with suspected infections, 64 patients with positive mNGS results received adjusted antibiotic therapy, including treatment transitions, antibiotic downgrading, and combination therapy. Notably, 21 patients had a definitive treatment turning point based on mNGS findings, leading to recovery and discharge due to timely antibiotic adjustment [91]. In a separate study of 263 patients with fever of unknown origin, the clinical management of 48.67% (128/263) patients was positively affected by mNGS results [95].
Antimicrobial Resistance Gene Detection
mNGS for Resistance Profiling
mNGS enables comprehensive detection of antibiotic resistance genes (ARGs), providing valuable insights for antimicrobial stewardship. Studies have demonstrated strong consistency between ARG detection and phenotypic resistance profiles.
Table 2: Antibiotic Resistance Gene Detection by mNGS
| Pathogen | Resistance Genes | Consistency with Phenotypic AST | Clinical Application | Reference |
|---|---|---|---|---|
| Acinetobacter baumannii | ade genes (adeA, adeB, adeC, adeS, adeR) | 100% (13/13 cases) | Epidemic strain tracking | [94] |
| Acinetobacter baumannii | sul2, APH(3")-Ib | 91.6% (12/13 cases) | Predict sulfonamide and aminoglycoside resistance | [94] |
| Staphylococcus aureus | Machine learning-selected minimal features for 18 antibiotics | 81.82%-100% accuracy in clinical samples | Reduced diagnostic time by ~40 hours | [93] |
A study analyzing Acinetobacter baumannii detected by both mNGS and culture found that ade genes (adeA, adeB, adeC, adeS, adeR) were the most frequently detected ARGs, showing 100% consistency with phenotypic resistance patterns. Similarly, sul2 and APH(3")-Ib genes demonstrated 91.6% consistency with corresponding resistance phenotypes [94].
Advanced Genotypic AST Prediction
Recent advances in machine learning approaches have further enhanced the capability of mNGS for predicting antimicrobial susceptibility. Researchers have developed interpretable genotypic AST models for Staphylococcus aureus that leverage minimal genomic determinants identified through analysis of 4,796 S. aureus genomes and AST data for 18 antibiotics [93].
This rule-based model achieved remarkable accuracy with area under the curve (AUC) values ranging from 0.94 to 1.00 for different antibiotics, with an overall sensitivity of 97.43% and specificity of 99.02%. When applied directly to clinical metagenomic samples, the model achieved 81.82% to 100% accuracy in AST predictions while bypassing the need for bacterial isolation and reducing diagnostic time by an average of 39.9 hours [93].
Methodological Protocols
Standard mNGS Wet-Lab Workflow
The following diagram illustrates the comprehensive workflow for mNGS-based pathogen detection and resistance gene analysis:
Sample Collection and Processing
Clinical samples (blood, BALF, tissue, CSF, etc.) are collected aseptically. Blood samples (≥5mL) are collected in cell-free DNA storage tubes containing EDTA and DNA protective agents, stored and transported at room temperature. BALF or pleural fluid samples (≥5mL) and sputum, CSF or other body fluids (1-3mL) are collected in dry sterile tubes for cryopreservation and transported on dry ice [91] [94]. All suspected infectious samples are inactivated by 56°C water bath for 30 minutes before nucleic acid extraction [94].
DNA Extraction and Library Preparation
DNA extraction is performed using commercial kits such as the QIAamp DNA Micro Kit (QIAGEN) or HostZERO Microbial DNA Kit (ZYMO RESEARCH) following manufacturer's instructions [91] [94]. For blood samples, cell-free DNA is extracted using specialized kits like HiPure circulating DNA MIDI kit (Magen) after centrifugation at 1600g for 10 minutes at 4°C to separate plasma [94]. DNA libraries are constructed using transposase-based methods such as the Nextera XT kit (Illumina) or Kapa hyper plus library preparation kit [91] [94]. Library quality is assessed using Agilent 2100 Bioanalyzer for fragment size distribution and Qubit fluorometer for concentration measurement [91].
Sequencing
Qualified libraries are sequenced on platforms such as Illumina NextSeq 550, NextSeq 550Dx, or similar systems, generating single-end or paired-end reads [91] [95] [94]. Typically, 20-30 million reads per sample are generated to ensure sufficient depth for microbial detection [91] [36]. Each sequencing run includes negative controls (no-template water) and positive controls (clinical samples with known pathogens) to monitor contamination and workflow performance [94].
Bioinformatics Analysis
Data Preprocessing and Host Depletion
Raw sequencing data undergoes quality control using tools like fastp (v0.19.5) to remove adapter sequences, low-quality reads (Q30<75%), and short sequences (<35bp) [95] [94]. Human sequence reads are identified and removed by alignment to reference genomes (hg38 or GRCh38) using Burrows-Wheeler Aligner (BWA) or Bowtie2 [91] [95]. The remaining microbial reads are retained for downstream analysis.
Microbial Identification
Processed reads are aligned against comprehensive microbial genome databases using various approaches. Some pipelines use marker-based alignment with software like MetaPhlAn2, which leverages unique marker sequences for each species [94]. Other approaches employ whole-genome alignment with tools like Kraken or SNAP against curated databases containing bacterial, fungal, viral, and parasitic genomes [91] [94]. Positive identification typically requires meeting thresholds based on standardized metrics such as SMRN (specifically mapped read number) or RPM (reads per million) [95].
Antimicrobial Resistance Gene Analysis
For ARG detection, sequencing reads are aligned against resistance databases such as CARD (Comprehensive Antimicrobial Resistance Database) using BLAST with stringent criteria (similarity identity ≥90%, length >70bp) [93] [94]. Advanced approaches employ machine learning-selected minimal feature sets for specific pathogen-antibiotic combinations, enabling rule-based resistance prediction [93].
The Scientist's Toolkit
Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for mNGS-Based AMR Analysis
| Reagent/Solution | Function | Example Products |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of microbial DNA/RNA from clinical samples | QIAamp DNA Micro Kit, HostZERO Microbial DNA Kit, TIANamp Micro DNA Kit |
| Library Preparation Kits | Construction of sequencing libraries | Nextera XT Kit, Kapa Hyper Plus Kit, QIAseq Ultralow Input Library Kit |
| Host DNA Depletion Reagents | Reduction of human background to enhance microbial detection | Benzonase, Tween20, Ribo-Zero rRNA Removal Kit |
| Sequencing Kits | Generation of sequencing data on platforms | Illumina NextSeq 500/550 kits, MiniSeq reagents |
| Positive Control Materials | Quality assurance for entire workflow | Characterized clinical samples with known pathogens |
| Negative Control Materials | Contamination monitoring during processing | Sterile deionized water, peripheral blood mononuclear cells from healthy donors |
Discussion and Future Perspectives
The integration of mNGS into clinical microbiology workflows represents a paradigm shift in diagnostic approaches, particularly for challenging cases such as febrile illnesses of unknown origin, culture-negative infections, and complex polymicrobial infections. The significantly higher sensitivity of mNGS compared to culture (58.01% vs. 21.65% in febrile patients) must be balanced against its somewhat lower specificity (85.40% vs. 99.27%) [91]. This trade-off necessitates careful clinical interpretation of mNGS results within the context of patient symptoms, history, and other diagnostic findings.
The ability of mNGS to detect antimicrobial resistance genes directly from clinical samples provides a powerful complement to traditional AST. While phenotypic AST remains essential for assessing actual resistance expression, genotypic resistance profiling by mNGS offers significantly faster results (reducing diagnostic time by approximately 40 hours) and can detect resistance mechanisms that might be missed by conventional methods [93]. The development of machine learning-based models that identify minimal genomic determinants for resistance prediction represents a major advancement toward interpretable and clinically actionable genotypic AST [93].
Future directions in this field include the standardization of wet-lab and bioinformatics protocols across laboratories, establishment of validated clinical interpretation guidelines, and refinement of resistance prediction algorithms through expanded training datasets. Additionally, the integration of mNGS with other technologies such as long-read sequencing and transcriptomics may further enhance our understanding of resistance mechanisms and microbial behavior in clinical settings.
As mNGS technologies continue to evolve and become more accessible, their role in antimicrobial resistance research and clinical management is poised to expand, ultimately contributing to more personalized and effective antimicrobial therapies.
Antimicrobial resistance (AMR) poses a critical global health threat, with bacterial AMR alone causing an estimated 1.14 million deaths annually [97]. The rapid and accurate identification of resistant pathogens is essential for effective treatment and antimicrobial stewardship. Traditional phenotypic susceptibility testing (PST), while considered the gold standard, requires bacterial culture and typically takes 2-5 days, leading to delays in targeted therapy [5] [98].
Metagenomic next-generation sequencing (mNGS) offers a culture-independent approach that can simultaneously detect pathogens and resistance genes directly from clinical samples [5] [99]. However, the concordance between mNGS-based genotypic resistance prediction and conventional phenotypic results varies significantly across pathogens, antibiotics, and technical approaches. This application note synthesizes current evidence on this concordance and provides detailed protocols for implementing mNGS-AMR analysis.
The predictive performance of mNGS for antimicrobial resistance varies substantially across different antibiotic classes, bacterial species, and specimen types. The tables below summarize key performance metrics from recent clinical studies.
Table 1: Overall performance of mNGS for AMR prediction in respiratory infections
| Patient Population | Specimen Type | Sensitivity Range | Specificity Range | Key Predictors | Reference |
|---|---|---|---|---|---|
| Pediatric severe pneumonia (n=120) | BALF | 28.6%-100%* | 64%-95%* | Carbapenem resistance genes | [5] |
| Critically ill adults with LRTI (n=27) | BALF, TA | 70%-100% | 64%-95% | Combination of RNA+DNA sequencing | [99] |
| Patients with A. baumannii (n=230) | Clinical specimens | 97.7%-98.4%* | 97.7%-98.4%* | Machine learning model with 20-31 genetic features | [98] |
*Varies by antibiotic class; Varies by gram stain category; *Varies by antibiotic
Table 2: Performance of mNGS for predicting resistance to specific antibiotic classes
| Antibiotic Class | Sensitivity | Specificity | Pathogens | Study |
|---|---|---|---|---|
| Carbapenems | 67.7%-94.7% | 85.7% | Acinetobacter baumannii, Enterobacterales | [5] [98] |
| Cephalosporins | 46.2% | 75.0% | Mixed respiratory pathogens | [5] |
| Penicillins | 28.6% | 75.0% | Mixed respiratory pathogens | [5] |
| Fluoroquinolones | 98.4%* | 98.4%* | Acinetobacter baumannii | [98] |
*Using machine learning model
Experimental Protocols for mNGS-AMR Analysis
Sample Processing and Library Preparation
The following protocol is adapted from Gan et al. (2024) and Chen et al. (2023) for BALF samples [5] [98]:
Sample Preprocessing:
- Centrifuge 1 mL BALF at 12,000 × g for 5 minutes to collect microorganisms and human cells
- Resuspend precipitate in 50 μL and perform host nucleic acid depletion using:
- 1 U Benzonase (Sigma)
- 0.5% Tween 20 (Sigma)
- Incubate at 37°C for 5 minutes
- Stop reaction with 400 μL terminal buffer
Nucleic Acid Extraction:
- Transfer 600 μL mixture to tubes with 500 μL ceramic beads
- Perform bead beating using Minilys Personal Homogenizer (Tiangen, China)
- Extract DNA from 400 μL pretreated samples using QIAamp UCP Pathogen Mini Kit (Qiagen)
- Elute in 60 μL elution buffer
- For RNA extraction: Use QIAamp Viral RNA Kit (Qiagen)
- Remove ribosomal RNA using Ribo-Zero rRNA Removal Kit (Illumina)
- Synthesize cDNA using reverse transcriptase and dNTPs (Thermo Fisher Scientific)
Library Preparation and Sequencing:
- Construct DNA/cDNA libraries using KAPA low throughput library construction kit (KAPA Biosystems)
- Use 750-ng library per sample for hybrid capture-based enrichment with microbial probes (SeqCap EZ Library, Roche)
- Probes designed using CATCH pipeline with default parameters based on pathogen genomes and resistance genes
- Assess library quality using Qubit dsDNA HS Assay kit and Agilent 2100 Bioanalyzer
- Sequence on Illumina Nextseq CN500 for 75 cycles single-end, generating ~20 million reads per library
Quality Control:
- Include internal controls: DNA phage (E. coli bacteriophage T1) and RNA phage (E. coli bacteriophage MS2) at 10^4 copies/mL
- Process negative controls (Hela cells and sterile deionized water) with each batch
Bioinformatics Analysis
Primary Data Processing:
- Perform deduplication, trimming, and quality filtering of raw reads
- Align trimmed reads to human reference genome (hg38) using Burrows-Wheeler Aligner or STAR aligner to remove human sequences
- For pathogen detection: Use Centrifuge (v1.0.3) or ID-Seq pipeline for taxonomic classification
AMR Gene Detection:
- Identify AMR genes using SRST2 coupled with expanded ARG-ANNOT database
- Include genes with ≥5% allele coverage in analysis
- For Streptococcus pneumoniae: Screen for point mutations in pbp genes associated with beta-lactam resistance using CARD resistance gene identifier with 'loose' setting
- Calculate normalized read depth (depth per million reads sequenced, dpM) for each allele
Machine Learning Enhancement (Optional):
- For enhanced prediction, implement LASSO regression model to identify key genetic features associated with resistance
- Train model on known genotype-phenotype correlations
- Apply model to mNGS data to predict resistance probabilities [98]
Figure 1: Complete workflow for mNGS-based antimicrobial resistance prediction, from sample collection to result validation.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key research reagent solutions for mNGS-AMR analysis
| Category | Product/Platform | Manufacturer | Application in mNGS-AMR |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp UCP Pathogen Mini Kit | Qiagen | Simultaneous extraction of DNA and RNA from difficult samples |
| Host Depletion | Benzonase | Sigma | Digestion of host nucleic acids to increase microbial sequencing depth |
| Library Preparation | KAPA Low Throughput Library Construction Kit | KAPA Biosystems | High-quality library prep for low-input clinical samples |
| Target Enrichment | SeqCap EZ Library | Roche | Hybrid capture-based enrichment of microbial and AMR gene targets |
| Sequencing Platforms | Illumina Nextseq CN500 | Illumina | High-accuracy sequencing for resistance variant detection |
| MinION | Oxford Nanopore | Long-read sequencing for resolving complex resistance loci | |
| Bioinformatics Tools | SRST2 | N/A | AMR gene detection from short-read sequencing data |
| CARD RGI | N/A | Comprehensive antibiotic resistance database and analysis | |
| ARG-ANNOT | N/A | Annotated antibiotic resistance gene database |
Critical Factors Influencing Concordance
Technical Considerations
The concordance between mNGS-predicted and phenotypic AMR is influenced by several technical factors:
Nucleic Acid Type: Combined DNA and RNA sequencing significantly improves performance for gram-positive bacteria (70% sensitivity, 95% specificity) compared to DNA-only approaches [99].
Sequencing Depth: Detection of low-abundance resistance genes requires sufficient sequencing depth (>20 million reads for respiratory samples) [5]. CRISPR/Cas9 enrichment (FLASH) can enhance detection of low-abundance AMR genes by >2500-fold [99].
Bioinformatic Analysis: Hybrid assembly approaches combining long-read and short-read data produce the highest quality genomes for AMR gene detection, though with increased computational requirements [100].
Biological and Clinical Considerations
Resistance Mechanisms: mNGS excels at detecting acquired resistance genes but may miss chromosomal mutations or novel mechanisms [14]. The technology shows highest concordance for carbapenem resistance in Gram-negative pathogens where mechanisms are well-characterized [5] [98].
Gene Expression: Detection of resistance genes does not necessarily indicate expression at protein level, creating potential genotype-phenotype discordance [14] [100].
Polymicrobial Infections: mNGS provides advantage in mixed infections where culture-based methods may miss fastidious organisms, but assigning resistance genes to specific pathogens remains challenging [99].
mNGS shows promising but variable concordance with phenotypic AST, performing best for specific pathogen-drug combinations such as carbapenem resistance in A. baumannii. Current evidence suggests mNGS cannot yet replace conventional PST but serves as a valuable supplementary tool that provides more rapid results (19.1 hours versus 63.3 hours for culture-based AST) [98].
Future developments including machine learning integration, standardized bioinformatic pipelines, and Cas9-based enrichment technologies are likely to improve concordance. For clinical implementation, laboratories should validate mNGS-AMR predictions against phenotypic methods for their specific patient populations and resistance patterns of local relevance.
Rapid pathogen identification is a cornerstone of effective clinical diagnostics and antimicrobial resistance (AMR) research. Traditional culture-based methods, while considered a gold standard, are often slow, with time to results ranging from hours to days, and are compromised by prior antibiotic use and the presence of fastidious or non-culturable organisms [101] [102]. Metagenomic Next-Generation Sequencing (mNGS) offers a culture-independent, high-throughput solution that can significantly accelerate pathogen and antimicrobial resistance gene (ARG) detection. This Application Note provides a comparative analysis of the turnaround times (TAT) of mNGS versus traditional culture, supplemented with detailed protocols and workflow visualizations to guide researchers and drug development professionals in the analysis of AMR genes.
Quantitative Comparison of Turnaround Times
The following table summarizes key quantitative data from recent studies, directly comparing the turnaround times of different diagnostic methods.
Table 1: Comparative Turnaround Times of Pathogen Detection Methods
| Method | Reported Turnaround Time (TAT) | Key Context / Sample Type | Citation |
|---|---|---|---|
| Traditional Microbial Culture | 15.1 ± 10.4 hours (Time to Positive Culture) | Neurosurgical Central Nervous System Infections (NCNSIs) | [101] |
| 22.6 ± 9.4 hours (Time from Sample to Final Result) | Neurosurgical Central Nervous System Infections (NCNSIs) | [101] | |
| 7 to 21 days (Standard vs. Extended Protocol) | Periprosthetic Joint Infection (PJI); extended duration did not improve yield | [102] | |
| Metagenomic NGS (mNGS) | 20 hours (Full Workflow) | Lower Respiratory Tract Infections | [36] |
| 16.8 ± 2.4 hours (Time from Sample to Final Result) | Neurosurgical Central Nervous System Infections (NCNSIs) | [101] | |
| Droplet Digital PCR (ddPCR) | 12.4 ± 3.8 hours (Time from Sample to Final Result) | Neurosurgical Central Nervous System Infections (NCNSIs); significantly faster than mNGS | [101] |
| Targeted NGS (tNGS) | Shorter than mNGS (implied) | Lower Respiratory Tract Infections; noted as an alternative for rapid results | [36] |
The data unequivocally demonstrates that mNGS offers a substantial speed advantage over traditional culture, reducing wait times from days to under 24 hours. In a direct comparative study on NCNSIs, mNGS provided results 5.8 hours faster than the final culture results on average [101]. It is also important to note that while culture can sometimes yield positive results in under 24 hours, the time-to-final-result—which includes the period until a culture is declared negative—is a more clinically relevant metric and is significantly longer for culture-based approaches [101] [102].
Detailed Experimental Protocols
To ensure reproducibility and provide a clear framework for implementation, detailed protocols for mNGS and traditional culture are outlined below.
Protocol for Metagenomic Next-Generation Sequencing (mNGS)
This protocol is adapted from studies on lower respiratory tract and neurosurgical infections [36] [101] [103].
Sample Collection and Pre-processing:
- Collect 1-10 mL of sample (e.g., Bronchoalveolar Lavage Fluid - BALF, Cerebrospinal Fluid - CSF) into a sterile container.
- Centrifuge the sample at 12,000 × g for 5 minutes to pellet cells and potential pathogens.
- Host Depletion (Critical for human samples): Resuspend the pellet in a mixture of 1 U Benzonase and 0.5% Tween 20. Incubate at 37°C for 5 minutes to degrade human nucleic acids and lyse cells [103].
Nucleic Acid Extraction:
- Extract total nucleic acid using a commercial kit, such as the QIAamp UCP Pathogen DNA Kit or MagPure Pathogen DNA/RNA Kit, following the manufacturer's instructions [36].
- For comprehensive pathogen detection, parallel RNA extraction can be performed using the QIAamp Viral RNA Kit, followed by ribosomal RNA depletion [36].
Library Preparation and Sequencing:
- DNA Library Construction: Use a library preparation system like the Ovation Ultralow System V2. Fragment the DNA, add sequencing adapters, and amplify the library via PCR [36].
- RNA Library Construction: Reverse transcribe RNA into cDNA, then proceed with library construction as for DNA.
- Quality Control: Quantify the final library concentration using a fluorometer (e.g., Qubit).
- Sequencing: Load the library onto a sequencer such as the Illumina NextSeq 550Dx for 75-bp single-end sequencing, aiming for approximately 20 million reads per sample [36].
Bioinformatic Analysis:
- Data Pre-processing: Use software like Fastp to remove adapter sequences, ambiguous nucleotides, and low-quality reads.
- Host Sequence Removal: Map reads to a human reference genome (e.g., hg38) using tools like Burrows-Wheeler Aligner (BWA) and remove matching sequences.
- Microbial Identification and ARG Detection: Align non-host reads to comprehensive genomic databases (e.g., RefSeq, GenBank) containing bacterial, viral, fungal, and parasitic sequences, as well as databases of known AMR genes [36] [8]. Tools like MetaPhlAn are also used for taxonomic profiling [10].
Protocol for Traditional Culture and Antimicrobial Susceptibility Testing (AST)
This protocol is standardized for samples from sterile sites like CSF and periprosthetic tissue [101] [102].
Sample Inoculation:
- Inoculate samples directly onto solid culture media (e.g., Columbia blood agar) for aerobic and anaerobic culture.
- Simultaneously, inoculate samples into liquid enrichment broth, such as BACTEC Plus aerobic and anaerobic blood culture vials.
- Incubate the vials in an automated continuous-monitoring blood culture system (e.g., BACTEC 9050) [102].
Culture Monitoring and Sub-culturing:
- Monitor liquid cultures continuously for a minimum of 5-7 days. For cases of suspected low-virulence organisms, this can be extended to 14-21 days, though this may not significantly improve yield [102].
- Any vial signaling positive is immediately Gram-stained and sub-cultured onto solid media to obtain isolated colonies for further identification.
- Solid media plates are inspected daily for growth for up to 7 days.
Pathogen Identification and AST:
- Isolated colonies are identified using matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry or biochemical tests.
- Antimicrobial Susceptibility Testing (AST) is performed on confirmed pathogens using methods like disk diffusion (Kirby-Bauer) or broth microdilution in automated systems (e.g., VITEK 2) to determine Minimum Inhibitory Concentrations (MICs) [8].
Workflow Visualization
The following diagram illustrates the parallel workflows of mNGS and traditional culture, highlighting the significant divergence in TAT.
Diagram 1: Comparative mNGS vs Culture Workflow and Timelines
The Scientist's Toolkit: Key Research Reagent Solutions
Successful execution of mNGS for AMR research relies on specific reagents and kits. The following table details essential solutions.
Table 2: Essential Research Reagents for mNGS-based AMR Analysis
| Product Category | Example Product | Primary Function in Workflow |
|---|---|---|
| Nucleic Acid Extraction | QIAamp UCP Pathogen DNA Kit (Qiagen) | High-quality DNA extraction from complex samples while minimizing contamination. |
| PowerSoil DNA Isolation Kit (MO BIO) | Standardized DNA extraction from environmental and difficult soil-like samples. | |
| Host Depletion | Benzonase (Sigma) | Enzymatic degradation of host (e.g., human) DNA and RNA to increase microbial sequencing depth. |
| Library Preparation | Ovation Ultralow System V2 (NuGEN) | Construction of sequencing libraries from low-input or degraded nucleic acid samples. |
| Illumina DNA Prep (Illumina) | A fast, user-friendly library preparation solution for a wide range of input DNA. | |
| Targeted Enrichment | Respiratory Pathogen ID/AMR Enrichment Panel (Illumina) | Probe-based enrichment of specific respiratory pathogens and AMR genes for highly sensitive detection. |
| AmpliSeq for Illumina Antimicrobial Resistance Panel (Illumina) | Amplification-based targeted sequencing of 478 AMR genes across 28 antibiotic classes. | |
| Bioinformatics Tools | MetaPhlAn (MetaGenomic Phylogenetic Analysis) | For taxonomic profiling of microbial communities from metagenomic shotgun sequencing data. |
| Custom AMR Databases (e.g., from NCBI) | Curated databases of known ARGs used as a reference for aligning sequences to identify resistance determinants. |
The comparative data and protocols presented herein establish mNGS as a superior methodological choice over traditional culture when turnaround time is a critical factor in AMR research and diagnostics. The ability of mNGS to deliver comprehensive pathogen and ARG profiles within a single day [36] [101] enables a more rapid research response, whether for tracking resistance transmission [10] [41] or investigating outbreak dynamics.
A key advantage of mNGS in the AMR context is its capacity to detect ARGs directly from complex samples, including those from non-culturable organisms, and to link them to mobile genetic elements (MGEs) like plasmids and transposons [8] [10]. This provides deep insights into the horizontal gene transfer dynamics that drive the spread of resistance, a dimension completely missed by culture-based AST.
While the initial cost of mNGS is higher [36], its speed, comprehensiveness, and ability to guide targeted therapeutic and public health interventions earlier present a compelling value proposition. For research and drug development focused on antimicrobial resistance, integrating mNGS into surveillance and discovery pipelines is not just an incremental improvement but a transformative step towards understanding and mitigating this global health threat.
The accurate and timely identification of pathogens in body fluids is a critical step in the diagnosis and treatment of infectious diseases, particularly in the context of rising antimicrobial resistance (AMR). Traditional culture-based methods, while considered a gold standard, are often slow and have limited sensitivity for fastidious or slow-growing microorganisms [44]. Metagenomic next-generation sequencing (mNGS) has emerged as a powerful, culture-independent tool capable of comprehensive pathogen detection. This Application Note provides a detailed comparative analysis of three primary NGS approaches used for pathogen identification in body fluids: whole-cell DNA mNGS (wcDNA mNGS), cell-free DNA mNGS (cfDNA mNGS), and 16S ribosomal RNA gene next-generation sequencing (16S rRNA NGS). Framed within the critical context of AMR gene analysis, this document summarizes key performance data, outlines standardized experimental protocols, and visualizes core workflows to support researchers and drug development professionals in selecting and implementing the most appropriate methodology for their specific applications.
The choice between wcDNA mNGS, cfDNA mNGS, and 16S rRNA NGS involves trade-offs between sensitivity, specificity, and the type of information yielded. The following tables summarize key quantitative findings from recent studies to facilitate comparison.
Table 1: Overall Diagnostic Performance of NGS Methodologies in Body Fluids
| Performance Metric | wcDNA mNGS | cfDNA mNGS | 16S rRNA NGS |
|---|---|---|---|
| Sensitivity (vs. Culture) | 74.1% [44] | 62.1% (for BSI) [104] | 58.5% (vs. culture) [44] |
| Specificity (vs. Culture) | 56.3% [44] | 57.1% (for BSI) [104] | Information Not Provided |
| Concordance with Culture | 63.3% [44] | 46.7% [44] | Information Not Provided |
| Host DNA Proportion | ~84% [44] | ~95% [44] | Not Applicable |
| Key Strengths | Higher sensitivity for bacterial detection; captures genomic DNA from intact cells [44] | Superior for low-load fungi, viruses, and intracellular pathogens; less affected by live organism viability [42] | Cost-effective; reduced host DNA interference; good for bacterial genus-level identification [104] |
| Key Limitations | Lower specificity; may miss non-viable or cell-free pathogens [44] | Lower specificity; may not detect all Gram-positive bacteria; highly fragmented DNA [104] [105] | Limited resolution for species-level identification; misses non-bacterial pathogens [44] |
Table 2: Performance in Predicting Antimicrobial Resistance
| Aspect | mNGS Performance | Notes |
|---|---|---|
| Overall AMR Prediction | Variable performance; cannot replace conventional Phenotypic Susceptibility Testing (PST) [5]. | Performance is highly dependent on the pathogen and antibiotic class. |
| Sensitivity (Gram-positive bacteria) | 70% (with RNA+DNA mNGS) [99]. | |
| Sensitivity (Gram-negative bacteria) | 100% (with RNA+DNA mNGS) [99]. | |
| Specificity (Gram-positive bacteria) | 95% (with RNA+DNA mNGS) [99]. | |
| Specificity (Gram-negative bacteria) | 64% (with RNA+DNA mNGS) [99]. | |
| Carbapenem Resistance Sensitivity | 67.7% (overall); 94.7% for Acinetobacter baumannii [5]. | Higher than for penicillins and cephalosporins. |
| Utility | Effective for epidemiological AMR surveillance; can be enhanced with targeted enrichment [99]. | CRISPR/Cas9 enrichment can detect low-abundance AMR genes [99]. |
Experimental Protocols
This section details standardized protocols for the preparation and analysis of body fluid samples using the three NGS methodologies, with a focus on generating data suitable for AMR gene analysis.
Sample Collection and Pre-processing
- Sample Types: The protocols are applicable to diverse body fluids, including bronchoalveolar lavage fluid (BALF), cerebrospinal fluid (CSF), pleural fluid, ascites, and preservation or drainage fluids [44] [42] [106].
- Initial Handling: Collect samples in sterile containers. For wcDNA and 16S rRNA NGS, aliquot a portion of the unprocessed sample for nucleic acid extraction.
- cfDNA Separation: For cfDNA mNGS, centrifuge the sample at high speed (e.g., 20,000 × g for 15 minutes) to pellet cells and debris [44]. Carefully transfer the supernatant to a new tube for subsequent cfDNA extraction. The pellet can be retained for parallel wcDNA analysis.
Nucleic Acid Extraction
Table 3: Nucleic Acid Extraction Protocols
| Method | Starting Material | Extraction Kit (Example) | Critical Steps |
|---|---|---|---|
| wcDNA Extraction | Body fluid pellet or uncentrifuged sample [42]. | Qiagen DNA Mini Kit [44]. | Incorporate a mechanical lysis step (e.g., bead beating) for robust disruption of microbial cells [44]. |
| cfDNA Extraction | Cell-free supernatant from pre-centrifuged sample [42] [106]. | QIAamp DNA Micro Kit [42] [106] or VAHTS Free-Circulating DNA Maxi Kit [44]. | Handle supernatant carefully to avoid disturbing the pellet; use carrier RNA if recommended to improve yield of low-concentration cfDNA. |
| 16S rRNA Gene DNA Extraction | Body fluid pellet or uncentrifuged sample. | PowerSoil DNA Isolation Kit [10] or QIAamp DNA Stool Mini Kit (for fecal samples) [10]. | Ensure complete lysis of Gram-positive bacteria; the extraction method should be consistent across samples to avoid bias. |
Library Preparation and Sequencing
- mNGS Library (wcDNA & cfDNA):
- Fragmentation: Fragment DNA to an average size of 200-500 bp using mechanical or enzymatic methods [104]. Note that cfDNA is already naturally fragmented.
- Library Prep Kit: Use a kit designed for low-input DNA, such as the VAHTS Universal Pro DNA Library Prep Kit for Illumina [44] [104] or the KAPA low throughput library construction kit [5].
- Sequencing: Sequence on an Illumina platform (e.g., NovaSeq or NextSeq) to generate 20-50 million paired-end reads (e.g., 2x150 bp) per sample [44] [5].
- 16S rRNA NGS Library:
- Targeted Amplification: Amplify the hypervariable regions (e.g., V3-V4) of the 16S rRNA gene using universal primers (e.g., 341F and 806R) [44] [104].
- Library Prep: Clean up the PCR amplicons and attach sequencing adapters and indices.
- Sequencing: Sequence on an Illumina platform (e.g., MiSeq or NovaSeq) with 2x250 bp paired-end reads to adequately cover the amplicon [44].
Bioinformatic Analysis for Pathogen and AMR Gene Detection
- Quality Control and Host Depletion: Process raw reads with tools like Fastp to remove adapters and low-quality sequences [104]. Align reads to a human reference genome (e.g., hg38) using Bowtie2 or BWA and remove matching reads [42] [106].
- Taxonomic Profiling:
- mNGS: Classify non-host reads using a taxonomic classifier such as Kraken2 against a curated microbial genome database [104] or align to NCBI NT/NR databases using tools like BLAST.
- 16S rRNA NGS: Process reads with a pipeline like QIIME 2 or DADA2 to denoise, cluster into Amplicon Sequence Variants (ASVs) or Operational Taxonomic Units (OTUs), and assign taxonomy using a reference database (e.g., SILVA) [10].
- AMR Gene Identification: Analyze quality-controlled, non-host mNGS reads using specialized tools like SRST2 [99] or the Resistance Gene Identifier (RGI) from the Comprehensive Antibiotic Resistance Database (CARD) [99]. For 16S rRNA NGS, AMR gene prediction is not possible due to the targeted nature of the assay.
Workflow Visualization
The following diagram illustrates the parallel pathways for processing body fluid samples via the three NGS methodologies, highlighting key decision points and procedural differences.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Kits for NGS-Based Pathogen Detection
| Item | Function/Application | Example Products |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA from various sample matrices. | QIAamp DNA Mini & Micro Kits (Qiagen) [44] [42], PowerSoil DNA Isolation Kit (Mo Bio) [10]. |
| NGS Library Preparation Kits | Construction of sequencing-ready libraries from low-input DNA. | VAHTS Universal Pro DNA Library Prep Kit (Vazyme) [44] [104], KAPA HyperPrep Kit (Roche). |
| 16S rRNA PCR Primers | Amplification of hypervariable regions for taxonomic profiling. | 341F / 806R (targeting V3-V4 region) [104]. |
| Probe-Based Enrichment Systems | Targeted enrichment of microbial sequences or AMR genes to improve sensitivity. | CRISPR/Cas9-based enrichment (e.g., FLASH) [99]. |
| Host Depletion Reagents | Selective removal of human nucleic acids to increase microbial sequencing depth. | Benzonase treatment [5]; Micronbrane's Devin Microbial DNA Enrichment Kit [105]. |
| Bioinformatics Databases | Reference databases for taxonomic classification and AMR gene identification. | NCBI NT/NR, Kraken2 databases, CARD, ARG-ANNOT [99]. |
The early and accurate identification of pathogens is fundamental to effective treatment of infectious diseases. However, conventional, culture-based diagnostic methods frequently fail to detect fastidious or non-culturable pathogens, leading to delayed or inappropriate antimicrobial therapy. This diagnostic gap contributes significantly to the global antimicrobial resistance (AMR) crisis. Metagenomic Next-Generation Sequencing (mNGS) represents a paradigm shift, offering a culture-independent, hypothesis-free approach to pathogen detection. This Application Note details a validated mNGS workflow for comprehensive identification of fastidious pathogens and their associated antimicrobial resistance genes (ARGs), providing a powerful tool for enhancing patient outcomes and strengthening AMR surveillance.
Clinical Significance and Performance
Ventilator-associated pneumonia (VAP) exemplifies a condition where rapid, accurate pathogen identification is critical. In a recent study of 63 patients with suspected VAP, nanopore-based mNGS demonstrated remarkable diagnostic performance. When compared to a composite standard, it achieved a sensitivity of 97.4% and a specificity of 100% [107]. Crucially, the co-infection rate identified by mNGS increased from 27% (based on clinical findings) to 46%, revealing a much more complex microbial landscape than previously appreciated, including viral co-infections [107]. The most significant advantage was in turnaround time: the median time for mNGS results was 4.43 hours, compared to 72 hours for routine culture [107]. This rapid result enables clinicians to make informed, data-driven treatment decisions days earlier than with conventional methods.
Table 1: Performance Metrics of mNGS vs. Culture for Pathogen Detection in VAP
| Parameter | mNGS (vs. Gold Standard) | mNGS (vs. Composite Standard) | Routine Culture |
|---|---|---|---|
| Sensitivity | 91.3% | 97.4% | Varies by pathogen/culturability |
| Specificity | 78.3% | 100% | 100% (for detected pathogens) |
| Co-infection Detection | Identified 46% of cases (vs. 27% clinically) | Limited by pathogen selectivity and culturability | |
| Median Turnaround Time | 4.43 hours | ~72 hours |
For AMR prediction, novel inference methods that move beyond simple ARG detection show great promise. One study on Klebsiella pneumoniae demonstrated that inferring resistance by matching whole-genome data to a curated database achieved 85.7% accuracy for predicting carbapenem resistance within 1 hour, outperforming the 54.2% accuracy of traditional AMR gene detection at the 6-hour mark [108].
Experimental Protocols
Sample Collection and DNA Extraction from Endotracheal Aspirates (ETA)
Principle: This protocol is designed to maximize yield and quality of microbial nucleic acids from respiratory samples for subsequent library preparation and sequencing [107].
Materials:
- Sterile endotracheal aspirate collection kit
- Phosphate Buffer Saline (PBS)
- Lytic enzyme solution (e.g., from Qiagen Inc.)
- MetaPolyzyme (Sigma Aldrich)
- IndiSpin Pathogen Kit (Indical Bioscience) or equivalent
- Qubit 4.0 fluorometer with dsDNA HS Assay kit (Thermo Fisher Scientific)
Procedure:
- Collection: Aseptically collect 1-2 mL of endotracheal aspirate from the patient and place it in a sterile tube.
- Aliquoting: Split the sample into two aliquots. One is sent for standard microbiological culture and antimicrobial susceptibility testing (AST), and the other is stored at 4°C for mNGS processing (for up to 72 hours).
- Enrichment: Mix 300 µL of the ETA sample with PBS in a 1:3 ratio. Centrifuge at 20,000 × g for 5 minutes. Discard 1 mL of supernatant.
- Enzymatic Lysis: To the pellet, add 5 µL of lytic enzyme solution and 10 µL of reconstituted MetaPolyzyme. Gently mix and incubate for 1 hour at 37°C in a shaker.
- Nucleic Acid Extraction: Perform DNA extraction using the IndiSpin Pathogen Kit according to the manufacturer's instructions. Include a negative control (sterile deionized water) to monitor for contamination.
- Quantification: Assess DNA concentration using the Qubit fluorometer.
Nanopore Library Preparation and Sequencing
Principle: This protocol utilizes the Oxford Nanopore Technology (ONT) MinION platform for real-time, long-read sequencing, enabling rapid diagnosis [107].
Materials:
- PCR Barcoding Kit (SQK-PBK004, ONT)
- R9.4.1 flow cell (FLO-MIN106)
- MinION Mk1B device
- ONT MinKNOW GUI software (version 4.2.8 or higher)
Procedure:
- Library Preparation: Prepare the sequencing library using the PCR Barcoding Kit according to the manufacturer's instructions. Use a 4-minute DNA extension time and 15 PCR amplification cycles.
- Loading: Load 75 µL of the prepared library onto the flow cell.
- Sequencing: Initiate the sequencing run using the MinKNOW software. The run can be stopped once approximately 50,000 read counts per sample are accumulated, which is typically sufficient for robust microbial detection [107].
Bioinformatic Analysis for Pathogen and AMR Detection
Principle: A automated bioinformatics pipeline processes raw sequencing data to identify pathogens and their resistance profiles. The following workflow can be implemented using open-source tools or integrated platforms like the CZ ID [107] [3].
Workflow Diagram 1: Dual-path bioinformatics pipeline for integrated pathogen and AMR detection from mNGS data.
Procedure:
- Basecalling and Demultiplexing: Convert raw electrical signals from the sequencer into nucleotide sequences (FASTQ files) and assign them to individual samples using barcodes (e.g., with ONT's Guppy).
- Quality Control and Host Depletion: Remove low-quality reads and sequences originating from the host (human) genome using aligners like Bowtie2 or HISAT2 [3].
- Pathogen Identification:
- Alignment: Map non-host reads to comprehensive microbial genome databases.
- Taxonomic Classification: Assign reads to specific microbial species using tools like Kraken2 or Centrifuge. The Relative Abundance (RA) of a pathogen has been shown to be a highly diagnostic metric, with an optimal threshold of 9.93% for VAP diagnosis [107].
- AMR Gene Analysis:
- Gene Detection: Analyze quality-filtered reads or assembled contigs against the Comprehensive Antibiotic Resistance Database (CARD) using the Resistance Gene Identifier (RGI) tool [3].
- Pathogen-of-Origin Prediction: Leverage beta features in RGI that use unique k-mers to predict which pathogen species carries a detected AMR gene and whether it is located on a chromosome or plasmid [3].
- Data Integration and Reporting: Correlate identified pathogens with detected ARGs to generate a comprehensive clinical report.
Research Reagent Solutions
A successful mNGS workflow relies on a suite of specialized reagents and computational tools. The table below summarizes key solutions for pathogen detection and AMR analysis.
Table 2: Essential Research Reagents and Tools for mNGS-based Pathogen Detection
| Item Name | Function/Description | Example Use Case |
|---|---|---|
| IndiSpin Pathogen Kit | DNA extraction from complex clinical samples. | Efficiently lyses diverse microbes (bacteria, fungi) in endotracheal aspirates [107]. |
| ONT PCR Barcoding Kit (SQK-PBK004) | Prepares DNA libraries for nanopore sequencing with sample barcodes. | Enables multiplexed sequencing of multiple samples on a single MinION flow cell [107]. |
| Illumina Respiratory Pathogen ID/AMR Panel (RPIP) | Probe-based panel for targeted enrichment of pathogen sequences. | Focused screening for 383 respiratory pathogens and AMR genes from diverse sample matrices [109]. |
| Comprehensive Antibiotic Resistance Database (CARD) | Curated database of ARGs and associated metadata. | Reference database for identifying and interpreting detected resistance genes via RGI [3]. |
| CZ ID AMR Module | Open-access, cloud-based bioinformatics platform. | Integrates pathogen detection and AMR profiling from mNGS data without local compute infrastructure [3]. |
Advanced Analysis: Resistance Inference and Visualization
While detecting ARGs is valuable, predicting phenotypic resistance remains a challenge. A powerful alternative is the "Align-Search-Infer" pipeline, which infers resistance by matching query sequences to a curated database of whole bacterial genomes with known AST profiles [108]. This method can predict carbapenem resistance in K. pneumoniae with high accuracy within 10-60 minutes of sequencing initiation, requiring as little as 50-500 kilobases of sequence data [108].
Workflow Diagram 2: The "Align-Search-Infer" pipeline for rapid antimicrobial resistance prediction.
Effective data visualization is critical for interpreting complex mNGS and resistome data. For non-bioinformaticians, platforms like CZ ID provide interactive tables that allow sorting and filtering of AMR hits based on metrics such as gene coverage, percent identity, and read counts per million (rpM) [3]. More advanced visualizations, such as phylogenetic trees coupled with heatmaps of ARG presence/absence, can reveal transmission clusters of multidrug-resistant pathogens in hospital outbreaks [3]. These visual strategies transform raw sequencing data into actionable insights for clinicians and public health officials.
Conclusion
Metagenomic NGS has unequivocally transformed the landscape of antimicrobial resistance research by providing an unparalleled, broad-spectrum view of the resistome. While challenges in standardization, cost, and data interpretation remain, the technology's ability to detect resistance mechanisms directly from complex samples, without prior culturing, offers a definitive speed and comprehensiveness advantage over traditional methods. The integration of optimized host-depletion protocols and sophisticated bioinformatics is steadily enhancing its diagnostic accuracy. Future directions must focus on the development of globally harmonized reporting standards, the creation of more curated and comprehensive AMR databases, and the rigorous validation of mNGS through large-scale prospective clinical trials. As the technology matures and becomes more accessible, its integration into routine public health surveillance and clinical diagnostics will be paramount for guiding stewardship efforts, curbing the spread of resistant infections, and ultimately informing the development of next-generation antimicrobial therapies.
References
- 1. Metagenomic Next-Generation Sequencing in Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384723/]
- 2. The application value and challenges of metagenomic next ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1686503/full]
- 3. Simultaneous detection of pathogens and antimicrobial ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01480-2]
- 4. Exploring drug resistance genes in Acinetobacter ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1669208/full]
- 5. Antimicrobial resistance prediction by clinical metagenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11020437/]
- 6. Comparative Diagnostic Accuracy of Metagenomic Next ... [https://www.sciencedirect.com/science/article/pii/S0163445325002610]
- 7. Application of mNGS in the Etiological Analysis of Lower Respiratory... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849087/]
- 8. Metagenomics as a Transformative Tool for Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939754/]
- 9. Application of next-generation sequencing in the detection ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898125003997]
- 10. Metagenomic analysis of human, animal, and ... [https://www.nature.com/articles/s41598-025-90777-8]
- 11. Hypothesis-Free Biomarker Discovery in Oncology [https://blog.crownbio.com/hypothesis-free-biomarker-discovery-in-oncology]
- 12. A culture-, amplification-independent, and rapid method for ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1104701/full]
- 13. Antibiotic Discovery and Resistance: The Chase and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8868473/]
- 14. Next generation sequencing as a panacea for antibiotic ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1650925/full]
- 15. Antimicrobial Resistance Gene Detection Methods for Bacteria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8146338/]
- 16. Metagenomic insights into resistance trends related to ... [https://www.nature.com/articles/s41598-025-06125-3]
- 17. Indexed variation graphs for efficient and accurate resistome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6198860/]
- 18. Unraveling the role of mobile genetic elements in antibiotic ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1557413/full]
- 19. Mobile Genetic Elements Associated with Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6148190/]
- 20. cost-effective antibiotic resistome profiling of metagenomic ... [https://pubmed.ncbi.nlm.nih.gov/40019273/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1F9sM2NQANFmLi9huljY4jEJuDZBPy7jc4pX-dgaFI9ivVeQ9&fc=None&ff=20251124175458&v=2.18.0.post22+67771e2]
- 21. Resistome identification [https://bio-protocol.org/exchange/minidetail?id=3285240&type=30]
- 22. Duplicated antibiotic resistance genes reveal ongoing ... [https://www.nature.com/articles/s41467-024-45638-9]
- 23. Resistome profiling and bacterial community structure of ... [https://www.nature.com/articles/s41598-025-20043-4]
- 24. Metagenomic analysis deciphers airborne pathogens with ... [https://www.sciencedirect.com/science/article/pii/S0160412025003204]
- 25. Metagenomic co-assembly uncovers mobile antibiotic ... [https://www.nature.com/articles/s43247-025-02381-3]
- 26. Metagenomic Approaches to Analyze Antimicrobial ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.575592/full]
- 27. Quantitative PCR versus metagenomics for monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10117749/]
- 28. Temporal dynamics and persistence of resistance genes to ... [https://www.nature.com/articles/s41545-024-00349-y]
- 29. ResistoXplorer: a web-based tool for visual, statistical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7991225/]
- 30. AMRViz enables seamless genomics analysis and ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-024-05792-9]
- 31. Metagenomic Next-Generation Sequencing in Infectious Diseases: Clinical Applications, Translational Challenges, and Future Directions [https://www.mdpi.com/2075-4418/15/16/1991]
- 32. AmrProfiler: a comprehensive tool for identifying ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12230725/]
- 33. Bioinformatics approaches to the study of antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8683011/]
- 34. Beyond clinical genomics: addressing critical gaps in One ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1596720/full]
- 35. Beyond clinical genomics: addressing critical gaps in One ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066572/]
- 36. Comparative diagnostic performance of metagenomic and ... [https://www.nature.com/articles/s41598-025-11834-w]
- 37. Review Targeted next-generation sequencing (tNGS): an ... [https://www.sciencedirect.com/science/article/pii/S1876034125002850]
- 38. Targeted Versus Shotgun Metagenomic Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10169413/]
- 39. Shotgun-metagenomics based prediction of antibiotic ... [https://www.nature.com/articles/s41598-021-00383-7]
- 40. Overcoming challenges in metagenomic AMR surveillance ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1614301/full]
- 41. Antimicrobial Resistance | Detection with NGS [https://www.illumina.com/areas-of-interest/microbiology/public-health-surveillance/antimicrobial-resistance-detection.html]
- 42. Comparison of metagenomic next-generation sequencing ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.1042945/full]
- 43. Metagenomic next-generation sequencing of cell-free and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9551220/]
- 44. Comparative analysis of metagenomic next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934473/]
- 45. Comparison Analysis of Different DNA Extraction Methods on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9273838/]
- 46. Comparison of DNA extraction methods for 16S rRNA gene ... [https://www.nature.com/articles/s41598-023-33959-6]
- 47. Datasets for benchmarking antimicrobial resistance genes ... [https://www.nature.com/articles/s41597-022-01463-7]
- 48. Genomics for antimicrobial resistance—progress and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057382/]
- 49. An ISO-certified genomics workflow for identification and ... [https://www.nature.com/articles/s41467-022-35713-4]
- 50. Application of different DNA extraction procedures, library ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6838873/]
- 51. Development of an NGS-Based Workflow for Improved ... [https://www.mdpi.com/2079-6382/9/8/503]
- 52. Automation of customizable library preparation for next- ... [https://www.nature.com/articles/s41598-024-67950-6]
- 53. Sequencing-based methods and resources to study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6525649/]
- 54. SARS-CoV-2 variant biology: immune escape, ... [https://www.nature.com/articles/s41579-022-00841-7]
- 55. Tracking SARS-CoV-2 variants [https://www.who.int/activities/tracking-SARS-CoV-2-variants]
- 56. Could wastewater-based surveillance be key to combating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607910/]
- 57. The interplay between antimicrobial resistance genes and ... [https://annalsmicrobiology.biomedcentral.com/articles/10.1186/s13213-025-01814-w]
- 58. National-scale insights into AMR transmission along the ... [https://www.sciencedirect.com/science/article/pii/S0043135425005123]
- 59. Introducing AMR surveillance systems: View as single page [https://www.open.edu/openlearncreate/mod/oucontent/view.php?id=227184&printable=1]
- 60. Characterization of antibiotic resistance genes in soils from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12149118/]
- 61. Enhanced detection for antibiotic resistance genes in ... [https://www.sciencedirect.com/science/article/pii/S0043135424019560]
- 62. Targeted next-generation sequencing for antimicrobial ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1526087/full]
- 63. Simultaneous detection of pathogens and antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057172/]
- 64. Antibiotic resistance genes in surface water of eutrophic ... [https://pubmed.ncbi.nlm.nih.gov/28516210/]
- 65. Microbial communities, resistance genes, and resistome ... [https://www.sciencedirect.com/science/article/pii/S2772416623000049]
- 66. AMRFinderPlus - Pathogen Detection - NCBI - NIH [https://www.ncbi.nlm.nih.gov/pathogens/antimicrobial-resistance/AMRFinder/]
- 67. Comparative assessment of annotation tools reveals ... [https://www.nature.com/articles/s41598-025-24333-9]
- 68. A long-read sequencing approach to high-resolution ... [https://www.nature.com/articles/s41598-025-96558-7]
- 69. Benefits and challenges of host depletion methods in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12234985/]
- 70. Microbial DNA extraction of high-host content and low ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1038120/full]
- 71. Accurate quantification of bacterial abundance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7660251/]
- 72. Comparison of four DNA extraction kits efficiency for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10051199/]
- 73. Optimization of Metagenomic Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436562/]
- 74. Combined nanopore adaptive sequencing and enzyme-based ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-021-08023-0]
- 75. Development of a portable on-site applicable metagenomic ... [https://www.nature.com/articles/s41598-023-46771-z]
- 76. A Ten-Month Study Leveraging RNA-Probe Capture and ... [https://www.sciencedirect.com/science/article/pii/S0304389425034867]
- 77. vs Dry Lab: What Recruiters Searching in Wet Lab 2025 [https://www.linkedin.com/pulse/wet-lab-vs-dry-careers-biotech-what-recruiters-2025-sujay-mukherjee-0sv0c]
- 78. vs Dry Lab: Challenges, Benefits and Skills... - BioSpace Wet Lab [https://www.biospace.com/wet-lab-vs-dry-lab-which-is-best-for-you]
- 79. Performance Characteristics of Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9238399/]
- 80. The impact of sequencing depth on the inferred taxonomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8204541/]
- 81. Identification of antibiotic resistance genes from whole ... [https://onehealthadv.biomedcentral.com/articles/10.1186/s44280-025-00079-x]
- 82. Introduction to Next Generation Sequencing (NGS) Data and ... [https://bioinformatics.ccr.cancer.gov/docs/bioinformatics-for-beginners-2025/Module2_RNA_Sequencing/Lesson7/]
- 83. Minimal gene signatures enable high-accuracy prediction ... [https://www.nature.com/articles/s41540-025-00584-0]
- 84. The diagnostic value of RNA-mNGS and DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12454375/]
- 85. ARG-ANNOT, a New Bioinformatic Tool To Discover ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3910750/]
- 86. Toward Accurate and Quantitative Comparative Metagenomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC5080976/]
- 87. Challenges in the application of NGS in the clinical laboratory [https://www.sciencedirect.com/science/article/abs/pii/S0198885921000835]
- 88. Comparison of the effectiveness of different normalization ... [https://www.nature.com/articles/s41598-024-57670-2]
- 89. Evaluation of normalization methods for predicting ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1369628/full]
- 90. Bioinformatics for wet-lab scientists: practical application in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10326960/]
- 91. Comparison of metagenomic next-generation sequencing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10964532/]
- 92. Metagenomic identification of pathogens and antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10773726/]
- 93. Machine learning-selected minimal features drive high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12323339/]
- 94. The Comparison of Metagenomic Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9586124/]
- 95. The value of metagenomic next-generation sequencing in ... [https://www.nature.com/articles/s41598-025-86295-2]
- 96. Comparison of mNGS and conventional culture in non- ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2023.1146088/full]
- 97. Tackling antimicrobial resistance, one genome at a time [https://www.illumina.com/company/news-center/feature-articles/tackling-antimicrobial-resistance--one-genome-at-a-time.html]
- 98. Novel Clinical mNGS-Based Machine Learning Model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10204632/]
- 99. Metagenomic prediction of antimicrobial resistance in critically ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-022-01072-4]
- 100. Comparing antimicrobial resistant genes and phenotypes ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-023-02975-x]
- 101. Comparison of microbial culture, metagenomic next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343261/]
- 102. Extending the culture duration could not improve ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1551862/full]
- 103. Comparison of microbial culture, metagenomic next- ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1606283/full]
- 104. Comparison of metagenomic next-generation sequencing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10847245/]
- 105. cfDNA or Genomic DNA-Based mNGS Assays [https://micronbrane.com/cell-free-or-genomic-dna-based-mngs-assays/]
- 106. Comparison of pathogen detection performance between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375685/]
- 107. Detection of Pathogens and Antimicrobial Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9939671/]
- 108. Inference of antimicrobial resistance (AMR) from a whole ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275941/]
- 109. Probe-based metagenomic pathogen detection [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1656831/full]