CRISPR-Cas9 Delivery Methods: A Comprehensive Guide for Therapeutic Development
This article provides a detailed overview of the current landscape of CRISPR-Cas9 delivery systems, tailored for researchers, scientists, and drug development professionals.
CRISPR-Cas9 Delivery Methods: A Comprehensive Guide for Therapeutic Development
Abstract
This article provides a detailed overview of the current landscape of CRISPR-Cas9 delivery systems, tailored for researchers, scientists, and drug development professionals. It covers foundational principles of CRISPR cargo and cellular uptake, explores viral and non-viral delivery methodologies with clinical applications, addresses key challenges in efficiency and safety with troubleshooting strategies, and presents comparative data from recent studies to validate method selection. The scope extends from basic mechanisms to advanced innovations and clinical trial updates, offering a practical framework for optimizing delivery strategies in both research and therapeutic contexts.
The Building Blocks: Understanding CRISPR-Cas9 Cargo and Cellular Entry
The CRISPR-Cas9 system requires the delivery of two key components into the nucleus of a target cell: the Cas nuclease and a guide RNA (gRNA). The format in which these components are delivered—collectively referred to as the "cargo"—significantly influences the efficiency, specificity, and safety of genome editing. The three primary cargo options are DNA, mRNA, and the pre-assembled Ribonucleoprotein (RNP) complex [1] [2]. The choice of cargo is inextricably linked to the selection of a delivery method and directly impacts critical experimental outcomes, including editing efficiency, off-target effects, and cellular toxicity. This application note provides a comparative analysis of these three cargo formats and details standardized protocols for their use in CRISPR research.
Comparative Analysis of Cargo Formats
The table below summarizes the key characteristics, advantages, and limitations of DNA, mRNA, and RNP cargo formats.
Table 1: Comparative Analysis of CRISPR-Cas9 Cargo Formats
| Characteristic | DNA (Plasmid) | mRNA | Ribonucleoprotein (RNP) |
|---|---|---|---|
| Cargo Composition | Plasmid encoding Cas9 and gRNA [2] | mRNA for Cas9 translation + separate gRNA [1] | Pre-complexed Cas9 protein + gRNA [1] |
| Mechanism of Action | Requires nuclear entry, transcription, and translation [3] | Requires cytoplasmic translation and nuclear entry [1] | Direct nuclear activity; no transcription/translation needed [4] |
| Onset of Editing Activity | Slow (24-72 hours) [3] | Moderate (12-48 hours) | Very Fast (hours) [4] [3] |
| Editing Efficiency | Variable, can be lower [3] | Moderate to High | Consistently High [4] [3] |
| Off-Target Effects | Higher (prolonged expression) [3] | Moderate | Lower (transient activity) [4] [3] |
| Cytotoxicity | Higher (transfection stress, immune activation) [3] | Moderate (immune activation possible) | Lower [3] |
| Risk of Genomic Integration | Yes (random plasmid integration) [3] | No | No [3] |
| Ease of Use | Simple cloning and production | Requires in vitro transcription | Requires protein purification; simple complexing |
| Ideal Application | Stable cell line generation, long-term expression studies | In vivo delivery via LNPs [5] | Knockouts in primary and sensitive cells, clinical applications [4] |
Detailed Cargo Delivery Protocols
Protocol: Plasmid DNA Transfection via Lipofection
This protocol is suitable for delivering all-in-one CRISPR plasmids to immortalized cell lines (e.g., HEK293T) using lipid-based transfection reagents.
Research Reagent Solutions:
- All-in-one CRISPR Plasmid: A single plasmid vector expressing both Cas9 and the target-specific gRNA [2].
- Lipofection Reagent: A cationic lipid formulation that complexes with DNA to facilitate cellular uptake.
- Opti-MEM Reduced-Serum Medium: Used to dilute the DNA and lipofection reagent.
- Appropriate Cell Culture Media: For maintaining the target cells.
Procedure:
- Day 1: Cell Seeding. Seed an appropriate number of cells into a multi-well plate to achieve 70-90% confluency at the time of transfection (24 hours later).
- Day 2: Transfection Complex Formation.
- Dilute 1-2 µg of the all-in-one CRISPR plasmid in 50-100 µL of Opti-MEM.
- Mix the lipofection reagent gently and dilute the recommended amount (e.g., 2-5 µL) in an equal volume of Opti-MEM (50-100 µL). Incubate for 5 minutes at room temperature.
- Combine the diluted DNA and diluted lipofection reagent. Mix gently and incubate for 15-20 minutes at room temperature to allow DNA-lipid complexes to form.
- Transfection. Add the complex mixture dropwise to the cells in complete media. Gently swirl the plate to ensure even distribution.
- Day 3: Post-transfection. 4-6 hours after transfection, replace the media with fresh complete media to reduce cytotoxicity.
- Analysis. Analyze editing efficiency 48-72 hours post-transfection via genomic DNA extraction, PCR amplification of the target locus, and sequencing (e.g., T7 Endonuclease I assay or NGS).
Protocol: mRNA and RNP Delivery via Electroporation
Electroporation is highly effective for delivering mRNA and RNP cargoes, especially in hard-to-transfect cells like primary T cells and stem cells [4] [6].
Research Reagent Solutions:
- Cas9 mRNA + synthetic gRNA OR Pre-complexed Cas9 RNP: For RNP, complex purified Cas9 protein with synthetic gRNA at a molar ratio of 1:1.2 to 1:1.5 and incubate at room temperature for 10-20 minutes before electroporation [4].
- Electroporation Buffer: A cell-type-specific, low-conductivity buffer.
- Electroporation Cuvettes/Plates: Compatible with the electroporator.
- Pre-warmed Complete Media.
Procedure:
- Cell Preparation. Harvest and wash the target cells (e.g., primary human T cells). Resuspend the cell pellet in the electroporation buffer at a concentration of 1-10 x 10^6 cells/mL.
- Cargo Loading. For a 100 µL reaction, mix 10-20 µg of Cas9 mRNA with 5-10 µg of synthetic gRNA, or the pre-complexed RNP (e.g., 5-20 µM final concentration), with the cell suspension.
- Electroporation.
- Transfer the cell-cargo mixture to an electroporation cuvette.
- Electroporate using a cell-type-optimized waveform (e.g., Square Wave) and parameters. A typical starting condition for T cells is 500V, 2ms, 1 pulse.
- Immediately after the pulse, add pre-warmed media to the cuvette and transfer the cells to a culture plate.
- Recovery and Analysis. Culture the cells and assess viability and editing efficiency after 3-5 days. Editing from RNP can be detected as early as 24 hours post-electroporation.
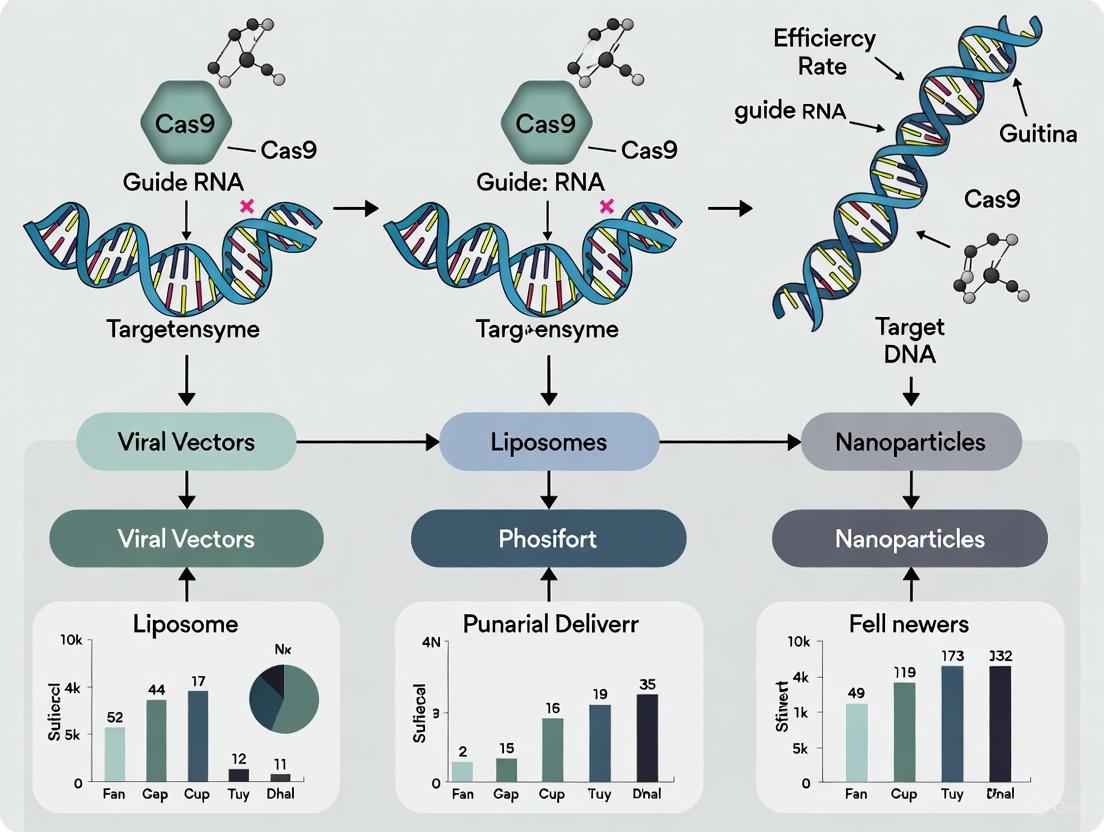
The workflow and key cellular mechanisms for each cargo format are illustrated below.
Advanced RNP Delivery Strategy
A cutting-edge strategy for RNP delivery involves the use of engineered Extracellular Vesicles (EVs). A 2025 study detailed a modular system for efficient EV-mediated RNP delivery [7].
Mechanism: EV-producing cells (e.g., HEK293T) are engineered to express a fusion protein. This protein consists of:
- MS2 Coat Protein (MCP): An RNA-binding module.
- PhoCl Linker: A UV-light-cleavable protein domain.
- CD63 Transmembrane Domain: A protein that directs the fusion to localize in EVs. Simultaneously, MS2 RNA aptamers are incorporated into the tetraloop and stemloop 2 of the sgRNA. During EV biogenesis, the MCP-fusion protein inside the EV binds with high affinity to the MS2-tagged sgRNA, which is already complexed with Cas9 protein, thereby loading the RNP into the EV [7]. Upon isolation and administration to target cells, exposure to UV light cleaves the PhoCl linker, releasing the RNP complex for efficient genome editing.
Table 2: Key Reagents for EV-Mediated RNP Delivery
| Reagent | Function |
|---|---|
| MCP-PhoCl-CD63 Plasmid | Expression vector for the EV-loading fusion protein [7] |
| MS2-Modified sgRNA | sgRNA engineered with MS2 aptamers for high-affinity loading [7] |
| Purified Cas9 Protein | Wild-type or variant Cas9 nuclease |
| Tangential Flow Filtration (TFF) | System for efficient EV isolation and concentration [7] |
Concluding Remarks
The selection of CRISPR cargo is a critical determinant of experimental and therapeutic success. DNA plasmids are simple but associated with higher off-target effects and toxicity. mRNA offers a transient profile suitable for in vivo delivery, while RNP complexes provide the highest specificity and efficiency for a wide range of in vitro and ex vivo applications, particularly in clinically relevant primary cells. The ongoing development of advanced delivery platforms, such as engineered extracellular vesicles and optimized lipid nanoparticles, continues to enhance the utility and reach of each cargo format, paving the way for more precise and effective genome editing.
The therapeutic application of the CRISPR-Cas9 system is fundamentally constrained by the challenge of delivering its molecular components into the nucleus of target cells. The efficiency, specificity, and safety of genome editing are directly governed by the cellular uptake mechanisms employed by the delivery vehicle [8] [9]. These vehicles must navigate multiple biological barriers, including the cell membrane, endosomal entrapment, and for non-viral methods, the nuclear envelope, to successfully deliver their cargo [1] [10]. Understanding the distinct entry pathways and intracellular trafficking of these vectors is therefore critical for optimizing CRISPR-based therapies. This application note details the cellular uptake mechanisms of the primary vehicle classes—viral vectors, lipid nanoparticles, and extracellular vesicles—within the context of CRISPR-Cas9 delivery, providing researchers with a mechanistic framework for selection and protocol design.
Vehicle-Specific Uptake Mechanisms and Intracellular Trafficking
The journey of a CRISPR delivery vehicle from the extracellular space to the nucleus involves a series of highly coordinated steps. The initial entry mechanism dictates the subsequent intracellular pathway and ultimately, the editing outcome.
Table 1: Quantitative Comparison of Cellular Uptake and Editing Efficiencies
| Delivery Vehicle | Primary Uptake Mechanism | Editing Efficiency (Reported Ranges) | Key Intracellular Processing Steps |
|---|---|---|---|
| Adeno-Associated Virus (AAV) | Clathrin-mediated endocytosis [1] | Varies by serotype and target cell; used in multiple clinical trials (e.g., EDIT-101) [11] | Endosomal escape, endosomal acidification triggers conformational change, nuclear import of single-stranded vector genome [1] [11] |
| Lentivirus (LV) | Receptor-mediated endocytosis (e.g., via VSV-G pseudotyping) [12] | High in immune cells; 30-70% transduction efficiency in clinical CAR-T manufacturing [12] | Reverse transcription in the cytoplasm, import of pre-integration complex into the nucleus, integration into host genome [1] [12] |
| Lipid Nanoparticle (LNP) | Endocytosis (multiple pathways, including clathrin-mediated) [1] [13] | Efficient in liver; >90% protein reduction in hATTR trial [5] | Endosomal encapsulation, endosomal escape via ionization of lipids, cargo release into the cytoplasm [1] [8] |
| Extracellular Vesicle (EV) | Membrane fusion or endocytosis [7] [9] | Demonstrated efficient endogenous gene editing (e.g., CCR5) [7] | Cargo release into the cytoplasm via fusion or endosomal escape; avoids lysosomal degradation [7] [10] |
The following diagram illustrates the fundamental pathways these vehicles take to enter cells and deliver their CRISPR cargo.
Viral Vector Uptake and Processing
Viral vectors are engineered to exploit naturally evolved mechanisms for efficient cellular entry.
Adeno-Associated Viruses (AAVs) first bind to primary receptors (e.g., HGFR for AAV2) and co-receptors (e.g., αVβ5 integrin) on the cell surface. This binding triggers clathrin-mediated endocytosis. Inside the resulting endosome, the acidic environment triggers conformational changes in the viral capsid, leading to endosomal escape. The viral single-stranded DNA genome is then imported into the nucleus [1] [11]. A key advantage is their episomal persistence, which avoids insertional mutagenesis but can also lead to transient expression depending on the cell type [1].
Lentiviral Vectors (LVs), often pseudotyped with the Vesicular Stomatitis Virus G-glycoprotein (VSV-G), enter primarily through receptor-mediated endocytosis. The VSV-G protein binds ubiquitously to LDL receptors on the target cell. Following endocytosis, the viral envelope fuses with the endosomal membrane in an acidification-dependent process, releasing the viral core into the cytoplasm. Here, the viral RNA is reverse-transcribed into DNA, forming a pre-integration complex that is actively transported into the nucleus via the nuclear pore complex. A defining feature of LVs is their ability to integrate the transgene into the host genome, enabling long-term expression—a critical feature for durable CAR-T cell therapies [1] [12].
Non-Viral Vector Uptake and Processing
Non-viral vectors offer advantages in safety and manufacturability, with uptake mechanisms that are primarily endocytic.
Lipid Nanoparticles (LNPs) interact with the cell membrane through electrostatic and apolar interactions, leading to engulfment via endocytosis. A critical step for LNP success is endosomal escape. Modern LNPs contain ionizable cationic lipids that are neutral at physiological pH but become positively charged in the acidic endosome. These protonated lipids can disrupt the endosomal membrane, facilitating the release of the CRISPR payload (e.g., RNP, mRNA) into the cytoplasm before the endosome matures into a degradative lysosome [1] [13]. The intrinsic liver tropism of systemically administered LNPs has been effectively leveraged in clinical trials for liver-specific diseases like hATTR and HAE [5].
Extracellular Vesicles (EVs) are natural lipid nanoparticles that can enter cells through multiple routes. They can engage in direct membrane fusion, releasing their cargo directly into the cytosol, thereby bypassing endosomal entrapment entirely. Alternatively, they can enter via endocytosis [7] [9]. Their native composition provides innate biocompatibility and reduces immunogenicity. Recent engineering strategies, such as fusing RNA-binding domains (e.g., MS2 coat protein) to EV-enriched tetraspanins (e.g., CD63), have significantly improved the loading efficiency of Cas9 RNP complexes, enabling robust gene editing [7].
Detailed Experimental Protocol: Analyzing LNP Uptake and Intracellular Trafficking
This protocol outlines the steps to track the cellular uptake and endosomal escape of LNPs delivering CRISPR RNP in vitro, using HeLa cells as a model system. The methodology is adapted from recent research on RNP-MITO-Porter systems [13].
Research Reagent Solutions
Table 2: Essential Reagents for LNP Uptake and Trafficking Experiments
| Reagent/Material | Function/Description | Example/Note |
|---|---|---|
| Cas9 RNP Complex | Active CRISPR editing machinery. | Pre-complexe Cas9 protein with fluorescently labeled sgRNA (e.g., Cy5). |
| Ionizable Lipid LNPs | Delivery vehicle. | Formulated with ionizable lipid (e.g., DOPE), phospholipid, cholesterol, and PEG-lipid [13]. |
| HeLa Cell Line | Model adherent cell line. | Easy to culture and transfert; used extensively in uptake studies [13]. |
| LysoTracker Deep Red | Fluorescent dye labeling acidic organelles (lysosomes). | Used to assess co-localization and endosomal escape. |
| DMEM Growth Medium | Cell culture maintenance. | Supplemented with 10% FBS and 1% penicillin-streptomycin. |
| Confocal Microscopy | High-resolution imaging of intracellular trafficking. | Equipped with lasers for DAPI, FITC, Cy5, and far-red channels. |
| Flow Cytometer | Quantitative analysis of cellular uptake. | Measures fluorescence intensity in thousands of cells. |
| 4% Paraformaldehyde (PFA) | Cell fixation. | Preserves cellular structures for imaging. |
Step-by-Step Procedure
LNP Formulation and Characterization:
- Formulate LNPs encapsulating Cy5-labeled RNP using a microfluidic device. The aqueous phase contains the RNP in HEPES buffer, while the organic phase contains the lipid mix in ethanol. Rapid mixing in the device promotes self-assembly into particles [13].
- Characterize the resulting LNP suspension using dynamic light scattering (DLS) to ensure a homogeneous particle size (e.g., ~70 nm) and a positive zeta potential, which aids in cellular interaction [13].
Cell Seeding and Preparation:
- Seed HeLa cells in glass-bottom imaging dishes at a density of 1.5 x 10^5 cells per dish in complete DMEM growth medium.
- Incubate the cells at 37°C and 5% CO₂ for 24 hours to achieve 60-70% confluency at the time of treatment.
LNP Treatment and Live-Cell Staining:
- Replace the culture medium with a fresh, pre-warmed medium.
- Add the formulated RNP-LNPs to the cells at a predetermined optimal concentration.
- Incubate for 4 hours at 37°C to allow for uptake and trafficking.
- One hour before the end of the incubation, add LysoTracker Deep Red to the culture medium at a recommended working concentration to stain acidic compartments.
Sample Fixation and Preparation:
- After incubation, carefully aspirate the medium and wash the cells three times with PBS to remove any non-internalized LNPs.
- Fix the cells by adding 4% PFA for 15 minutes at room temperature.
- Wash again with PBS and add an anti-fade mounting medium containing DAPI to stain the nuclei.
Image Acquisition and Analysis via Confocal Microscopy:
- Image the cells using a confocal laser scanning microscope.
- Use the following channels: DAPI (nucleus, blue), FITC/GFP (optional other marker, green), Cy5 (RNP-LNPs, red), and far-red (LysoTracker, magenta).
- Acquire Z-stack images to capture the 3D distribution of the signal within the cells.
- To analyze endosomal escape, quantify the degree of co-localization between the Cy5 signal (RNP) and the LysoTracker signal (acidic endosomes/lysosomes) using image analysis software (e.g., ImageJ with JaCoP plugin). A decrease in the Pearson's correlation coefficient over time indicates successful endosomal escape of the RNP cargo.
Quantitative Uptake Measurement via Flow Cytometry:
- In parallel, seed and treat HeLa cells in a standard 6-well plate under identical conditions.
- After the 4-hour incubation and PBS washes, trypsinize the cells, collect them in centrifuge tubes, and resuspend in flow cytometry buffer.
- Analyze the cells using a flow cytometer, detecting the Cy5 fluorescence. The geometric mean fluorescence intensity (MFI) of the treated cells, compared to untreated controls, provides a quantitative measure of LNP uptake.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagent Solutions for Studying Cellular Uptake
| Reagent Category | Specific Examples | Primary Function in Uptake Studies |
|---|---|---|
| Chemical Inhibitors | Chlorpromazine (clathrin-mediated endocytosis), Dynasore (dynamin), Filipin (caveolae-mediated endocytosis), Amiloride (macropinocytosis) [1] [10] | To delineate the primary endocytic pathway by selectively inhibiting specific mechanisms. |
| Fluorescent Labels | Cy5, FITC, Rhodamine (for labeling sgRNA, proteins, or lipids); Lipophilic dyes (e.g., DiI, DiO) [7] [13] | To visually track the vehicle and/or cargo throughout the uptake and intracellular trafficking process via microscopy and flow cytometry. |
| Endo/Lysosomal Markers | LysoTracker (acidic compartments), antibodies against LAMP1 or Rab proteins (early/late endosomes) [13] | To identify and track the progression of vesicles through the endosomal-lysosomal system and assess escape. |
| Engineered Cell Lines | Cells stably expressing fluorescently tagged organelle markers (e.g., GFP-Rab5 for early endosomes) | To enable live-cell imaging of cargo trafficking in real-time within defined intracellular compartments. |
Efficient intracellular delivery of the CRISPR-Cas9 system represents one of the most significant challenges in therapeutic genome editing. The success of any CRISPR-based experiment or therapy fundamentally depends on overcoming three interconnected delivery hurdles: the physical size limitations of the cargo, its stability within the cellular environment, and the ultimate requirement for nuclear access to enact genetic changes. This application note examines these critical parameters, providing a structured analysis and practical protocols to guide researchers in selecting and optimizing CRISPR delivery strategies for cell-based research and drug development.
Quantitative Analysis of CRISPR Delivery Cargo
The form in which CRISPR components are delivered significantly impacts editing efficiency, specificity, and potential cytotoxicity. The primary cargo configurations each present distinct advantages and challenges related to size, stability, and functionality.
Table 1: Comparative Analysis of CRISPR-Cas9 Cargo Configurations
| Cargo Form | Typical Size | Stability Considerations | Key Advantages | Key Limitations |
|---|---|---|---|---|
| DNA Plasmid | ~9-12 kb (for SpCas9) | Variable expression; prolonged activity increases off-target risk [1] | Simplicity of cloning and production; long-term expression | Cytotoxicity; variable editing efficiency; immunogenicity [1] |
| mRNA + gRNA | ~4.5 kb (SpCas9 mRNA) | mRNA susceptible to degradation; requires chemical modifications for stability [1] [14] | Transient expression; reduced off-target effects compared to plasmids | Requires nuclear export for translation; immunogenic potential |
| Ribonucleoprotein (RNP) | ~160 kDa (SpCas9 protein) | Immediate activity; rapid degradation minimizes off-target effects [1] [7] | Highest precision; minimal off-target effects; immediate activity [1] | More complex delivery due to large size and charge; limited time window for editing |
The cargo size directly influences the selection of an appropriate delivery vehicle, particularly when considering viral vectors with fixed payload capacities.
Table 2: Cargo Size Compatibility with Viral Delivery Vectors
| Viral Vector | Payload Capacity | Compatibility with CRISPR Cargo | Strategies for Large Cargos |
|---|---|---|---|
| Adeno-Associated Virus (AAV) | ~4.7 kb [1] | Too small for full SpCas9 (∼4.2 kb); requires dual-AAV systems or smaller Cas variants [1] | Use of smaller Cas enzymes (e.g., Cas12a, SaCas9); split-intein systems; separate delivery of Cas and gRNA [1] |
| Adenoviral Vectors (AdVs) | Up to 36 kb [1] | Readily accommodates Cas9, gRNA, and donor DNA templates | Minimal size constraints; suitable for large multi-component systems |
| Lentiviral Vectors (LVs) | ~8 kb | Can package most single CRISPR components | Suitable for Cas9 ORF delivery; used extensively for ex vivo editing (e.g., CAR-T cells) |
Cargo Stability and Nuclear Access Requirements
Beyond size considerations, cargo stability and nuclear translocation are critical determinants of editing success. The journey from extracellular delivery to functional nuclear activity presents multiple biological barriers.
Biological Barrier Navigation for CRISPR Cargo
The diagram above illustrates the sequential challenges CRISPR cargo must overcome from delivery to functional nuclear activity. Each barrier demands specific consideration during experimental design:
Endosomal Escape: Lipid-based nanoparticles (LNPs) and cell-penetrating peptides (CPPs) must facilitate escape before cargo degradation in lysosomal pathways [1]. The endosomal entrapment remains a primary cause of failed delivery for non-viral methods.
Cytoplasmic Stability: mRNA is particularly vulnerable to cytoplasmic nucleases, while RNP complexes benefit from immediate functionality without additional processing steps. Chemical modifications to mRNA (e.g., pseudouridine) can enhance stability and reduce immunogenicity [14].
Nuclear Membrane Translocation: The nuclear pore complex restricts passive diffusion of molecules larger than ~40 kDa. DNA plasmids require nuclear envelope breakdown during cell division for efficient access, while RNPs and mRNA-derived Cas9 depend on nuclear localization signals (NLS) for active transport [1]. This makes RNP delivery particularly challenging in non-dividing cells.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CRISPR-Cas9 Delivery Experiments
| Reagent / Material | Function | Example Applications |
|---|---|---|
| CRISPOR Web Tool | Guide RNA design and off-target prediction [15] | Selecting optimal gRNAs with high on-target and low off-target activity |
| MS2-MCP Loading System | Modular RNP loading into extracellular vesicles [7] | EV-mediated delivery using RNA-binding domains and aptamers |
| Lipid Nanoparticles (LNPs) | Encapsulation and delivery of nucleic acids or proteins [1] | in vivo delivery of CRISPR components; clinically validated platform |
| UV-Cleavable Linker (PhoCl) | Controlled cargo release post-delivery [7] | Light-activated release of CRISPR machinery from delivery vehicles |
| eGFP-to-BFP Reporter System | Rapid assessment of editing outcomes [16] | Quantifying HDR vs. NHEJ repair outcomes via fluorescence conversion |
| Selective Organ Targeting (SORT) LNPs | Tissue-specific nanoparticle delivery [1] | Targeted delivery to lung, spleen, and liver tissues |
Detailed Protocol: EV-Mediated RNP Delivery Using MS2-MCP System
This protocol details a modular strategy for extracellular vesicle-mediated CRISPR-Cas9 RNP delivery, leveraging MS2 coat protein (MCP) fusion constructs and MS2 aptamer-modified sgRNAs for efficient loading and targeted release [7].
Materials and Reagents
- Plasmid constructs: MCP-CD63 fusion, Cas9 expression vector, MS2-sgRNA expression vector
- HEK293T cells (or other appropriate packaging cell line)
- Cell culture media and transfection reagent (e.g., PEI, lipofectamine)
- Tangential Flow Filtration (TFF) system
- Size Exclusion Chromatography (SEC) columns
- OptiPrep density gradient medium
- Anti-CD63, anti-CD9 antibodies for immunocapture
- UV light source (365 nm) for PhoCl cleavage
Procedure
Day 1: Cell Seeding and Transfection
- Seed HEK293T cells in appropriate culture vessels at 60-70% confluence.
- Prepare transfection mixture containing three plasmid constructs:
- MCP-CD63 fusion construct (for EV loading)
- Cas9 or variant (e.g., ABE8e, dCas9-VPR) expression vector
- MS2-sgRNA expression vector with aptamers incorporated in tetraloop and stemloop 2
- Transfect cells using preferred transfection method and incubate for 48 hours.
Day 3: EV Isolation and Purification
- Collect cell culture supernatant and remove cells and debris by centrifugation at 2,000 × g for 30 minutes.
- Concentrate the supernatant using Tangential Flow Filtration (TFF) with a 100-500 kDa molecular weight cutoff membrane.
- Further purify EVs by Size Exclusion Chromatography (SEC) using commercially available columns (e.g., qEVoriginal).
- Characterize EV preparation by:
- Nanoparticle Tracking Analysis (NTA) for size distribution and concentration
- Transmission Electron Microscopy (TEM) for morphological assessment
- Western blot for EV markers (CD63, ALIX, TSG101) and absence of contaminants (Calnexin)
Day 3: EV Loading Validation
- Verify Cas9 RNP loading by Western blot comparing EVs with and without MCP-CD63 expression.
- Quantify sgRNA loading efficiency using digital droplet PCR (ddPCR) or qPCR.
- Confirm EV association through OptiPrep density gradient centrifugation - Cas9 should co-localize with EV markers in specific density fractions (1.10-1.18 g/mL).
Day 4: Target Cell Transduction and UV Activation
- Incubate isolated EVs with target cells for 24 hours.
- Expose cells to UV light (365 nm, optimized duration) to cleave the PhoCl linker and release Cas9 RNP cargo.
- Allow cells to recover for 24-72 hours before assessing editing efficiency.
Expected Outcomes and Troubleshooting
- Successful EV loading should yield ≥50-fold enrichment of Cas9 and sgRNA in EVs from MCP-CD63 expressing cells versus controls [7].
- Low loading efficiency may indicate issues with MCP-MS2 interaction - verify aptamer incorporation in sgRNA and MCP fusion protein expression.
- Poor editing in target cells may require optimization of EV:cell ratio or UV exposure conditions for efficient cargo release.
The interdependent considerations of cargo size, stability, and nuclear access requirements form the foundation of successful CRISPR-Cas9 experimental design. By matching cargo configuration to appropriate delivery vehicles and acknowledging the biological barriers to nuclear delivery, researchers can significantly enhance editing efficiency while minimizing off-target effects. The protocols and analytical frameworks provided here offer a structured approach to navigating these complex decisions, ultimately supporting the development of more reliable and reproducible CRISPR-based research and therapeutic applications.
The transformative potential of CRISPR-Cas9 gene editing in therapeutic applications is fundamentally constrained by a single, multifaceted challenge: the safe, efficient, and specific delivery of its molecular components into target cells. This dilemma, often termed "the delivery problem," represents the critical bottleneck in translating laboratory success into clinical breakthroughs [8] [9]. The core of this challenge lies in balancing three interdependent properties—Efficiency, the successful delivery and editing activity in a high percentage of target cells; Specificity, the minimization of off-target effects at unintended genomic sites; and Safety, the avoidance of immunogenic responses and long-term toxicities [17] [1]. These three properties form a "Delivery Triad" where optimizing one often compromises another. For instance, viral vectors can provide high efficiency but may raise safety concerns due to immunogenicity and long-term persistence, while physical methods are transient but can suffer from low efficiency and poor specificity [1]. This document provides a structured analysis of CRISPR-Cas9 delivery strategies through the lens of this triad, offering application notes and detailed protocols to guide researchers in making informed decisions for their experimental and therapeutic designs.
Cargo Types: The Foundation of the Editing Experiment
The form in which CRISPR-Cas9 components are delivered—the cargo—profoundly influences the outcome of a gene-editing experiment by directly affecting the triad's balance. The three primary cargo types offer distinct trade-offs between editing duration, off-target risk, and complexity of delivery [8] [18] [1].
Table 1: Comparison of CRISPR-Cas9 Cargo Types
| Cargo Type | Components Delivered | Key Advantages | Key Disadvantages | Impact on Triad |
|---|---|---|---|---|
| Plasmid DNA (pDNA) | DNA plasmid encoding Cas9 and gRNA [8] [1]. | Simple design, low-cost production, sustained expression [8] [18]. | Risk of genomic integration, prolonged Cas9 expression increasing off-target effects, cytotoxicity, large size [8] [18] [1]. | Safety: MediumSpecificity: LowEfficiency: Medium |
| Messenger RNA (mRNA) | mRNA for Cas9 + separate gRNA [8] [1]. | Rapid editing, transient activity, reduced off-target effects, no risk of genomic integration [8] [18]. | Instability, strong immune response, requires nuclear entry for activity, lower efficiency in some systems [8] [18]. | Safety: LowSpecificity: HighEfficiency: Medium |
| Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and gRNA [8] [1]. | Highest specificity, immediate activity, shortest persistence, minimal off-target effects [8] [18]. | Difficult and expensive to manufacture, challenging in vivo delivery, lack of efficient delivery vectors in vivo [8] [18]. | Safety: HighSpecificity: HighEfficiency: Low |
The following diagram illustrates the logical decision-making pathway for selecting the most appropriate cargo type based on the experimental goals and constraints related to the Delivery Triad.
Delivery Vehicles: Navigating Biological Barriers
The vehicle is as critical as the cargo, determining how CRISPR components traverse biological barriers to reach the nucleus. Vehicles are broadly classified into viral, non-viral, and physical methods, each with distinct implications for the Delivery Triad [8] [1].
Table 2: Comparison of Major CRISPR-Cas9 Delivery Vehicles
| Delivery Vehicle | Mechanism of Action | Key Advantages | Key Disadvantages | Ideal Cargo | Impact on Triad |
|---|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | Non-pathogenic virus; delivers genetic cargo without genome integration [18] [1]. | Low immunogenicity, high transduction efficiency, proven clinical success [18] [1]. | Limited packaging capacity (~4.7 kb), potential for long-term expression, pre-existing immunity in populations [18] [1]. | DNA, gRNA alone [1] | Safety: MediumSpecificity: MediumEfficiency: High |
| Lentivirus (LV) | Retrovirus that integrates into the host genome [18] [1]. | Large cargo capacity, infects dividing and non-dividing cells, stable long-term expression [1]. | Integration raises oncogenic risk, more severe off-target potential, complex safety profile [18] [1]. | DNA [1] | Safety: LowSpecificity: LowEfficiency: High |
| Lipid Nanoparticles (LNPs) | Synthetic lipid vesicles encapsulating cargo; fuse with cell membrane [8] [1]. | Low immunogenicity, tunable organ targeting (e.g., liver), FDA-approved for mRNA, suitable for redosing [8] [18] [5]. | Endosomal entrapment and degradation, primarily liver-tropic with current formulations [8] [1]. | mRNA, RNP, DNA [8] [1] | Safety: HighSpecificity: MediumEfficiency: Medium |
| Electroporation | Electrical pulse creates temporary pores in cell membrane for cargo entry [8]. | High efficiency for hard-to-transfect cells (e.g., stem cells), direct delivery, clinical validation (CASGEVY) [8] [5]. | Mostly restricted to ex vivo use, can impact cell viability [8] [1]. | RNP, mRNA, DNA [8] | Safety: HighSpecificity: MediumEfficiency: High |
A landmark demonstration of balancing the delivery triad is the first FDA-approved CRISPR therapy, CASGEVY. It successfully employs electroporation for the ex vivo delivery of RNP complexes into patient hematopoietic stem cells. This strategy maximizes specificity and safety (via RNP's transient activity) while achieving high efficiency in a clinically challenging cell type, offering a curative treatment for sickle cell disease and β-thalassemia [8] [5].
Application Note: An Integrated Workflow for In Vivo Liver Editing
The following workflow diagram and protocol detail a methodology for efficient in vivo gene editing, leveraging the high liver tropism of certain delivery vehicles.
Protocol: Systemic Administration of LNP-mRNA for Liver Gene Knockdown
This protocol is adapted from successful clinical trials for hereditary transthyretin amyloidosis (hATTR), where a single dose of LNP-mRNA achieved ~90% reduction of the disease-related TTR protein [5].
Materials & Reagents
- CRISPR-mRNA: Codon-optimized mRNA encoding SpCas9 or a high-fidelity variant, purified and sterile.
- sgRNA: Synthetic single-guide RNA targeting the gene of interest, HPLC-purified.
- LNP Formulation: Ionizable lipid (e.g., DLin-MC3-DMA), phospholipid, cholesterol, and PEG-lipid for nanoparticle self-assembly.
- Animal Model: Adult mice (e.g., C57BL/6).
- Delivery Equipment: Syringe and needle for IV injection (e.g., via tail vein).
- Analytical Tools: ELISA kit for target protein quantification, NGS platform for off-target analysis.
Procedure
- LNP Formulation: Formulate CRISPR-mRNA and sgRNA into LNPs using a microfluidic mixer. The aqueous phase containing the mRNA/gRNA is mixed with the ethanol phase containing dissolved lipids at a specific flow rate ratio to form stable, monodisperse particles. Dialyze the formulated LNPs against a sterile buffer (e.g., PBS, pH 7.4) to remove residual ethanol. Sterile-filter the final product through a 0.22 µm filter.
- Quality Control: Characterize the LNPs for particle size (targeting 70-100 nm), polydispersity index (PDI < 0.2), and mRNA encapsulation efficiency (>90%) using dynamic light scattering (DLS) and Ribogreen assays.
- Systemic Administration: Calculate the dose based on mRNA (e.g., 1-3 mg/kg). Gently warm the animal to dilate the tail vein. Slowly inject the LNP formulation intravenously via the tail vein. Monitor the animal for any acute adverse reactions.
- Efficacy Assessment: At defined timepoints post-injection (e.g., 7, 14, 28 days), collect blood samples via retro-orbital bleeding or terminal cardiac puncture. Isolate serum and quantify the level of the target protein using a validated ELISA.
- Specificity & Safety Profiling: At the study endpoint, harvest the liver and other potential off-target organs. Extract genomic DNA. Use unbiased methods like GUIDE-seq or CIRCLE-seq to comprehensively profile potential off-target sites. Sequence the on-target locus to determine the indel percentage.
Protocol: Rapid Screening of Gene Editing Outcomes via eGFP Disruption
This protocol provides a cell-based method for the high-throughput, quantitative assessment of delivery efficiency and DNA repair outcomes, enabling rapid iteration and optimization of delivery parameters [16].
Materials & Reagents
- Cell Line: HEK293T or other readily transfectable mammalian cell line.
- Lentiviral Vector: Plasmid for producing lentivirus encoding eGFP.
- CRISPR Components: Pre-designed sgRNA targeting the eGFP sequence and Cas9 (as pDNA, mRNA, or RNP).
- Transfection Reagent: Lipofectamine 2000 or similar for pDNA/mRNA delivery; or electroporation kit for RNP delivery.
- Instrumentation: Flow cytometer.
Procedure
- Generate eGFP-Expressing Cell Line: Produce lentiviral particles by co-transfecting HEK293T cells with the eGFP transfer plasmid and packaging plasmids (psPAX2, pMD2.G). Harvest the virus-containing supernatant, filter it, and transduce your target cell line. Use fluorescence-activated cell sorting (FACS) to select a pure population of eGFP-positive cells.
- Transfection with CRISPR Components: Seed eGFP-positive cells in a multi-well plate. Transfect the cells with the Cas9/sgRNA constructs using a method appropriate for your cargo (e.g., lipofection for pDNA/mRNA, electroporation for RNP). Include a non-targeting sgRNA as a negative control.
- Incubation and Harvest: Incubate the cells for 48-72 hours to allow for gene editing and turnover of the existing eGFP protein.
- Flow Cytometry Analysis: Harvest the cells, wash with PBS, and resuspend in a FACS-compatible buffer. Analyze the cells using a flow cytometer. Measure the fluorescence in the FITC (green) channel to detect eGFP loss and other channels (e.g., Pacific Blue) to detect potential BFP conversion if using a specific donor template [16].
- Data Interpretation: The percentage of cells that have lost eGFP fluorescence (FITC-negative) corresponds to the total gene editing efficiency, primarily resulting from NHEJ-induced indels. A shift to a blue fluorescence profile indicates successful HDR.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for CRISPR-Cas9 Delivery
| Research Reagent / Tool | Primary Function | Key Considerations for the Delivery Triad |
|---|---|---|
| High-Fidelity Cas9 Variants | Engineered Cas9 protein with reduced off-target activity [17]. | Directly enhances Specificity and Safety by minimizing unintended edits, potentially at a small cost to on-target Efficiency. |
| Selective Organ Targeting (SORT) LNPs | Engineered LNPs that modify natural tropism to target organs beyond the liver (e.g., spleen, lungs) [1]. | Dramatically improves Specificity by directing cargo to desired tissues, thereby improving therapeutic Efficiency and reducing off-target Safety risks. |
| Virus-Like Particles (VLPs) | Engineered viral capsids lacking viral genetic material; delivers functional Cas9-gRNA RNP complexes [18] [1]. | Improves Safety profile versus viral vectors (non-integrating, transient). Can enhance Efficiency of RNP delivery in vivo while maintaining high Specificity. |
| Base and Prime Editors | "CRISPR 2.0" systems that chemically alter a single base or search-and-replace a sequence without creating DSBs [17] [19]. | Major Safety and Specificity advancement by avoiding DSB-related genotoxicity and reducing off-target effects. Broadens therapeutic applications. |
| Unbiased Off-Target Assays | Methods like GUIDE-seq and CIRCLE-seq to genome-widely identify potential off-target sites [17]. | Critical for empirically measuring Specificity and validating the Safety profile of a chosen gRNA and delivery method. |
Navigating the Delivery Triad requires a strategic and balanced approach, where the choice of cargo, vehicle, and experimental protocol is dictated by the specific therapeutic or research goal. No single solution is universally superior; rather, the optimal strategy is context-dependent. The ongoing clinical success of ex vivo RNP delivery for hematopoietic diseases and in vivo LNP-mRNA delivery for liver-specific targets provides a robust framework and proof-of-concept for future therapies [5]. As the field progresses, emerging technologies—including novel capsids for targeted viral delivery, refined non-viral nanoparticles for systemic tissue targeting, and cleavage-free editing systems—are poised to further refine this balance, expanding the reach of CRISPR-based medicines to a broader array of genetic disorders [17] [1] [19].
Delivery in Action: Viral, Non-Viral, and Physical Methodologies
The efficacy of CRISPR-Cas9 genome editing is profoundly influenced by the delivery system used to introduce its components into target cells. Viral vectors, including adeno-associated virus (AAV), lentivirus (LV), and adenovirus (AdV), have emerged as leading vehicles for this purpose, each offering distinct advantages and challenges. Their performance directly impacts critical factors such as editing efficiency, specificity, and therapeutic safety [8] [20]. Within the context of a broader thesis on delivery methods for CRISPR-Cas9, this document provides detailed application notes and standardized protocols for employing these viral vectors in a research setting, supporting the development of next-generation gene therapies.
Comparative Analysis of Major Viral Vector Systems
The table below summarizes the core characteristics of AAV, lentiviral, and adenoviral vectors to guide appropriate selection for research applications.
Table 1: Key Characteristics of Viral Vectors for CRISPR-Cas9 Delivery
| Feature | Adeno-Associated Virus (AAV) | Lentivirus (LV) | Adenovirus (AdV) |
|---|---|---|---|
| Packaging Capacity | <4.7 kb [11] [1] [21] | ~8 kb [1] | Up to 36 kb [1] |
| Integration Profile | Predominantly episomal; non-integrating [21] | Integrates into host genome [1] | Non-integrating [1] |
| Transgene Expression Duration | Long-term (can persist for years) [11] | Long-term (stable expression) [1] | Transient [1] |
| Tropism & Specificity | High; serotype-dependent tissue tropism [11] [21] | Broad; can be pseudotyped to alter tropism [1] | Broad; can be modified for specificity [1] |
| Immunogenicity | Low; mild immune response [11] [1] | Moderate; HIV backbone raises safety concerns [1] | High; can trigger strong immune responses [1] |
| CRISPR Cargo Format | DNA (requires compact Cas versions or dual vectors) [11] | DNA (integrating) [1] | DNA (non-integrating) [1] |
Application Notes
Adeno-Associated Virus (AAV) Vectors
AAV vectors are a premier choice for in vivo gene therapy due to their excellent safety profile and sustained transgene expression [11]. A significant challenge is their limited packaging capacity (~4.7 kb), which is insufficient for the commonly used Streptococcus pyogenes Cas9 (SpCas9). Researchers have developed ingenious strategies to overcome this:
- Compact Cas Orthologs: Employing smaller Cas proteins, such as Staphylococcus aureus Cas9 (SaCas9, ~3.2 kb) or the even smaller Cas12f, allows for packaging of the entire CRISPR machinery into a single "all-in-one" vector [11] [22].
- Dual-Vector Systems: For larger nucleases, the Cas9 and guide RNA (gRNA) can be split across two separate AAV vectors. While this necessitates co-infection of the same cell, strategies like intein-mediated trans-splicing can reconstitute the full protein [11].
AAV serotype selection is critical as it dictates tissue tropism. For example, AAV5 is effective for retinal delivery (as in the clinical trial EDIT-101 for Leber Congenital Amaurosis), while AAV9 exhibits strong tropism for the liver and central nervous system [11] [21].
Lentiviral Vectors (LVs)
Lentiviral vectors are exceptional for ex vivo applications and functional genomics screens due to their ability to stably integrate into the host genome, including non-dividing cells [1]. This makes them ideal for creating stable cell lines for long-term gene expression studies. A primary safety consideration is the potential for insertional mutagenesis due to random integration, though the use of integrase-deficient LVs (IDLVs) can provide transient expression and mitigate this risk [23]. Their relatively large packaging capacity (~8 kb) easily accommodates SpCas9 and multiple gRNAs, enabling complex multiplexed editing experiments [1].
Adenoviral Vectors (AdVs)
Adenoviral vectors feature a very large packaging capacity (up to 36 kb), making them one of the few viral platforms capable of delivering SpCas9, multiple gRNAs, and even a donor DNA template for homology-directed repair (HDR) within a single particle [1]. They are non-integrating and provide high-level, transient transgene expression, which is advantageous for reducing long-term off-target effects. However, their high immunogenicity can trigger robust inflammatory responses, which may be a liability for therapeutic in vivo applications but can be harnessed for vaccine development [1].
Key Experimental Protocols
Protocol: Assessing CRISPR Editing Outcomes via eGFP-to-BFP Conversion
This protocol provides a high-throughput method to screen and quantify the efficiency of different CRISPR delivery systems by measuring the conversion of enhanced Green Fluorescent Protein (eGFP) to Blue Fluorescent Protein (BFP) in a cell population [16].
Table 2: Research Reagent Solutions for eGFP-to-BFP Assay
| Item | Function/Description |
|---|---|
| eGFP-Expressing Cell Line | Target cells providing a visual readout for editing. Can be generated via lentiviral transduction. |
| CRISPR Delivery System | Viral vectors (AAV, LV, AdV) or non-viral methods containing Cas9 and anti-eGFP gRNA. |
| Anti-eGFP gRNA | Guide RNA designed to target the eGFP sequence for cleavage. |
| HDR Donor Template | DNA template encoding BFP mutation with homology arms for precise repair. |
| Flow Cytometer | Instrument for quantifying the percentages of eGFP-positive and BFP-positive cells. |
Procedure:
- Cell Preparation: Generate or obtain a stably transduced cell line with uniform, high-level eGFP expression.
- Transfection/Transduction: Deliver the CRISPR-Cas9 components (as plasmid DNA, mRNA, or RNP) along with the HDR donor template using your chosen method (e.g., viral transduction).
- For viral delivery, transduce cells at an appropriate multiplicity of infection (MOI) determined by pilot experiments.
- Incubation: Culture the cells for 3-7 days to allow for genome editing and expression of the BFP phenotype.
- Harvesting and Analysis: Harvest the cells and analyze them using a flow cytometer.
- Measure fluorescence: Detect eGFP (excitation ~488 nm, emission ~510 nm) and BFP (excitation ~405 nm, emission ~450 nm).
- Data Interpretation:
- Knockout Efficiency: Calculate the percentage of cells that have lost eGFP fluorescence (eGFP-negative), indicating indels from NHEJ repair.
- HDR Efficiency: Calculate the percentage of cells that have gained BFP fluorescence (BFP-positive), indicating precise HDR-mediated editing.
Protocol: In Vivo Gene Editing Using AAV Vectors
This protocol outlines the key steps for performing in vivo genome editing in a mouse model using AAV vectors, a common approach for preclinical therapeutic studies [11].
Procedure:
- Vector Design and Production:
- Select Cas Ortholog: Choose a nuclease compatible with AAV packaging (e.g., SaCas9) if using an all-in-one system. Alternatively, design dual vectors for larger nucleases.
- Clone Components: Clone the expression cassettes for the Cas nuclease and gRNA(s) into the AAV vector backbone, ensuring they are flanked by inverted terminal repeats (ITRs).
- Package and Purify: Produce recombinant AAV particles using a triple-transfection system in HEK293T cells and purify via ultracentrifugation or chromatography.
- In Vivo Delivery:
- Administration Route: Choose based on target tissue (e.g., systemic intravenous injection for liver editing, subretinal injection for retinal editing).
- Dosage: Titrate the vector dose (e.g., (1 \times 10^{11} - 1 \times 10^{13}) vector genomes per animal) based on pilot studies and literature.
- Validation and Analysis:
- Harvest Tissues: After a suitable period (e.g., 2-4 weeks), harvest the target tissues.
- Assess Editing: Use next-generation sequencing (NGS) or T7E1 assay to quantify indel frequencies at the target locus.
- Evaluate Phenotype: Perform functional assays (e.g., immunohistochemistry, behavioral tests, biomarker analysis) to assess the physiological outcome.
Workflow and Pathway Diagrams
The following diagram illustrates the critical decision-making pathway for selecting and applying viral vectors in a CRISPR-Cas9 research project.
The clinical success of Lipid Nanoparticles (LNPs) in mRNA-based COVID-19 vaccines has catalyzed their rapid adoption as a premier delivery platform for CRISPR-Cas9 gene editing. LNPs provide a solution to one of the most significant challenges in therapeutic genome editing: the safe and efficient transport of CRISPR components into target cells. This document details the application of LNP technology for CRISPR delivery, providing a comparative analysis of cargo formats, step-by-step experimental protocols, and an overview of the current clinical landscape to aid researchers in transitioning this technology from concept to bench.
LNP Fundamentals and Mechanism of Action
LNPs are sophisticated, multi-component systems whose function is dictated by their precise composition.
1.1 Core Components: A standard LNP formulation for nucleic acid delivery includes four key lipids [24]:
- Ionizable Lipids: The most critical component (e.g., ALC-0315, SM-102). They are neutral at physiological pH but acquire a positive charge in acidic environments, enabling efficient mRNA encapsulation during formulation and facilitating endosomal escape post-cell entry [25] [26].
- Phospholipids: Helper lipids (e.g., DSPC) that contribute to the bilayer structure and stability of the particle.
- Cholesterol: A structural lipid that integrates into the LNP membrane, enhancing stability and facilitating cellular uptake.
- PEG-lipids: Located on the LNP surface, these lipids control particle size, prevent aggregation during storage and circulation, and modulate in vivo pharmacokinetics [24] [27].
1.2 Mechanism of Intracellular Delivery: The journey of an LNP from administration to protein expression or gene editing involves a defined cascade [28]:
- Cellular Uptake: LNPs are internalized by cells via endocytosis.
- Endosomal Trafficking: The LNP is encapsulated within an endosome, which acidifies as it matures.
- Endosomal Escape: The acidic environment of the endosome protonates the ionizable lipids, inducing a structural transition from an inverse micellar to an inverse hexagonal phase. This transition disrupts the endosomal membrane, releasing the nucleic acid payload into the cytoplasm [25].
- Payload Function: For CRISPR applications, the released mRNA is translated into the Cas9 protein, which complexes with the gRNA to form the active editing machinery.
The diagram below illustrates this key mechanism of endosomal escape.
Comparative Analysis of CRISPR Cargo Formats for LNP Delivery
CRISPR-Cas9 components can be delivered via LNPs in different formats, primarily as mRNA/sgRNA or as a pre-complexed Ribonucleoprotein (RNP). The choice of cargo significantly impacts editing efficiency, kinetics, and safety. A summary of the quantitative differences is provided in the table below.
Table 1: Comparison of LNP-Mediated CRISPR Cargo Formats [29] [30]
| Feature | mRNA/sgRNA | Cas9 RNP |
|---|---|---|
| Editing Efficiency (in vivo) | Up to 60% knockout in hepatocytes [30] | Minimal editing detected in mouse liver [30] |
| Onset of Action | Delayed (requires translation) | Immediate |
| Duration of Activity | Transient (hours to days) | Very short (hours) |
| Risk of Off-Target Effects | Moderate (prolonged Cas9 expression) | Lower (transient activity) |
| Particle Size | Smaller (~80 nm) [30] | Larger |
| Biodistribution (Systemic) | Primarily liver | Liver, spleen, and lungs [30] |
| Payload Protection | Better protection from nucleases [30] | Potentially less stable |
Protocols for LNP Formulation and Testing
This section provides detailed methodologies for formulating and evaluating LNPs for CRISPR delivery.
3.1 LNP Formulation via Ethanol Injection
- Principle: Lipids dissolved in an organic phase are rapidly mixed with an aqueous phase containing the nucleic acid payload, leading to spontaneous nanoparticle formation [26].
- Materials:
- Ionizable lipid, phospholipid, cholesterol, PEG-lipid
- Anhydrous ethanol
- CRISPR payload: mRNA, sgRNA, or Cas9 RNP complex in citrate buffer (pH 4.0)
- Microfluidic mixer or tangential flow filtration system
- Dialysis cassettes and PBS (pH 7.4)
- Procedure:
- Dissolve the lipid mixture (e.g., 50:10:38.5:1.5 molar ratio of ionizable lipid:DSPC:cholesterol:PEG-lipid) in ethanol to a final concentration of 10-20 mg/mL total lipids [26].
- Prepare the aqueous phase by dissolving the CRISPR payload in a citrate buffer (e.g., 25 mM, pH 4.0). An N/P ratio (moles of amine in lipid to moles of phosphate in nucleic acid) of 3:1 to 6:1 is typically optimal [26] [30].
- Rapidly mix the ethanolic lipid solution and the aqueous nucleic acid solution using a microfluidic device at a fixed flow rate (e.g., 1:3 volumetric ratio) to form LNPs.
- Immediately dialyze the formed LNPs against a large volume of PBS (pH 7.4) for at least 4 hours at 4°C to remove ethanol and balance the pH.
- Sterile-filter the final LNP formulation (0.22 µm pore size) and store at 4°C for short-term use or at -80°C for long-term storage with cryoprotectants like sucrose.
3.2 Protocol for In Vitro Gene Editing in Adherent Cell Lines
- Principle: LNPs are used to transfert cells in culture, and editing efficiency is quantified by analyzing target genomic DNA.
- Materials:
- Adherent cell line (e.g., HEK293T, HEPA 1-6) [30]
- Complete cell culture medium
- LNP formulation (from Protocol 3.1)
- Opti-MEM or similar serum-free medium
- Genomic DNA extraction kit
- PCR reagents and T7 Endonuclease I or tracking of indels by decomposition (TIDE) analysis reagents
- Procedure:
- Seed cells in a 24-well plate at a density of 1-2 x 10^5 cells/well and incubate for 24 hours to reach 60-80% confluency.
- Dilute the LNP formulation in Opti-MEM to the desired concentration.
- Remove the growth medium from the cells, wash with PBS, and add the LNP-Opti-MEM mixture.
- Incubate for 4-6 hours, then replace the transfection medium with fresh complete medium.
- Harvest cells 48-72 hours post-transfection and extract genomic DNA.
- Amplify the target genomic locus by PCR and analyze the PCR products using the T7E1 assay or Sanger sequencing followed by TIDE analysis to quantify indel percentages [29].
The workflow for this in vitro protocol is summarized below.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of LNP-based CRISPR delivery requires a suite of specialized reagents and equipment.
Table 2: Key Reagents and Materials for LNP-CRISPR Research
| Item | Function/Description | Example |
|---|---|---|
| Ionizable Lipid | pH-responsive lipid critical for encapsulation and endosomal escape. | ALC-0315, SM-102, ALC-0307 [24] |
| Cas9 mRNA | Template for in vivo production of the Cas9 nuclease. | Modified nucleotides for enhanced stability and reduced immunogenicity [27]. |
| Chemically Modified sgRNA | Guides Cas9 to the specific genomic target. | Synthetic sgRNA with phosphorothioate bonds for improved nuclease resistance [29]. |
| Microfluidic Mixer | Instrument for controlled, rapid mixing of lipid and aqueous phases to form uniform LNPs. | NanoAssemblr, Mikro-Technik mixing chips. |
| Dynamic Light Scattering (DLS) | Instrument for measuring LNP particle size, polydispersity index (PDI), and zeta potential. | Malvern Zetasizer. |
| T7 Endonuclease I Assay | Kit for detecting and quantifying CRISPR-induced indels at the target site. | New England Biolabs T7E1 kit. |
Clinical Translation and Future Directions
LNP-mediated CRISPR delivery has moved from proof-of-concept to clinical reality, demonstrating therapeutic potential in human trials.
5.1 Clinical Trial Highlights:
- hATTR Amyloidosis: Intellia Therapeutics' NTLA-2001, an LNP delivering CRISPR components targeting the TTR gene, achieved ~90% reduction in disease-causing protein levels after a single intravenous infusion, establishing a benchmark for in vivo gene editing [5].
- Personalized In Vivo Therapy: A landmark case in 2025 reported the development of a bespoke LNP-CRISPR therapy for an infant with CPS1 deficiency. The therapy was developed and administered within six months, and the patient safely received multiple doses, showing significant clinical improvement and establishing a regulatory precedent for rapid, personalized genomic medicine [5] [24].
5.2 Emerging Innovations and Challenges:
- Liver Tropism: A primary challenge is the inherent liver tropism of current LNPs. Research is actively focused on Selective Organ Targeting (SORT) molecules, which, when incorporated into LNPs, can redirect them to tissues like the lungs, spleen, and heart [24].
- Dosing Regimens: The low immunogenicity of LNPs enables re-dosing, a significant advantage over viral vectors. Clinical trials have successfully administered multiple LNP doses to enhance therapeutic effect, paving the way for "dosing to effect" paradigms [5] [24].
- Payload Capacity and Efficiency: Innovations like metal-ion-mediated mRNA enrichment (e.g., using Mn²⁺ to pre-condense mRNA) are being explored to double the payload capacity of LNPs, which could improve efficacy and reduce lipid-related toxicity [27].
LNPs have successfully pivoted from their foundational role in vaccines to becoming a versatile and powerful platform for CRISPR-Cas9 delivery. Their proven efficacy in clinical trials, combined with the flexibility for re-dosing and a favorable safety profile, positions them at the forefront of in vivo gene editing. Ongoing research aimed at overcoming challenges in tissue-specific targeting and payload optimization will further solidify LNPs as an indispensable tool in the development of next-generation genetic therapeutics.
The successful application of the CRISPR-Cas9 system in genetic research and therapeutic development is fundamentally dependent on the efficient delivery of its molecular components into target cells. Among the various strategies available, physical delivery methods—namely electroporation, microinjection, and magnetofection—offer distinct advantages and challenges. These techniques facilitate the direct introduction of CRISPR cargoes (plasmid DNA, mRNA, or ribonucleoprotein complexes) by temporarily disrupting cellular membranes or using physical forces to bypass them. This application note provides a comparative analysis of these three physical methods, summarizes key quantitative performance data in structured tables, and outlines detailed experimental protocols to assist researchers in selecting and optimizing these techniques for their specific CRISPR-Cas9 applications.
Physical delivery methods function by creating transient physical disruptions in the cell membrane or utilizing force to directly propel cargo into cells, thereby avoiding many of the biological barriers associated with viral and non-viral chemical methods [31] [8]. These techniques are particularly valuable for hard-to-transfect cells, such as primary cells and stem cells, and for applications requiring high precision and minimal extraneous material. The choice of physical method significantly impacts key outcome metrics including editing efficiency, cell viability, and experimental throughput. Furthermore, the format of the CRISPR cargo—whether as plasmid DNA, mRNA, or preassembled ribonucleoprotein (RNP) complexes—interacts with the delivery method to determine final editing success [32]. RNP delivery is often favored for its rapid activity and reduced off-target effects, as the complex is active immediately upon entry and quickly degraded [32].
Comparative Analysis and Performance Data
The table below provides a direct comparison of the three primary physical delivery methods across several critical parameters, offering a guide for initial method selection.
Table 1: Comparison of Physical CRISPR-Cas9 Delivery Methods
| Parameter | Electroporation | Microinjection | Magnetofection |
|---|---|---|---|
| Principle | Electrical pulses create temporary pores in cell membrane [8]. | Fine needle mechanically injects cargo directly into cytoplasm or nucleus [32]. | Magnetic force pulls nucleic acid-coated nanoparticles into cells [29]. |
| Cargo Compatibility | DNA, mRNA, RNP [32]. | DNA, mRNA, RNP [32]. | RNP (e.g., complexed with SPIONs) [29]. |
| Typical Editing Efficiency | Very High (Up to 95% in amenable cell lines) [29]. | High (e.g., ~40% in HepG2 cells) [8]. | Variable (Can be limited by post-entry barriers despite efficient uptake) [29]. |
| Cell Viability | Variable; can be low under high-efficiency parameters [29]. | Low; technically demanding and damaging to cells [32]. | Generally high biocompatibility [29]. |
| Throughput | High (can process millions of cells). | Very Low (single-cell level). | Moderate to High. |
| Key Advantages | High efficiency, works on a broad range of cell types [32]. | Precise control over delivered dose, large cargo capacity [32]. | Low cytotoxicity, potential for targeted delivery with magnetic fields [29]. |
| Key Limitations | Can be damaging to cells, requires optimization of pulse parameters [29] [32]. | Technically demanding, low throughput, requires specialized equipment [32]. | Editing efficiency may not correlate with uptake; requires specialized nanoparticles [29]. |
The following table summarizes specific experimental data from published studies, illustrating how performance varies with specific protocols and cell types.
Table 2: Quantitative Performance Data from Representative Studies
| Delivery Method | Cell Type/Model | Cargo Format | Key Parameters | Reported Editing Efficiency | Cell Viability / Notes | Source |
|---|---|---|---|---|---|---|
| Electroporation | SaB-1 (Sea Bream) Cell Line | RNP (3 µM, synthetic sgRNA) | 1800 V, 20 ms, 2 pulses | Up to 95% | ~20% survival | [29] |
| Electroporation | DLB-1 (Sea Bass) Cell Line | RNP (3 µM) | 1700 V, 20 ms, 2 pulses | ~28% | Sharply reduced viability | [29] |
| Electroporation | HSPCs (Human) | RNP (CASGEVY ex vivo therapy) | Not Specified | Up to 90% indels | N/A | [8] |
| Electroporation | Mouse Zygotes | RNP | Not Specified | Highly Efficient | N/A | [8] |
| Microinjection | HepG2 Cells | Not Specified (GFP reporter) | Not Specified | ~40% | N/A | [8] |
| Magnetofection | DLB-1 & SaB-1 Cell Lines | RNP with SPIONs@Gelatin | Not Specified | No detectable editing | Efficient uptake, highlighting post-entry barriers | [29] |
Experimental Protocols
Protocol for RNP Delivery via Electroporation
This protocol is adapted from a study achieving high editing efficiency in marine fish cell lines and is applicable to many mammalian cell types [29].
Key Research Reagent Solutions:
- CRISPR-Cas9 RNP Complex: Purified Cas9 protein complexed with synthetic, chemically modified sgRNA (e.g., from Synthego) at a 3 µM final concentration [29].
- Electroporation Buffer: Opti-MEM or cell line-specific electroporation buffer.
- Cell Culture Media: Standard growth media supplemented with serum.
Methodology:
- Cell Preparation: Harvest and count the target cells. Centrifuge and wash the cell pellet twice with electroporation buffer to remove all traces of serum and antibiotics. Resuspend the cells at a high concentration (e.g., 1-5 x 10^6 cells/mL) in the electroporation buffer.
- RNP Complex Formation: Pre-complex the recombinant Cas9 protein with the sgRNA at a molar ratio of 1:1.2 to 1:2 (Cas9:sgRNA). Incubate the mixture at room temperature for 10-20 minutes to allow for RNP formation.
- Electroporation Setup: Combine the cell suspension with the pre-formed RNP complexes in an electroporation cuvette. Gently mix by pipetting. The final RNP concentration is typically 2-5 µM [29].
- Pulse Delivery: Place the cuvette in the electroporator and deliver the electrical pulse. Critical: Parameters must be optimized for each cell type. Example conditions from the literature include:
- Post-Electroporation Recovery: Immediately after pulsing, transfer the cells from the cuvette into a pre-warmed culture plate containing complete medium. Incubate the cells at standard conditions (37°C, 5% CO2).
- Analysis: Assess editing efficiency via T7E1 assay, TIDE analysis, or NGS 48-72 hours post-electroporation. Cell viability can be determined 24 hours post-delivery using a trypan blue exclusion assay.
Protocol for Microinjection
This protocol outlines the general workflow for delivering CRISPR components via microinjection, commonly used for zygotes and single-cell applications [32] [8].
Key Research Reagent Solutions:
- Injection Sample: CRISPR cargo (e.g., Cas9 mRNA and sgRNA, or pre-assembled RNP) in a nuclease-free injection buffer.
- Holding Pipette and Injection Needle: Specialized glass capillaries.
- Microinjection System: Comprising an inverted microscope, a micromanipulator, and a microinjector.
Methodology:
- Sample Preparation: Prepare the injection mixture. For RNP delivery, combine Cas9 protein and sgRNA at a high concentration (e.g., 100-500 ng/µL) in an appropriate injection buffer and incubate prior to loading.
- Cell Immobilization: Secure the target cell (e.g., a zygote) using a holding pipette under the microscope.
- Needle Insertion: Carefully advance the injection needle through the zona pellucida (if present) and the cell membrane into the cytoplasm or pronucleus.
- Cargo Delivery: Apply a brief positive pressure pulse to expel a precise volume of the CRISPR cargo. A visible slight swelling of the cell indicates successful delivery.
- Needle Retraction: Gently retract the injection needle.
- Post-Injection Culture and Analysis: Wash the injected cells and transfer them to a culture medium for recovery and further development. Genotype the resulting embryos or cells to determine editing efficiency.
Protocol for Magnetofection
This protocol describes the use of magnetic nanoparticles, such as gelatin-coated SPIONs, for the delivery of CRISPR RNP complexes [29].
Key Research Reagent Solutions:
- Magnetic Nanoparticles: Gelatin-coated Superparamagnetic Iron Oxide Nanoparticles (SPIONs@Gelatin) [29].
- RNP Complex: Pre-assembled Cas9-sgRNA RNP.
- Magnetofection Reagent: A commercial reagent or protocol for conjugating RNPs to nanoparticles.
- Platform Magnet: A magnet designed to create a magnetic field across the culture vessel.
Methodology:
- RNP-Nanoparticle Complex Formation: Conjugate the pre-assembled RNP complexes to the surface of the magnetic nanoparticles according to the manufacturer's instructions. This may involve incubating the two components together to allow for electrostatic or covalent binding.
- Cell Preparation: Seed and culture the target cells in a multi-well plate until they reach 50-70% confluency.
- Transfection: Add the RNP-nanoparticle complexes directly to the cell culture medium. Gently swirl the plate to ensure even distribution.
- Magnetic Field Application: Place the culture plate on a platform magnet for a specified period (typically 15-30 minutes) to draw the magnetic particles onto the cell surface.
- Incubation and Analysis: Remove the plate from the magnet and continue incubating the cells under standard conditions. Analyze editing efficiency and cellular uptake after 48-72 hours. Note that efficient cellular uptake does not always guarantee successful gene editing, as post-entry barriers can be a significant limitation [29].
Workflow and Decision Pathways
The following diagram illustrates the key decision-making process for selecting and implementing a physical delivery method for CRISPR-Cas9.
Decision Workflow for Physical CRISPR Delivery
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Physical Delivery
| Item | Function/Description | Example Application / Note |
|---|---|---|
| Synthetic sgRNA | Chemically modified guide RNA for enhanced stability and reduced immunogenicity. | Outperformed in vitro transcribed (IVT) sgRNA, achieving up to 95% editing in electroporation [29]. |
| Recombinant Cas9 Protein | High-purity, endotoxin-free nuclease for forming RNP complexes. | Essential for RNP-based delivery in electroporation and microinjection [32]. |
| Electroporation System | Instrument that delivers controlled electrical pulses to cells (e.g., Neon, Amaxa). | Must be compatible with cuvettes or strips for the cell type being used. |
| Microinjection System | Comprises a microscope, micromanipulator, and microinjector for precise delivery. | Used for pronuclear or cytoplasmic injection in zygotes and large cells [32]. |
| Magnetic Nanoparticles (SPIONs) | Superparamagnetic iron oxide nanoparticles, often coated (e.g., with gelatin), for magnetofection. | Used to deliver RNP complexes; enables efficient uptake but may face post-entry barriers [29]. |
| Platform Magnet | Creates a magnetic field to pull nanoparticle complexes onto cultured cells. | Critical for achieving localized and efficient delivery in magnetofection protocols. |
Electroporation, microinjection, and magnetofection are powerful physical methods for delivering the CRISPR-Cas9 system, each with a unique profile of efficiency, viability, and applicability. Electroporation stands out for high-throughput and high-efficiency editing, microinjection for unparalleled precision in single-cell applications, and magnetofection for its potential for high viability and targeted delivery. The choice of method is not one-size-fits-all and must be informed by the target cell type, the desired cargo format, and the specific experimental goals. As the field of gene editing advances, continued optimization of these physical protocols will be crucial for unlocking the full potential of CRISPR-based research and therapies.
The therapeutic potential of CRISPR-Cas9 gene editing is fundamentally constrained by the availability of safe and efficient delivery vehicles. Viral vectors, while efficient, raise concerns regarding immunogenicity, cargo limitations, and long-term persistence. Consequently, extracellular vesicles (EVs) and virus-like particles (VLPs) have emerged as promising non-viral platforms that combine favorable delivery characteristics with enhanced safety profiles [33] [9]. This application note details the latest protocols and quantitative performance data for EV and VLP-mediated CRISPR-Cas9 delivery, providing researchers with practical methodologies for implementing these platforms in gene editing applications.
EVs are biological nanoparticles that play a key role in intercellular communication, while VLPs are engineered nanostructures that mimic viral architecture without containing viral genetic material [7] [34]. The table below summarizes the key characteristics and performance metrics of recently developed EV and VLP platforms for CRISPR-Cas9 delivery.
Table 1: Performance Comparison of Recent EV and VLP Platforms for CRISPR-Cas9 Delivery
| Platform & Study | Cargo Type | Loading Strategy | Target Application | Editing Efficiency (Key Metric) | Notable Advantage |
|---|---|---|---|---|---|
| Modular EV [7] | Cas9 RNP, ABE8e, dCas9-VPR | MS2 aptamer/MCP fusion to CD63 + UV-cleavable linker | Genetic engineering & transcriptional regulation | ~270-fold increase in sgRNA loading | Modular; applicable to multiple Cas9 variants |
| ARMMs [35] | Cas9 RNP | Direct ARRDC1-Cas9 fusion | APP gene editing in neuronal cells (Alzheimer's model) | Significant reduction in amyloid peptides | Efficient packaging and budding |
| Myristoylated-EV [36] | Cas9 RNP | N-myristoylation of Cas9 protein | Androgen receptor silencing in prostate cancer | Attenuated cancer cell proliferation | Enhanced RNP encapsulation |
| RIDE VLP [33] | Cas9 RNP | Engineered enveloped VLP | Ocular & Huntington's disease models | Robust, localized editing in immune-privileged sites | Cell-selective targeting; low immunogenicity |
| SFV-based VLP [37] | mRNA, Protein, RNP | Fusion to truncated capsid protein | Broad in vitro delivery (including hard-to-transfect cells) | Dose-dependent indel formation | Programmable tropism; large cargo capacity (~10 kb) |
| eVLPs for wet AMD [38] | Cas9 RNP (anti-VEGFA) | MMLVgag–3xNES–Cas9 fusion | Vegfa knockout in mouse retinal pigment epithelium | Up to 99% indel in vitro; 16.7% in vivo | Efficient RNP delivery to retinal tissue |
The following workflow diagram illustrates the general experimental process for developing and utilizing these platforms, from initial engineering to functional validation.
Detailed Protocols for EV-Mediated CRISPR Delivery
Modular EV Platform via Aptamer-Based Loading
This protocol describes a versatile strategy for loading Cas9 ribonucleoprotein (RNP) complexes into EVs using high-affinity RNA aptamers, allowing for the delivery of various CRISPR effectors without direct fusion to EV membrane proteins [7].
Key Reagents:
- Plasmids: Expression vectors for MCP-CD63 fusion protein, Cas9 (or variants), and MS2-sgRNA.
- Cells: HEK293T cells for EV production.
- Buffers: Standard cell culture and purification buffers.
Step-by-Step Workflow:
- Producer Cell Transfection: Co-transfect HEK293T cells with plasmids expressing the MCP-CD63 loading construct, the desired Cas9 variant, and the MS2-sgRNA using a standard transfection reagent. The MS2 aptamers are incorporated into the tetraloop and second stem-loop of the sgRNA.
- EV Biogenesis and Loading: Incubate cells for 48 hours to allow for intracellular RNP formation and loading into budding EVs via the MCP-MS2 interaction.
- EV Harvest and Purification: Collect conditioned media and isolate EVs using a two-step purification process:
- Tangential Flow Filtration (TFF) to concentrate the vesicles.
- Size Exclusion Chromatography (SEC) to separate EVs from protein contaminants.
- Cargo Release Activation (Optional): For constructs containing a UV-cleavable linker (e.g., PhoCl), expose isolated EVs to UV light to release the RNP cargo from the EV membrane upon internalization.
- Validation: Confirm EV isolation and Cas9 loading via Nanoparticle Tracking Analysis (NTA), Western Blot (for CD63, ALIX, TSG101, and Cas9), and qPCR/ddPCR for sgRNA quantification.
Typical Results: This method yields EVs with a mode size of ~75 nm and demonstrates a significant enrichment of Cas9 protein (~270-fold increase in sgRNA) compared to controls without the MCP-CD63 construct [7].
ARMMs for Neuronal Gene Editing
This protocol utilizes Arrestin Domain-Containing Protein 1-Mediated Microvesicles (ARMMs) for packaging and delivering CRISPR-Cas9, showing high efficiency in editing neuronal cells [35].
Key Reagents:
- Plasmids: Expression vectors for ARRDC1-Cas9 fusion (full-length or shortened sARRDC1) and VSV-G.
- Cells: Appropriate producer cell line (e.g., HEK293T) and target neuronal cells (e.g., for APP gene editing).
Step-by-Step Workflow:
- Fusion Construct Design: Generate fusion constructs where Cas9 is directly fused to the C-terminus of ARRDC1 (or sARRDC1). Co-express VSV-G to enhance ARMMs budding and Cas9 encapsulation.
- Particle Production: Transfect producer cells with the ARRDC1-Cas9 and VSV-G plasmids.
- ARMMs Collection and Purification: Collect particles from the conditioned media 48-72 hours post-transfection and purify using standard EV isolation techniques.
- Target Cell Transduction: Apply purified ARMMs to target neuronal cells (e.g., for APP gene editing in an Alzheimer's model).
- Efficiency Assessment: Evaluate gene editing via indel measurement and functional assays (e.g., reduction of pathogenic amyloid peptides).
Typical Results: The shorter sARRDC1 fusion proves particularly effective for enhancing Cas9 packaging. The combination with VSV-G improves budding and leads to significant editing of the endogenous APP gene in human neuronal cells [35].
Detailed Protocols for VLP-Mediated CRISPR Delivery
RIDE VLP Platform for Cell-Selective Editing
The RIDE (RNP Integrating with Designer Envelope) platform is a modular VLP system designed for transient, cell-selective genome editing with a favorable immunological profile [33].
Key Reagents:
- Core Components: Engineered VLPs for RNP delivery, customizable envelope proteins (e.g., single-chain antibodies, DARPins) for targeting.
- Cells: Producer and target cells.
Step-by-Step Workflow:
- VLP Production: Generate VLPs in producer cells (e.g., HEK293T) co-transfected with Gag-Pol, Cas9-sgRNA RNP, and the engineered envelope protein.
- Purification: Purify VLPs from the cell culture supernatant via ultracentrifugation or chromatography.
- Cell Targeting and Transduction: Incubate purified RIDE VLPs with target cells. The custom envelope proteins mediate specific binding and entry.
- Efficiency and Safety Validation:
- Quantify editing efficiency via NGS or T7E1 assay.
- Assess specificity and off-target effects.
- Evaluate immunogenicity (e.g., anti-Cas9 antibody response).
Typical Results: The RIDE platform achieves robust and localized gene editing in preclinical models (e.g., ocular neovascular disease, Huntington's disease). It demonstrates minimal innate immune activation and no detectable anti-Cas9 IgG antibodies, supporting its potential for repeat dosing [33].
SFV-based VLP for Programmable Delivery
This protocol employs a streamlined Semliki Forest Virus (SFV)-based VLP backbone, engineered for programmable tissue-specific gene delivery of various cargos, including RNPs [37].
Key Reagents:
- Plasmids: SFV backbone with minimal viral elements, genes for capsid and envelope proteins, and the transgene cargo (mRNA, protein, or RNP).
- Cells: A broad range of target cell lines.
Step-by-Step Workflow:
- System Customization: Engineer the SFV backbone by deleting all viral protein-coding sequences, retaining only the necessary elements for capsid assembly and envelope binding.
- Cargo Packaging:
- For RNP delivery: Fuse Cas9 to a truncated capsid protein (e.g., Cd118) and co-package with sgRNA.
- VLP Assembly and Harvest: Transfert producer cells to assemble and release VLPs. Collect and purify the supernatant.
- Tropism Expansion (Optional): Engineer the envelope protein via rational peptide insertion or pseudotyping to alter or enhance targeting capabilities (e.g., for BBB penetration, muscle targeting).
- Functional Assay: Transduce target cells and assess delivery efficiency (e.g., luciferase activity), RNP function (indel formation), and cargo integrity.
Typical Results: This SFV-VLP system shows broad in vitro delivery capabilities, outperforming AAV9 and Lipofectamine in hard-to-transfect cell lines. It successfully packages large cargos (up to 10 kb) and mediates functional RNP delivery in a dose-dependent manner [37].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for EV and VLP CRISPR Delivery
| Reagent / Material | Function / Role | Example Usage |
|---|---|---|
| MS2-MCP System | High-affinity RNA-protein interaction for cargo loading into EVs. | Modular EV platform for loading Cas9 RNP [7]. |
| ARRDC1/sARRDC1 | Key protein that mediates the budding of ARMMs from the plasma membrane. | Direct fusion to Cas9 for packaging into ARMMs [35]. |
| VSV-G Envelope Protein | Enhances particle budding and fusion with target cell membranes, broadening tropism. | Co-expression improves ARMMs yield and VLP entry efficiency [35]. |
| UV-Cleavable Linker (PhoCl) | Allows for controlled release of cargo from the vesicle membrane upon UV exposure. | Enables light-activated RNP release in the modular EV platform [7]. |
| Engineered Envelope Proteins | Provides cell-specific targeting capabilities to VLPs (e.g., DARPins, scFvs). | Enables selective cell targeting in the RIDE VLP platform [33]. |
| Truncated Capsid Protein (e.g., Cd118) | Facilitates the packaging of bulky protein cargo, such as Cas9 fusion proteins, into VLPs. | Used in SFV-based VLPs for efficient RNP delivery [37]. |
The logical relationships and critical engineering strategies for these platforms are summarized in the diagram below.
The transformative potential of CRISPR-Cas9 genome editing in medicine is fundamentally constrained by a single critical factor: the safe and efficient delivery of editing machinery to target cells. The clinical landscape is divided into two primary methodologies—ex vivo editing, where cells are genetically modified outside the body before transplantation, and in vivo editing, where therapeutic agents are administered directly to the patient. The choice between these approaches dictates the delivery strategy, cargo format, and ultimately, the therapeutic outcome [39] [1]. This application note delineates the current state of CRISPR-based therapies, providing detailed protocols and quantitative comparisons to guide researchers in navigating this complex field. The recent approval of Casgevy for sickle cell disease and transfusion-dependent beta thalassemia marks a pivotal milestone, demonstrating that CRISPR-based therapies can provide functional cures for genetic disorders [5] [40].
Ex Vivo Cell Engineering: Protocols and Applications
Ex vivo cell engineering involves extracting specific cell types from a patient, modifying them genetically in a controlled laboratory setting, and then reinfusing the edited cells back into the patient. This approach allows for precise quality control of the edited product but requires complex and costly manufacturing processes.
Case Study 1: Engineering Hematopoietic Stem Cells for Sickle Cell Disease
Therapeutic Goal: Disrupt the BCL11A gene to reactivate fetal hemoglobin expression, thereby compensating for the defective adult hemoglobin in sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT) [40].
Detailed Protocol for Ex Vivo HSC Editing:
- Cell Sourcing and Isolation: Collect CD34+ hematopoietic stem and progenitor cells (HSPCs) from the patient via apheresis, followed by immunomagnetic selection for CD34+ cells.
- Electroporation of CRISPR Components: Deliver the CRISPR-Cas9 system—typically as a ribonucleoprotein (RNP) complex of Cas9 protein and guide RNA—into the isolated HSPCs via electroporation. The use of RNP complexes minimizes off-target effects and enables rapid editing with transient activity [1] [41].
- Quality Control and Expansion: Post-electroporation, cells are expanded in culture medium supplemented with cytokines (SCF, TPO, FLT3-L) to maintain stemness and promote recovery.
- Patient Conditioning and Reinfusion: The patient undergoes myeloablative conditioning (e.g., with busulfan) to create niche space in the bone marrow. The validated, edited CD34+ cells are then reinfused into the patient [40].
Clinical Outcomes: Clinical trial data for Casgevy demonstrated that 25 of 27 TBT patients were freed from transfusion dependence, and 16 of 17 SCD patients were free of vaso-occlusive crises, with effects sustained for over three years in some cases [40].
Advanced Protocol: Peptide-enabled Ribonucleoprotein Delivery (PERC) for Primary Immune Cells
The PERC system presents an advanced, hardware-free alternative to electroporation for ex vivo editing, offering high efficiency with reduced impact on cell viability and phenotype [42].
Step-by-Step PERC Protocol:
- Reagent Preparation:
- CRISPR RNP Complex Formation: Complex a purified Cas9 or Cas12a protein with a chemically synthesized guide RNA (final typical working concentration: 5 µM RNP) by incubating at room temperature for 10-15 minutes.
- Peptide Transduction Agent Preparation: Prepare a stock solution of the amphiphilic peptide (e.g., in water or PBS).
- Delivery Mixture Assembly: Combine the pre-formed RNP complex with the peptide transduction agent at a defined molar ratio (e.g., 1:30 RNP:Peptide) and incubate for 15-30 minutes to allow nanoparticle formation.
- Cell Transduction:
- Harvest and count the primary human T cells or HSPCs. Ensure T cells are activated prior to editing.
- Resuspend the cells in the prepared RNP-peptide mixture at a density of 1-5 million cells per mL.
- Incubate the cell-transduction mixture for 1-3 hours at 37°C under standard cell culture conditions.
- Post-Transduction Processing: After incubation, wash the cells to remove the delivery reagent and resuspend them in fresh culture medium for further expansion or analysis. For precise knock-in, the protocol can be co-delivered with an adeno-associated virus (AAV) providing the homology-directed repair (HDR) template [42].
Key Advantages: This gentle method allows for multiple rounds of delivery to increase editing efficiency without significant loss of cell health. Efficiencies can surpass 90% for gene knockout in primary T cells and HSPCs [42].
Quantitative Data: Ex Vivo Clinical Trial Outcomes
Table 1: Summary of Key Ex Vivo CRISPR Clinical Trials and Outcomes
| Therapy / Trial | Target / Condition | Delivery Method | Key Outcome Measure | Result | Reference |
|---|---|---|---|---|---|
| Casgevy | BCL11A / SCD & TBT | Electroporation of RNP | Freedom from vaso-occlusive crises (SCD); Transfusion independence (TBT) | 94% (16/17) SCD patients crisis-free; 93% (25/27) TDT patients transfusion-independent | [40] |
| EDIT-101 | CEP290 / LCA10 | AAV5 (subretinal injection) | Vision improvement | First in vivo CRISPR therapy administered; Phase 1/2 trials ongoing | [9] |
| CAR-T for NSCLC | PD-1 / NSCLC | Not Specified (Ex Vivo) | Safety & Feasibility | Demonstrated safety and therapeutic potential for large-scale trials | [9] |
| PERC Platform | Multiple / Primary T cells & HSPCs | Peptide-mediated RNP | Gene Knockout Efficiency | >90% editing efficiency in primary T cells and HSPCs | [42] |
In Vivo Therapeutic Delivery: Case Studies and Protocols
In vivo delivery involves the systemic or local administration of CRISPR therapeutics directly into the patient, targeting cells within their native physiological environment. This approach poses significant delivery challenges but offers a less invasive and more scalable treatment modality.
Case Study 1: Lipid Nanoparticle Delivery for Hereditary Transthyretin Amyloidosis (hATTR)
Therapeutic Goal: Knock out the TTR gene in hepatocytes to reduce the production of misfolded transthyretin protein, the driver of hATTR pathology [5] [40].
Mechanism of Action: The systemically administered LNP is trafficked to the liver. Following cellular uptake and endosomal escape, the Cas9 mRNA is translated into protein in the cytoplasm. The Cas9 protein and sgRNA form a complex in the nucleus, where they induce a double-strand break in the TTR gene. Repair via the error-prone non-homologous end joining (NHEJ) pathway leads to gene disruption [39] [5].
Clinical Outcomes: In a Phase I trial, a single intravenous infusion of the LNP-formulated CRISPR therapy (NTLA-2001) resulted in a dose-dependent and durable reduction of serum TTR protein levels, with an average reduction of approximately 90% [5]. This was the first trial to demonstrate systemic in vivo gene editing in humans.
Case Study 2: In Vivo Engineering for Rare Genetic Disease
Therapeutic Goal: Rapidly develop and administer a personalized CRISPR therapy for an infant with a rare, life-threatening genetic disease, CPS1 deficiency [5].
Protocol and Workflow: This landmark case established a regulatory and manufacturing pathway for bespoke in vivo therapies. The process, from project initiation to treatment, was completed in six months.
- Target Identification & Component Design: Identify the causative mutation and design sgRNAs and Cas9 mRNA targeting the specific genomic locus.
- LNP Formulation & QA/QC: Encapsulate the CRISPR payload (mRNA and sgRNA) into clinical-grade lipid nanoparticles.
- Regulatory Review: Submit an Investigational New Drug (IND) application to the FDA, leveraging prior data on the LNP delivery platform.
- Clinical Administration: Administer the therapy via intravenous infusion. The use of LNPs allowed for multiple doses to maximize editing efficiency, which is not feasible with viral vectors due to immunogenicity [5].
Outcome: The patient (KJ) safely received three doses, showed improvement in symptoms, decreased dependence on medications, and was successfully discharged home [5].
Quantitative Data: In Vivo Delivery Systems and Clinical Progress
Table 2: Comparison of Major In Vivo CRISPR Delivery Systems
| Delivery System | Cargo Format | Key Advantages | Key Limitations | Clinical Stage |
|---|---|---|---|---|
| Lipid Nanoparticles (LNPs) | mRNA, sgRNA | High delivery efficiency to liver; Potential for re-dosing; Transient activity reduces off-target risks | Limited tropism beyond liver; Endosomal escape is inefficient in some tissues; Immunogenicity concerns | Phase 3 (e.g., hATTR, HAE) [5] |
| Adeno-Associated Virus (AAV) | DNA | Strong, sustained expression; Broad tissue tropism (serotype-dependent) | Small payload capacity (<4.7 kb); Pre-existing immunity in population; Risk of persistent off-target editing | Phase 1/2 (e.g., LCA10) [39] [1] |
| Extracellular Vesicles (EVs)/ARMMs | Protein (RNP) | Low immunogenicity; Natural homing properties; Potential for engineering | Manufacturing complexity; Heterogeneity; Low and variable loading efficiency | Preclinical [35] |
| Virus-Like Particles (VLPs) | Protein (RNP) | Transient delivery; High editing efficiency; Reduced off-target risk | Manufacturing challenges; Cargo size limitations; Optimizing tissue targeting | Preclinical (efficient delivery to neurons shown) [43] |
Successful CRISPR-Cas9 experimentation, whether ex vivo or in vivo, relies on a suite of core reagents and engineered components.
Table 3: Essential Research Reagent Solutions for CRISPR-Cas9 Workflows
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| CRISPR Nuclease (Cas9, Cas12a) | Effector protein that creates a double-strand break at the target DNA site. | Size (critical for AAV packaging), fidelity (HF variants), PAM requirement, specificity [39] [1]. |
| Guide RNA (sgRNA) | RNA molecule that directs the Cas nuclease to the specific genomic target via Watson-Crick base pairing. | Specificity (minimize off-targets), efficiency (on-target activity), chemical modification (stability) [41]. |
| Delivery Vehicle (LNPs, AAV, EVs) | Physically encapsulates and delivers CRISPR cargo to target cells, protecting it from degradation. | Tropism, cargo capacity (AAV: <4.7kb), transfection/transduction efficiency, immunogenicity, cost [39] [1] [35]. |
| HDR Donor Template | Exogenous DNA template used by the cell's HDR pathway to introduce precise edits (knock-ins, corrections). | Format (ssODN, dsDNA, AAV), length of homology arms, modification (e.g., silent mutations to prevent re-cutting) [39] [41]. |
| Cell Culture & Expansion Media | Supports the health, viability, and proliferation of cells during and after the editing process. | Serum-free formulations for clinical work, cytokine cocktails (for HSCs), activation media (for T cells) [42] [40]. |
| Electroporation/Transfection System | Creates transient pores in the cell membrane to allow intracellular entry of CRISPR cargo (RNP, DNA). | Parameters (voltage, pulse length), cell type-specific protocols, impact on cell viability [1] [41]. |
Visualizing Workflows and Mechanisms
Ex Vivo Cell Engineering Workflow
In Vivo LNP Delivery Mechanism
Overcoming Hurdles: Strategies for Enhancing Efficiency and Safety
A paramount challenge in therapeutic CRISPR-Cas9 application is the occurrence of off-target effects, where unintended edits are made at genomic sites with sequence similarity to the target. These effects can confound experimental results and pose significant safety risks in clinical settings, including the potential activation of oncogenes [44]. The risk profile is particularly acute for in vivo gene therapies, where edits cannot be reversed post-administration, underscoring the necessity of robust off-target mitigation strategies integrated within delivery system designs [1] [44]. This document details protocols for selecting high-fidelity Cas variants and designing optimized guide RNAs (gRNAs) to achieve precise genome editing.
High-Fidelity Cas Variants
The wild-type Streptococcus pyogenes Cas9 (SpCas9) exhibits a tolerance for 3-5 base pair mismatches between the gRNA and genomic DNA, leading to promiscuous cleavage [44]. High-fidelity variants engineered for reduced off-target activity are crucial for therapeutic applications.
Mechanism of Action
These variants achieve higher specificity through enhanced structural rigidity, particularly in the REC3 domain, which strengthens the energy requirement for DNA strand separation and duplex formation. This reduces tolerance for gRNA-DNA mismatches [45].
Selection Guide
The choice of nuclease involves a balance between specificity and efficiency. High-fidelity Cas9 variants are the default for most knockout applications, while Cas12a or engineered systems like OpenCRISPR-1 offer advantages for specific targeting or enhanced specificity [1] [45]. Nickases and base editors provide alternative pathways that avoid double-strand breaks, further minimizing off-target risks [44].
Table 1: Comparison of High-Fidelity Cas Variants
| Editor Name | Parent Nuclease | Key Feature | Reported Specificity Improvement | Considerations |
|---|---|---|---|---|
| OpenCRISPR-1 | AI-generated Cas9 | Designed de novo using large language models; ~400 mutations from SpCas9 [45]. | Comparable or improved vs. SpCas9 [45]. | Demonstrates compatibility with base editing; high sequence novelty. |
| hfCas12Max | Cas12 | Engineered for minimal size (1080 aa) and high fidelity [1]. | High editing efficiency with reduced off-targets [1]. | Smaller size enables easier packaging into AAV vectors [1]. |
| eSpCas9(1.1) | SpCas9 | Altered positive charges in the REC3 domain to reduce off-target binding [44]. | Reduced off-target cleavage; variable on-target efficiency. | An early engineered high-fidelity variant; may have reduced on-target activity in some contexts. |
| Cas9 Nickase (nCas9) | SpCas9 | Catalytically inactivated in one DNA cleavage domain (makes single-strand breaks) [44]. | Paired nicking strategy drastically reduces off-target effects. | Requires two adjacent gRNAs for a single edit, which can complicate delivery. |
gRNA Design Optimization
Careful gRNA design is the most direct method to minimize off-target effects. The objective is to select a guide sequence with maximal uniqueness in the genome.
In Silico Design and Selection Protocol
This protocol outlines the steps for selecting optimal gRNAs using computational tools.
Materials:
- Target Genomic Sequence: FASTA format for the region of interest.
- gRNA Design Software: CRISPOR, ChopChop, or Synthego's guide design tool.
- Reference Genome: The appropriate reference (e.g., GRCh38 for human).
Procedure:
- Input Target Sequence: Provide the 200-500 bp genomic sequence flanking your intended target site into the design software.
- Generate gRNA Candidates: The tool will output all possible gRNAs in the region.
- Analyze and Rank: Rank candidates based on the following criteria, prioritizing those with the best aggregate scores:
- High On-Target Efficiency Score: As predicted by the software's algorithm (e.g., Doench '16 score).
- Low Off-Target Score: Favor guides with high specificity scores (e.g., CCTop, CFD scores). Manually inspect the top 5-10 predicted off-target sites for each candidate; avoid guides with off-targets in protein-coding regions [46] [44].
- Optimal GC Content: Select guides with 40-60% GC content. Guides with GC content that is too low may be unstable, while those that are too high may have increased off-target binding [44].
- Minimize Repetitive Sequences: Exclude guides with homopolymeric runs (e.g., AAAA) or simple repeats.
- Select Multiple Guides: Choose 3-5 top-ranked gRNAs for empirical testing, as in silico predictions do not always correlate with cellular performance.
gRNA Chemical Modifications
For in vivo applications, synthetic gRNAs with chemical modifications enhance stability and specificity.
- Common Modifications:
- 2'-O-methyl analogs (2'-O-Me): Added to the 3' and 5' ends to increase nuclease resistance.
- 3' phosphorothioate bonds (PS): Linkages between nucleotides in the terminal bases to reduce degradation.
- Impact: These modifications not only increase gRNA half-life and on-target editing efficiency but also significantly reduce off-target editing [44].
Table 2: Key Considerations for gRNA Design
| Design Factor | Recommendation | Rationale |
|---|---|---|
| gRNA Length | 18-20 nucleotides | Shorter guides have lower risk of off-target activity while often maintaining high on-target efficiency [44]. |
| GC Content | 40-60% | Stabilizes the DNA:RNA duplex at the on-target site, improving efficiency and specificity. Extreme GC increases off-target risk [44]. |
| Off-Target Prediction | Select gRNAs with no or few predicted off-targets, especially in exons | Computational prediction is the first line of defense against off-target effects [46] [44]. |
| Chemical Modifications | Incorporate 2'-O-Me and PS bonds for synthetic guides | Increases resistance to nucleases, improves efficacy, and reduces off-target editing in therapeutic contexts [44]. |
Delivery Considerations and Cargo Format
The delivery vehicle and the form of the CRISPR cargo directly influence the kinetics and duration of editing activity, which is a critical factor for off-target effects.
Cargo Format Comparison
The CRISPR machinery can be delivered as DNA, mRNA, or protein (RNP), each with different implications for specificity.
Table 3: Impact of CRISPR Cargo Format on Specificity
| Cargo Format | Mechanism | Impact on Off-Target Effects | Compatible Delivery Methods |
|---|---|---|---|
| DNA Plasmid | Requires transcription and translation within the cell. | Highest Risk: Leads to prolonged Cas9 expression, increasing the window for off-target activity [1] [44]. | Viral vectors (LV, AdV), some non-viral methods. |
| mRNA | Requires only translation within the cell. | Medium Risk: More transient activity than DNA, but still allows for a burst of protein production [1]. | LNPs, electroporation. |
| Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and gRNA. | Lowest Risk: Immediate activity and rapid degradation; offers the most transient exposure, drastically reducing off-target effects [1] [44]. | Electroporation (ex vivo), some LNPs. |
Protocol: RNP Delivery for Ex Vivo Editing
This protocol utilizes RNP complexes for high-specificity editing in cell cultures.
Materials:
- Purified High-Fidelity Cas9 Protein: Commercially available or purified in-house.
- Chemically Modified Synthetic gRNA: Designed per Section 3 protocols.
- Electroporation System (e.g., Neon, Amaxa).
- Appropriate Cell Culture Media.
Procedure:
- RNP Complex Formation:
- In a nuclease-free tube, combine purified Cas9 protein and synthetic gRNA at a molar ratio of 1:1.2 to 1:1.5 (e.g., 5 µg Cas9 with ~100 pmol gRNA).
- Incubate at room temperature for 10-20 minutes to allow RNP complex assembly.
- Cell Preparation:
- Harvest and wash the target cells (e.g., HEK293, primary T-cells).
- Resuspend cells in an electroporation-compatible buffer at a high concentration (e.g., 1-10 x 10^7 cells/mL).
- Electroporation:
- Mix the cell suspension with the pre-formed RNP complexes.
- Immediately electroporate using a pre-optimized program for your cell type.
- Post-Transfection Handling:
- Transfer cells quickly to pre-warmed culture media.
- Assay editing efficiency and cell viability after 48-72 hours.
Off-Target Detection and Analysis
After editing, it is critical to assess off-target activity, especially for therapeutic development.
Detection Methodologies
A range of methods exists, from targeted to genome-wide.
- Candidate Site Sequencing: The most common method. PCR-amplify and sequence the top ~10-20 in silico predicted off-target sites from your gRNA design tool. This is cost-effective but can miss unpredicted sites [44].
- Targeted Sequencing Methods (Higher Sensitivity):
- GUIDE-seq: Integrates a double-stranded oligodeoxynucleotide tag into double-strand break sites, which is then sequenced to reveal off-target locations genome-wide [46].
- CIRCLE-seq: A cell-free method that uses circularized genomic DNA incubated with Cas9 RNP to identify off-target cleavage sites in vitro with high sensitivity [46] [44].
- Whole Genome Sequencing (WGS): The most comprehensive method. Sequence the entire genome of edited clones to identify all variants. It is the gold standard but is expensive and requires sophisticated bioinformatics to distinguish true off-targets from background noise [46] [44].
The Scientist's Toolkit
Table 4: Essential Research Reagents and Resources
| Item | Function/Description | Example Tools/Suppliers |
|---|---|---|
| gRNA Design Software | Computational nomination of high-specificity gRNAs with off-target predictions. | CRISPOR, ChopChop, Synthego Guide Design [44]. |
| High-Fidelity Cas Nuclease | Engineered Cas protein with reduced off-target cleavage. | OpenCRISPR-1, eSpCas9(1.1), SpCas9-HF1, hfCas12Max [1] [45] [44]. |
| Chemically Modified gRNA | Synthetic gRNA with modifications to improve stability and reduce off-target effects. | Synthego (2'-O-Me, PS modifications) [44]. |
| Off-Target Detection Kits | Wet-bench kits for identifying off-target sites experimentally. | GUIDE-seq, CIRCLE-seq, DISCOVER-seq kits [46] [44]. |
| Analysis Software | Tool for analyzing sequencing data to determine editing efficiency and identify indels. | ICE (Inference of CRISPR Edits) for Sanger data; NGS analysis pipelines [44]. |
The safe and efficient delivery of CRISPR-Cas genome editing machinery represents one of the most significant bottlenecks in therapeutic applications. A primary constraint stems from the limited packaging capacity of delivery vectors, particularly adeno-associated viruses (AAVs), which have a payload limit of approximately 4.7 kilobases (kb) [1]. The conventionally used Streptococcus pyogenes Cas9 (SpCas9) is ~4.2 kb in DNA form, already approaching the AAV capacity limit before including essential components like guide RNA sequences and regulatory elements [1]. This review details two innovative strategies—compact Cas protein utilization and dual-vector delivery systems—that effectively circumvent this barrier, enabling broader therapeutic application of CRISPR technologies.
Compact Cas Proteins: Overcoming Size Restrictions
The Size Advantage of Miniature Cas Variants
Recent discovery and engineering of compact Cas proteins from diverse bacterial and archaeal species provide a direct solution to cargo limitations. These proteins offer a substantial reduction in amino acid length while maintaining full genome-editing functionality, making them ideal candidates for single-vector delivery.
Table 1: Comparison of Cas Protein Sizes and Key Characteristics
| Cas Protein | Size (Amino Acids) | Size (DNA, kb approximate) | Key Advantages | Reported Editing Efficiency |
|---|---|---|---|---|
| SpCas9 (Standard) | 1,368 [1] | ~4.2 [1] | Well-characterized, high efficiency | Baseline |
| Cas12f (Un1Cas12f1) | 529 [47] | ~1.6 | Extremely compact, enables single-AAV delivery | Suboptimal in native form [47] |
| hfCas12Max | 1,080 [1] | ~3.3 | Engineered for enhanced editing fidelity | High editing efficiency [1] |
| Cas12k | 639 [48] | ~1.9 | Compact size with editing capability | Varies by target |
| Cas12m | 596 [48] | ~1.8 | Compact size with editing capability | Varies by target |
The enhanced cellular uptake of compact Cas proteins has been experimentally validated. A 2025 comparative study demonstrated that the Cas12f protein (552 Da) showed significantly enhanced cellular penetration compared to the larger Cas9 (~1.4 kDa) when delivered using efficient delivery vectors in human cells [48]. This improved uptake efficiency directly addresses critical challenges in clinical application where delivery efficiency is paramount.
Engineering Enhancements for Compact Cas Systems
While naturally compact, many miniature Cas proteins initially exhibited suboptimal editing efficiency compared to their larger counterparts. Recent protein and guide RNA engineering efforts have substantially improved their performance:
Engineered Circular Guide RNAs (cgRNAs): Research demonstrates that engineering circular guide RNAs for Cas12f significantly improves system stability and efficiency. These cgRNAs feature covalently closed loop structures that offer enhanced protection against exonuclease degradation [47]. In experimental models, this innovation resulted in a 1.9 to 19.2-fold improvement in gene activation efficiency compared to conventional linear guide RNAs [47].
Phase Separation Systems: Further enhancement of the Cas12f/cgRNA system has been achieved by incorporating liquid-liquid phase separation domains. Fusion of the intrinsically disordered region (IDR) of FUS protein with dCas12f-VPR created dynamic compartmentalization organelles that further increased activation efficiency approximately 2.3 to 3.9-fold in experimental models [47].
The following diagram illustrates the structural and functional enhancements in engineered compact Cas systems:
Dual-Vector Systems: Delivering Large Payloads
Dual-Vector Strategies and Mechanisms
When compact Cas proteins are unsuitable for a specific application or when larger editing systems are required, dual-vector approaches provide an effective alternative. These systems employ two separate AAV vectors to co-deliver split components of the CRISPR machinery that reassemble inside target cells. The three primary mechanisms for dual-vector reconstitution include:
DNA Trans-Splicing: Relies on homologous recombination and concatemerization of co-infecting AAV genomes. While this was the first dual-vector approach applied in vivo, it often results in low to moderate reconstitution efficiency [49].
Protein Trans-Splicing (Split Inteins): Utilizes naturally occurring intein domains that mediate protein splicing and reconstitution. This approach typically achieves higher reconstitution efficiencies but requires specific amino acids at the split site and produces potentially immunogenic intein fragments, raising safety concerns for clinical applications [49].
mRNA Trans-Splicing (REVeRT): A recently developed technology that enables reconstitution at the mRNA level through trans-splicing of two separate transcripts. This method offers greater flexibility in split site selection and does not produce foreign protein elements, making it potentially safer for therapeutic use [49].
Quantitative Performance of Dual-Vector Systems
Table 2: Comparison of Dual-Vector System Performance in Experimental Models
| System Type | Application | Reconstitution Efficiency | Key Findings | Reference |
|---|---|---|---|---|
| Dual AAV8 (SaCas9) | OTC deficiency correction in mice | 10% (6.7-20.1%) of hepatocytes corrected | Increased survival on high-protein diet; 31% of alleles showed indels | [50] |
| REVeRT (mRNA trans-splicing) | Fluorophore reconstitution in vitro | 44-53.5% of transfected cells | Flexible split site selection; seamless ligation | [49] |
| REVeRT (mRNA trans-splicing) | Retinal delivery in mouse models | Robust specific fluorophore expression | Successful reconstitution in retinal cells | [49] |
| Dual AAV (DNA trans-splicing) | Various in vivo applications | Low to moderate | Limited by homologous recombination efficiency | [49] |
The following diagram illustrates the workflow and comparative efficiency of the three dual-vector approaches:
Application Notes and Protocols
Protocol: Dual AAV-Mediated Gene Correction in Mouse Liver
This protocol outlines the methodology for in vivo gene correction using dual AAV8 vectors based on the successful treatment of ornithine transcarbamylase (OTC) deficiency in newborn mice [50].
Materials and Reagents
- AAV8.SaCas9 vector (expressing Staphylococcus aureus Cas9 from liver-specific TBG promoter)
- AAV8.sgRNA1.donor vector (containing U6-driven sgRNA and 1.8 kb donor DNA sequence)
- Newborn spfash mice (postnatal day 2)
- High-protein diet challenge materials
- Deep sequencing platform for analysis
- SURVEYOR assay reagents for indel detection
Procedure
- Vector Preparation: Prepare AAV8.SaCas9 and AAV8.sgRNA1.donor vectors at appropriate titers. For the OTC study, a 1:10 ratio (5×10¹⁰ GC SaCas9 : 5×10¹¹ GC sgRNA.donor) was optimal [50].
Neonatal Injection: Intravenously infuse the AAV mixture into postnatal day 2 spfash pups. The neonatal timing is critical as it leverages hepatocyte proliferation to promote editing and vector genome dilution.
Efficiency Analysis (3-8 weeks post-injection):
- Deep Sequencing: Amplify and sequence the targeted OTC region to quantify HDR efficiency and indel formation.
- Immunohistochemistry: Assess OTC protein expression in liver sections.
- Functional Assay: Evaluate survival and ammonia levels in response to high-protein diet challenge.
Off-Target Assessment: Analyze top predicted off-target sites (e.g., 49 potential sites identified for sgRNA1 in the OTC study) using targeted amplification and deep sequencing.
Key Considerations
- Monitor SaCas9 persistence: Western blot analysis typically shows high SaCas9 at 1 week declining to undetectable by 8 weeks [50].
- Assess liver enzyme activity and mRNA expression to confirm functional correction.
- The sparse fur ash (spfash) mouse model has a G-to-A point mutation creating a splice site defect, with animals exhibiting 5% residual OTC activity and susceptibility to high-protein diet-induced hyperammonemia [50].
Protocol: Screening Gene Editing Outcomes via eGFP to BFP Conversion
This protocol provides a rapid, scalable method to quantify CRISPR editing outcomes using a fluorescent reporter system [16].
Materials and Reagents
- eGFP-positive cell lines (generated via lentiviral transduction)
- CRISPR-Cas9 editing reagents (RNP, mRNA, or plasmid)
- BFP repair template (for HDR)
- Flow cytometer with appropriate laser/filter configuration
- Cell culture reagents and transfection materials
Procedure
- Cell Preparation: Generate eGFP-positive cells through lentiviral transduction and ensure robust, stable expression.
Transfection: Deliver CRISPR-Cas9 reagents targeting the eGFP sequence along with BFP repair template (for HDR assessment).
Incubation and Analysis: Allow 72-96 hours for editing and protein turnover, then analyze by flow cytometry.
Data Interpretation:
- eGFP-negative/BFP-negative cells: Indicate NHEJ-mediated knockout.
- eGFP-negative/BFP-positive cells: Successful HDR-mediated conversion.
- eGFP-positive cells: Unsuccessful editing.
Applications
- Optimizing delivery methods: Compare transfection/transduction efficiency.
- Testing novel editors: Evaluate efficiency of new Cas variants or engineered systems.
- Screening gRNAs: Identify most effective guide sequences for a target.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Compact CRISPR Delivery Systems
| Reagent/Category | Specific Examples | Function and Application | Considerations |
|---|---|---|---|
| Compact Cas Proteins | Cas12f, Cas12k, Cas12m, hfCas12Max | Genome editing in size-constrained environments; Cas12f (529 aa) enables single-AAV delivery with additional space for regulatory elements [48] [47] | Editing efficiency may require enhancement; specificity varies |
| Engineered Guide RNAs | Circular gRNAs (cgRNAs) | Enhanced stability and persistence; demonstrated 1.9-19.2-fold improvement in activation with Cas12f systems [47] | Requires specialized expression systems; optimization needed for different Cas proteins |
| Delivery Vectors | AAV8, AAV8(Y733F), Lipid Nanoparticles (LNPs) | AAV: High liver tropism; LNPs: Suitable for repeated administration as they avoid viral vector immunity [50] [5] | AAV immunogenicity; LNP tissue targeting limitations |
| Dual-Vector Systems | REVeRT (mRNA trans-splicing), Split Intein, DNA Trans-Splicing | Delivery of large cargo; REVeRT offers flexibility in split site selection and efficient reconstitution [49] | Reconstitution efficiency varies; potential immunogenicity with intein systems |
| Analytical Tools | Deep Sequencing, SURVEYOR Assay, Flow Cytometry (eGFP/BFP conversion) | Quantifying editing efficiency and off-target effects; fluorescent reporter systems enable rapid screening [50] [16] | Sensitivity limitations; cost considerations for large-scale sequencing |
The complementary strategies of compact Cas protein utilization and dual-vector delivery systems have significantly advanced the field of CRISPR-based therapeutics by overcoming fundamental cargo limitations. Compact Cas proteins like Cas12f provide a direct solution through their minimal size requirements, while engineering enhancements such as circular guide RNAs and phase separation domains have addressed initial efficiency concerns. Meanwhile, dual-vector approaches, particularly mRNA trans-splicing systems, offer a versatile platform for delivering larger CRISPR payloads with improving efficiency and safety profiles. As these technologies continue to mature, they pave the way for treating a broader range of genetic disorders through precise genome editing, moving the field closer to realizing the full therapeutic potential of CRISPR-based medicine.
{# The Challenge of Endosomal Escape in CRISPR-Cas9 Delivery}
The Endosomal Bottleneck in Non-Viral Delivery
The journey of a non-viral CRISPR-Cas9 delivery vector from the extracellular space to its site of action in the nucleus is fraught with obstacles. A primary barrier is entrapment within the endo-lysosomal pathway. After cellular internalization via endocytosis, delivery vehicles are trafficked through endosomes, which mature into late endosomes and ultimately fuse with lysosomes. Within these compartments, the acidic environment and abundant digestive enzymes (e.g., nucleases and proteases) can degrade the precious CRISPR cargo before it ever reaches the cytosol [51] [52]. It is estimated that a mere 1–2% of internalized nucleic acids successfully escape this pathway, making endosomal escape a critical limiting factor for editing efficiency [52]. Overcoming this barrier is therefore not merely an optimization step but a fundamental requirement for effective non-viral CRISPR-Cas9 gene therapy.
Quantitative Data on Endosomal Escape Strategies
The field has developed diverse strategies to enhance endosomal escape, each with distinct mechanisms and performance metrics. The data below summarizes key approaches and their reported efficacy.
Table 1: Performance Metrics of Lipid-Based and Polymeric Escape Strategies
| Strategy Category | Specific Example / Mechanism | Reported Escape / Editing Efficiency | Key Advantages |
|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Ionizable lipids (e.g., DODMA, DLin-MC3-DMA) that become cationic in acidic endosomes [52]. | Varies with composition; considered a major bottleneck with ~1-2% escape efficiency for nucleic acids [52]. | Clinically advanced; biodegradable variants reduce long-term toxicity [52]. |
| Polymeric Nanoparticles | Polymers with protonable amines (e.g., PBAEs) that cause endosomal swelling and rupture via the "proton sponge" effect [53]. | Highly variable and dependent on polymer structure; lack of standardized quantification methods [53]. | Highly tunable chemical properties; can be engineered for stimuli-responsive behavior [51] [53]. |
| Stimuli-Responsive Systems | Systems designed to respond to low pH (acid-labile linkers) or high redox potential (GSH-sensitive bonds) in the endosome [51]. | Facilitates controlled, targeted release; minimizes off-target editing [51]. | Provides spatiotemporal control, enhancing safety and specificity [51]. |
| Fusogenic Lipids / Peptides | Incorporation of dioleoylphosphatidylethanolamine (DOPE) or synthetic fusogenic peptides that promote membrane fusion [52]. | Enhances escape by fusing the delivery vehicle membrane with the endosomal membrane [52]. | Mimics viral escape mechanisms; can be co-formulated with other nanocarriers. |
Table 2: Physical and Biological Methods for Intracellular Delivery
| Strategy Category | Method | Typical Application | Key Advantages & Disadvantages |
|---|---|---|---|
| Physical Methods | Electroporation / Nucleofection | Ex vivo delivery to hematopoietic stem cells (HSCs) and immune cells [8] [54]. | Advantage: High efficiency for ex vivo work (e.g., ~90% indels in HSCs for CASGEVY) [8].Disadvantage: Can compromise cell viability; not suitable for in vivo systemic delivery [54]. |
| Biological Vesicles | Extracellular Vesicles (EVs) | Delivery of Cas9 RNP via engineered EVs with aptamer-based loading [7]. | Advantage: Innate biocompatibility and low immunogenicity; natural membrane fusion capabilities [7] [55].Disadvantage: Complex manufacturing and loading heterogeneity [7] [1]. |
Experimental Protocols for Key Strategies
Protocol 1: Formulating Endosomolytic Lipid Nanoparticles (LNPs) for RNP Delivery
This protocol details the microfluidic formulation of LNPs encapsulating Cas9 ribonucleoprotein (RNP) for enhanced endosomal escape [52].
1. Reagent Preparation:
- Lipids: Prepare ethanolic solutions of the following lipids at specified molar ratios:
- Ionizable Lipid (e.g., DLin-MC3-DMA): 50 mol%
- Helper Lipid (e.g., DOPE): 10 mol% (Note: DOPE promotes fusogenic behavior)
- Cholesterol: 38.5 mol% (stabilizes LNP structure)
- PEGylated Lipid (e.g., DMG-PEG2000): 1.5 mol% (controls nanoparticle size and stability)
- Aqueous Phase: Prepare the Cas9 RNP complex by incubating purified Cas9 protein with synthetic sgRNA in a suitable buffer (e.g., sodium acetate, pH 4.0). The acidic pH is crucial for subsequent encapsulation.
2. Microfluidic Mixing:
- Use a microfluidic device (e.g., NanoAssemblr) for rapid and reproducible LNP formation.
- Set the flow rate ratio (aqueous:organic) to 3:1 to ensure efficient mixing.
- Combine the aqueous RNP solution and the ethanolic lipid solution in the mixing chamber. The change in pH and polarity during mixing drives the self-assembly of lipids around the RNP cargo.
3. Buffer Exchange and Characterization:
- Dialyze or use tangential flow filtration (TFF) against a neutral pH buffer (e.g., 1X PBS) to remove ethanol and adjust the final pH.
- Characterize the final LNPs for:
- Size and Polydispersity (PDI): via Dynamic Light Scattering (DLS). Target size: < 150 nm.
- Encapsulation Efficiency (EE): Quantify using Ribogreen assay post-dialysis. Target EE: > 80%.
- Zeta Potential: via DLS. A near-neutral charge is desirable for in vivo applications.
Protocol 2: Aptamer-Based Loading of Cas9 RNP into Extracellular Vesicles (EVs)
This protocol describes a modular strategy for loading Cas9 RNP into EVs using MS2 aptamer-based capture and a UV-cleavable linker for controlled release [7].
1. Plasmid Construction and Cell Transfection:
- Construct a plasmid expressing a fusion protein of tandem MS2 coat protein (MCP), a UV-photocleavable linker (PhoCl), and the EV-enriched tetraspanin CD63 (MCP-PhoCl-CD63).
- Design a second plasmid expressing the sgRNA with MS2 aptamer sequences incorporated into its tetraloop and stemloop 2.
- Co-transfect HEK293T cells (or another EV-producing cell line) with three plasmids: the MCP-PhoCl-CD63 construct, the MS2-sgRNA construct, and a Cas9 expression plasmid (or variant, e.g., base editor ABE8e).
2. EV Biogenesis and Harvesting:
- Incubate transfected cells for 48-72 hours in EV-depleted media to allow for EV biogenesis and cargo loading. The intraluminal MCP binds to the MS2 aptamers on the Cas9 RNP, loading it into nascent EVs.
- Collect the conditioned media and remove cells and debris via sequential centrifugation (e.g., 300 × g for 10 min, then 2,000 × g for 20 min).
3. EV Purification and UV Activation:
- Concentrate and purify EVs from the supernatant using Tangential Flow Filtration (TFF) followed by Size Exclusion Chromatography (SEC).
- Characterize EV preparation via Nanoparticle Tracking Analysis (NTA) for size/concentration and Western Blot for EV markers (CD63, ALIX, TSG101).
- UV Activation: To release the Cas9 RNP from the EV membrane upon internalization into target cells, expose the purified EV preparation to 365 nm UV light for a defined duration (e.g., 10-15 minutes). This cleaves the PhoCl linker, freeing the RNP in the endosomal lumen to facilitate its escape and nuclear entry.
Protocol 3: Quantifying Endosomal Escape Efficiency
A critical and often overlooked step is the direct measurement of escape efficiency. This protocol outlines a quantitative imaging-based method [53].
1. Fluorescent Labeling:
- Label the CRISPR cargo (e.g., Cas9 RNP) with a pH-insensitive fluorophore (e.g., Alexa Fluor 647).
- Co-label endo-lysosomal compartments by incubating cells with a fluorescent dye that marks these organelles (e.g., LysoTracker Green).
2. Live-Cell Imaging and Analysis:
- Treat cells with the labeled delivery vehicle and perform live-cell confocal microscopy over a time course (e.g., 0-8 hours post-transfection).
- Acquire z-stack images to capture entire cell volumes.
- Use image analysis software (e.g., ImageJ, Volocity) to perform colocalization analysis.
- The Manders' Colocalization Coefficient (MCC) or Pearson's Correlation Coefficient (PCC) can be calculated between the cargo signal (red) and the endo-lysosomal signal (green).
- A decrease in the colocalization coefficient over time indicates successful endosomal escape, as the cargo is no longer confined to the labeled compartments.
- The escape efficiency can be quantified as the percentage of cells showing a significant decrease in colocalization by a specific time point.
Visualizing the Pathways and Workflows
Cellular Journey of a Non-Viral CRISPR Vector
This diagram illustrates the intracellular trafficking pathway of a non-viral CRISPR delivery vector, highlighting the critical endosomal escape step.
Mechanisms of Endosomal Escape
This diagram outlines the primary physicochemical mechanisms used by non-viral vectors to achieve endosomal escape.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Endosomal Escape
| Reagent / Material | Function / Role in Research | Example Use Case |
|---|---|---|
| Ionizable Cationic Lipids | Core component of LNPs; protonates in acidic endosomes, destabilizing the endosomal membrane. | DLin-MC3-DMA, SM-102; used in LNP formulation for mRNA/RNP delivery [52]. |
| Fusogenic Helper Lipids | Promotes transition to inverted hexagonal phase, enhancing membrane fusion and content release. | DOPE (1,2-dioleoyl-sn-glycero-3-phosphoethanolamine) is a common additive to LNP formulations [52]. |
| Cationic Polymers | Induces the "proton sponge" effect; buffers endosomal pH, leading to osmotic swelling and rupture. | Polyethylenimine (PEI), PBAEs; used in polymeric nanoparticle formation [53]. |
| Photocleavable Linkers | Enables spatiotemporally controlled cargo release inside cells via external light trigger. | PhoCl; used in EV strategies to uncouple Cas9 RNP from the vesicle membrane upon UV exposure [7]. |
| Fluorescent Dyes for Tracking | Allows visualization and quantification of cargo localization and escape efficiency via microscopy. | LysoTracker (for endo-lysosomes), pHrodo (for pH sensing), Alexa Fluor dyes (for cargo labeling) [53]. |
| MS2-MCP Aptamer System | Provides a high-affinity, modular platform for loading RNA or RNP complexes into delivery vehicles. | Used to load MS2-aptamer-modified sgRNA/Cas9 RNP into EVs engineered with MCP fusion proteins [7]. |
The therapeutic application of CRISPR-Cas9 technology hinges on the efficient and specific delivery of editing components to target cells. While the CRISPR system itself offers unparalleled precision in genome targeting, achieving cell-type specificity in delivery remains a paramount challenge for research and drug development [1]. Lipid Nanoparticles (LNPs) have emerged as a leading non-viral delivery platform, acclaimed for their safety profile and modularity, which permits tailoring for organ-selective targeting [1] [5]. The natural tropism of systemically administered LNPs tends toward the liver; however, recent advances in LNP biochemistry and screening methodologies have enabled the rational design of formulations with enhanced specificity for other tissues, including the spleen and its resident T cells [5] [56]. This Application Note details the principles, experimental data, and protocols for developing and utilizing tissue-specific LNPs for targeted CRISPR-Cas9 delivery in biomedical research.
Principles and Advances in Tissue-Specific LNP Delivery
The modular composition of LNPs, typically consisting of an ionizable lipid, helper lipid(s), cholesterol, and a PEG-lipid, provides a chemical toolkit for tuning their biological fate [56]. The foundational principle of tissue-specific LNP design, such as Selective Organ Targeting (SORT), involves incorporating supplementary SORT molecules into the standard LNP structure. These molecules alter the LNP's surface properties and subsequent interactions with biological systems, enabling targeted delivery to tissues beyond the liver, such as the lungs and spleen [1].
A landmark 2025 study demonstrated the feasibility of this approach by identifying a spleen-tropic LNP formulation through a multi-step screening platform. This formulation preferentially targeted splenic T cells in vivo and enabled efficient gene editing via the delivery of CRISPR-Cas9 Ribonucleoprotein (RNP) complexes [56]. The success of this platform underscores two critical trends in the field: the advantages of RNP cargo and the power of systematic screening.
RNP Cargo for Therapeutic Editing: The delivery of pre-assembled Cas9-gRNA RNP complexes offers significant benefits over DNA or mRNA cargoes. RNPs mediate immediate genome editing upon cytosolic delivery, bypassing the need for transcription or translation. This leads to a shorter cellular residence time, which minimizes off-target effects and reduces potential immunogenicity, enhancing both the precision and safety profile of the intervention [1] [56].
Table 1: Key Advantages of RNP Delivery for CRISPR-Cas9 Editing
| Feature | Benefit for Research and Therapy |
|---|---|
| Immediate Activity | Faster editing kinetics; does not rely on endogenous translation machinery [56]. |
| Short Persistence | Reduced off-target effects due to transient activity [1] [56]. |
| Pre-assembled Complex | Consistent and predictable editing efficiency; avoids immune responses to exogenous mRNA [56]. |
Quantitative Data and Design Principles from a Spleen-Tropic LNP Study
A high-throughput screening of 486 unique LNP formulations, systematically varying in helper lipid composition, was conducted to identify candidates optimal for RNP delivery. The screening used HEK Ai9 reporter cells, where successful editing via Cre recombinase RNP delivery activates tdTomato fluorescence, quantified by flow cytometry [56].
Table 2: Top-Performing Helper Lipids for RNP Delivery Identified by In Vitro Screening
| Helper Lipid | Abbreviation | Key Property | Relative Editing Efficiency |
|---|---|---|---|
| Dioleoyl-3-trimethylammonium propane | DOTAP | Cationic | High (~14.3% tdTomato+ cells) |
| Dimethyldioctadecylammonium | DDAB | Cationic | High |
| 1-stearoyl-2-oleoyl-sn-glycero-3-phospho-(1'-rac-glycerol) | 18PG | Anionic, unsaturated acyl chains | Moderate |
| 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine | DOPE | Zwitterionic | Low/Minimal |
| 1,2-distearoyl-sn-glycero-3-phosphocholine | DSPC | Zwitterionic | Low/Minimal |
The most potent formulation from this library achieved an editing efficiency of 14.3% ± 8% in vitro, which was more than double the efficiency of a commercial benchmark reagent (CRISPR-Max, ~6%) at the same RNP dose [56].
Subsequent in vivo screening in Ai9 mice revealed that the top-performing LNP formulation from the in vitro assay exhibited spleen-tropic behavior. This formulation demonstrated a clear preference for gene editing in splenic T cells over other cell types in the spleen, such as B cells and macrophages [56].
A machine learning analysis of the high-throughput screening data yielded key design principles for LNP-based protein delivery, quantified using SHAP (Shapley Additive exPlanations) values [56]:
- Lipid Composition: Formulations with a combined percentage of ionizable and helper lipids between 50% and 80% showed improved efficiency.
- Lipid Saturation: Helper lipids with unsaturated tails (e.g., higher number of double bonds) were preferred, as their increased fluidity promotes endosomal escape.
- Surface Charge: Cationic helper lipids (DOTAP, DDAB) generally outperformed anionic and zwitterionic lipids, suggesting a role for charge in complexing with negatively charged RNPs and facilitating cellular uptake.
- Lipid-to-Protein Ratio: A lower ratio was associated with higher editing efficiency, indicating that excessive lipid content may hinder RNP release.
Experimental Protocol: In Vivo Gene Editing of Splenic T Cells
This protocol details the methodology for achieving functional gene knockout in murine splenic T cells using the optimized, spleen-tropic LNP formulation to deliver CRISPR-Cas9 RNPs [56].
Research Reagent Solutions
Table 3: Essential Materials for LNP-RNP In Vivo Editing
| Item | Function/Description | Example/Note |
|---|---|---|
| Ionizable Lipid | Core structural component of LNP; enables encapsulation and endosomal escape. | DLin-MC3-DMA |
| Helper Lipids | Modulate LNP structure, stability, and targeting. Critical for specificity. | DOTAP, DDAB, 18PG |
| Cholesterol | Enhances LNP stability and membrane integrity. | Pharmaceutical grade |
| PEG-Lipid | Shields LNP surface, controls particle size and pharmacokinetics. | DMG-PEG-2000 |
| Cas9 Protein | The nuclease component of the RNP complex. | High-purity, endotoxin-free |
| sgRNA | Target-specific guide RNA for the RNP complex. | Chemically modified for stability |
| Ai9 Reporter Mice | In vivo model for screening and quantifying editing efficiency. | Allows tdTomato activation upon successful Cre RNP editing |
Step-by-Step Methodology
Part A: Preparation of RNP-Loaded LNPs This process uses microfluidic mixing for precise LNP formation.
- Prepare the Aqueous Phase: Dissolve the pre-complexed Cas9-sgRNA RNP (e.g., targeting CCR5 or PD-1) in a sodium acetate buffer (pH 4.0). The final RNP concentration should be tailored to the desired in vivo dosing.
- Prepare the Organic Phase: Combine the lipid mixture in ethanol. The optimized spleen-tropic formulation from the cited study includes:
- Ionizable Lipid: DLin-MC3-DMA
- Helper Lipid: Cationic lipid (e.g., DOTAP or DDAB)
- Structural Lipids: Cholesterol, DMG-PEG-2000
- Critical Note: The specific molar ratios are proprietary and central to the technology. Researchers should systematically optimize these ratios based on the design principles in Section 3.
- Microfluidic Mixing: Use a microfluidic device (e.g., NanoAssemblr) to mix the aqueous and organic phases at a controlled flow rate and ratio (e.g., 3:1 aqueous-to-organic ratio) to form stable LNPs.
- Buffer Exchange and Purification: Dialyze the freshly formed LNP suspension against a large volume of PBS (pH 7.4) for several hours at 4°C to remove residual ethanol and adjust the pH. Subsequently, concentrate the LNPs using centrifugal filters if necessary.
- Quality Control: Characterize the LNPs for:
- Size and Polydispersity (PDI): Use Dynamic Light Scattering (DLS). Target a size of ~80-100 nm with PDI < 0.2.
- Encapsulation Efficiency (EE): Quantify using an RNP-specific assay (e.g., Ribogreen assay).
- Sterility: Ensure formulations are sterile-filtered (0.22 µm) before in vivo administration.
Part B: In Vivo Administration and Analysis All animal procedures must be approved by the relevant Institutional Animal Care and Use Committee (IACUC).
- Animal Model: Use 6-8 week old Ai9 reporter mice for screening or C57BL/6 mice for therapeutic knockouts (e.g., CCR5, PD-1).
- LNP Dosing: Administer the formulated RNP-LNPs intravenously via the tail vein. A typical dose may range from 0.5 to 5 mg/kg of RNP.
- Tissue Harvest and Analysis: Euthanize mice at the desired endpoint (e.g., 3-7 days post-injection).
- Harvest Spleens: Process spleens into a single-cell suspension.
- Isolate T Cells: Enrich for T cells using a commercial isolation kit or by magnetic-activated cell sorting (MACS).
- Assess Editing Efficiency:
- Flow Cytometry: For Ai9 mice, analyze the percentage of tdTomato+ cells in the T cell population (CD3+).
- Next-Generation Sequencing (NGS): For therapeutic targets, perform T7 Endonuclease I assay or deep sequencing of the genomic region surrounding the sgRNA target site to quantify indel frequency.
Diagram 1: Workflow for Spleen-Tropic LNP-Mediated In Vivo Gene Editing.
Application in Disease Models
The functional utility of this platform was validated in two distinct disease models [56]:
- HIV Resistance Model: LNPs encapsulating RNPs targeting the CCR5 co-receptor achieved efficient knockout in splenic T cells. This strategy aims to create a population of HIV-resistant T cells, mimicking the protective effect observed in individuals with a natural CCR5 mutation.
- Cancer Immunotherapy Model: In a B16-OVA melanoma model, LNPs delivering RNPs to knock out PD-1 in splenic T cells led to enhanced antitumor efficacy. This in vivo gene editing approach for immune checkpoint blockade (ICB) presents a potential alternative to antibody-based therapies.
The development of tissue-specific LNPs represents a significant leap forward for in vivo CRISPR-Cas9 research and therapy. By moving beyond the liver's natural tropism, these advanced delivery systems open new avenues for targeting genetic diseases, infections, and cancers residing in other tissues. The outlined principles, quantitative data, and detailed protocol provide a foundation for researchers to develop and apply these sophisticated targeting strategies, accelerating the transition from basic research to transformative therapeutics.
The CRISPR-Cas9 system has emerged as a revolutionary technology in genome editing, offering unprecedented potential for treating genetic disorders. However, the clinical application of CRISPR-based therapies, particularly in vivo approaches, faces a significant challenge: immunogenicity. The Cas9 nuclease, derived from bacteria such as Streptococcus pyogenes (SpCas9) and Staphylococcus aureus (SaCas9), is recognized as foreign by the human immune system, potentially triggering both innate and adaptive immune responses [57] [58]. Pre-existing immunity to these bacterial proteins is widespread in the human population, with studies indicating that approximately 78% of healthy individuals possess class-switched immunoglobulin G (IgG) antibodies against SaCas9, and 58% have antibodies against SpCas9 [59]. This immunogenicity poses a dual risk, potentially compromising both the safety and efficacy of CRISPR-based treatments through reduced editing efficiency, accelerated clearance of edited cells, and potential inflammatory toxicities.
Addressing immunogenicity requires a multi-faceted approach that integrates insights from immunology with innovative protein and delivery engineering. This Application Note outlines validated strategies and detailed protocols for mitigating immune responses against CRISPR-Cas9 components, providing researchers with practical tools to enhance the therapeutic potential of their gene editing applications within the broader context of CRISPR-Cas9 delivery methods for cellular research [1] [31].
Strategic Approaches to Mitigate Immunogenicity
Protein Engineering to Evade Immune Recognition
Rational design of Cas9 variants with reduced immunogenicity represents a promising strategy for mitigating immune responses. This approach focuses on modifying immunodominant epitopes while preserving nuclease activity and specificity.
Epitope Identification and Modification
The initial step involves mapping the specific regions (epitopes) within Cas9 proteins that are recognized by the immune system. MHC-associated peptide proteomics (MAPPs) analysis has identified immunodominant epitopes in clinically relevant nucleases. For SaCas9, key epitopes include 8-GLDIGITSV-16, 926-VTVKNLDVI-934, and 1034-ILGNLYEVK-1050. Similarly, for AsCas12a, dominant epitopes include 210-RLITAVPSL-218, 277-LNEVLNLAI-285, and 971-YLSQVIHEI-979 [59].
Computational tools such as NetMHCpan 4.1 enable prediction of peptide-MHC class I binding affinity, guiding the design of modified variants with reduced immunogenicity. Point mutations are introduced into these epitopes to disrupt MHC binding while maintaining structural integrity and catalytic function. For example, SaCas9 triple mutants L9A/I934T/L1035A (SaCas9.Redi.1), L9S/I934K/L1035V (SaCas9.Redi.2), and V16A/I934K/L1035V (SaCas9.Redi.3) demonstrate wild-type levels of nuclease activity with significantly reduced immune recognition [59].
Table 1: Engineered Low-Immunogenicity Cas Variants
| Nuclease | Variant Name | Key Mutations | Editing Efficiency | Immunogenicity Reduction |
|---|---|---|---|---|
| SaCas9 | Redi.1 | L9A, I934T, L1035A | Comparable to WT | Significant reduction in CD8+ T cell response |
| SaCas9 | Redi.2 | L9S, I934K, L1035V | Comparable to WT | Significant reduction in CD8+ T cell response |
| SaCas9 | Redi.3 | V16A, I934K, L1035V | Comparable to WT | Significant reduction in CD8+ T cell response |
| AsCas12a | Redi variants | Multiple triple mutants | Varies by mutant | Reduced CD8+ T cell reactivity |
Experimental Validation of Engineered Variants
Protocol: Evaluation of T-cell Response to Cas9 Variants Using ELISpot
Purpose: To assess CD8+ T cell-mediated immunogenicity of engineered Cas9 variants compared to wild-type nucleases.
Materials:
- Peripheral blood mononuclear cells (PBMCs) from healthy human donors (HLA-A*0201 positive)
- ELISpot plates pre-coated with anti-IFN-γ antibody
- Synthetic peptides corresponding to wild-type and mutant epitopes
- Cell culture medium (RPMI-1640 with 10% FBS)
- Positive control (phytohemagglutinin)
- Detection reagents (biotinylated anti-IFN-γ antibody, streptavidin-ALP)
Procedure:
- Isolate PBMCs from donor blood using density gradient centrifugation.
- Resuspend PBMCs in culture medium at a concentration of 2×10^6 cells/mL.
- Add 100 μL cell suspension (2×10^5 cells) to each well of the ELISpot plate.
- Add peptides to respective wells at a final concentration of 10 μg/mL.
- Include positive control (PHA) and negative control (medium only) wells.
- Incubate plates for 24-48 hours at 37°C in 5% CO₂.
- Develop plates according to manufacturer's instructions.
- Quantify spot-forming units (SFUs) using an automated ELISpot reader.
Interpretation: A significant reduction in SFUs for mutant peptides compared to wild-type indicates successful reduction of immunogenicity [59].
Delivery System Selection and Optimization
The choice of delivery vehicle significantly influences the immunogenic profile of CRISPR-Cas9 components. Different delivery modalities present distinct advantages and challenges concerning immune activation.
Viral Vector Systems
Viral vectors remain efficient for CRISPR delivery but vary in their immunogenic potential.
Adeno-Associated Viruses (AAVs) are widely used for in vivo CRISPR delivery due to their mild immune response profile and non-integration into the host genome. However, their limited payload capacity (~4.7 kb) constrains delivery of larger Cas9 orthologs and requires creative solutions such as dual-vector systems or compact Cas9 variants [1]. Adenoviral Vectors (AdVs) offer larger cargo capacity (up to 36 kb) and non-integrative properties but can stimulate stronger immune responses, potentially causing inflammation and tissue damage [1]. Lentiviral Vectors (LVs) efficiently infect dividing and non-dividing cells but integrate into the host genome, raising safety concerns for therapeutic applications [1].
Table 2: Immunogenicity Profiles of Viral Delivery Systems
| Vector Type | Immunogenicity Concern | Advantages | Strategies to Mitigate Immune Response |
|---|---|---|---|
| Adeno-Associated Virus (AAV) | Low to moderate; pre-existing immunity in some populations | Mild immune response; non-integrating; FDA-approved for some applications | Use of rare serotypes; empty capsid removal; transient immunosuppression |
| Adenovirus (AdV) | High; robust innate and adaptive immune activation | Large cargo capacity; high transduction efficiency | PEGylation; immunosuppressive regimens; tissue-specific promoters |
| Lentivirus (LV) | Moderate; potential for insertional mutagenesis | Stable long-term expression; broad tropism | Integration-deficient designs; tissue-specific promoters |
Non-Viral Delivery Systems
Non-viral delivery methods generally elicit reduced immune responses compared to viral vectors and offer advantages in cargo flexibility and manufacturing.
Lipid Nanoparticles (LNPs) have emerged as promising vehicles for CRISPR component delivery, as demonstrated by their successful application in COVID-19 mRNA vaccines. LNPs effectively encapsulate and protect Cas9 mRNA or ribonucleoprotein (RNP) complexes and can be functionalized for targeted delivery. For instance, Selective Organ Targeting (SORT) nanoparticles can be engineered to specifically target lung, spleen, or liver tissues [1]. A key challenge for LNP-mediated delivery is enhancing endosomal escape to avoid lysosomal degradation and improve editing efficiency [1] [29].
Extracellular Vesicles (EVs) represent a biologically inspired delivery platform with innate low immunogenicity, as they are derived from human cells. EVs naturally facilitate intercellular communication and can be engineered for precise CRISPR-Cas9 delivery. A modular strategy using MS2 coat protein fused to EV-enriched proteins (e.g., CD63) enables efficient loading of Cas9 RNP complexes through interaction with MS2 aptamers incorporated into guide RNAs [7]. This approach, combined with UV-cleavable linkers for controlled cargo release, provides a versatile system for delivering various Cas9 variants with minimal immune activation [7].
Protocol: EV-Mediated Cas9 RNP Delivery Using Aptamer-Based Loading
Purpose: To load and deliver CRISPR-Cas9 ribonucleoprotein complexes via engineered extracellular vesicles.
Materials:
- HEK293T cells
- Plasmids: MCP-CD63 (MS2 coat protein-CD63 fusion), Cas9 expression vector, MS2-sgRNA expression vector
- Transfection reagent
- Tangential Flow Filtration (TFF) system
- Size Exclusion Chromatography (SEC) columns
- UV light source (365 nm)
Procedure:
- EV Production:
- Co-transfect HEK293T cells with MCP-CD63, Cas9, and MS2-sgRNA plasmids.
- Culture for 48 hours to allow EV secretion.
EV Isolation:
- Collect conditioned medium and remove cells/debris by centrifugation.
- Concentrate EVs using Tangential Flow Filtration.
- Purity EVs using Size Exclusion Chromatography.
EV Characterization:
- Analyze size distribution by Nanoparticle Tracking Analysis.
- Confirm EV markers (CD63, ALIX, TSG101) by Western blot.
- Verify Cas9 loading efficiency by Western blot.
Cargo Release and Delivery:
- Expose EVs to UV light (365 nm) to cleave the photocleavable linker.
- Incubate EVs with target cells for 24-48 hours.
- Assess editing efficiency by targeted deep sequencing [7].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Immunogenicity Mitigation Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Low-Immunogenicity Cas Variants | SaCas9.Redi.1, .2, .3; AsCas12a Redi variants | Engineered nucleases with reduced MHC binding epitopes |
| Delivery Vehicles | AAV serotypes (e.g., AAV8, AAV9); LNPs with SORT molecules; Engineered EVs | Packaging and targeted delivery of CRISPR components |
| Immune Assessment Tools | ELISpot kits; MHC tetramers; Cytokine ELISA panels | Quantifying T-cell responses and inflammatory profiles |
| sgRNA Modifications | MS2-aptamer sgRNAs; Chemically modified sgRNAs (Synthego) | Enhanced stability and efficient RNP assembly for EV loading |
| Cell Lines | HLA-A*0201 expressing cells (e.g., MDA-MB-231); Primary human PBMCs | In vitro immunogenicity screening |
| Analytical Tools | NetMHCpan 4.1; NTA for EV characterization; ICE analysis for editing assessment | Computational prediction and experimental validation |
Mitigating the immunogenicity of CRISPR-Cas9 components is essential for realizing the full therapeutic potential of gene editing technologies. This Application Note outlines a comprehensive framework combining protein engineering, delivery system optimization, and immune-compatible cargo formulations to address this challenge. The provided protocols and strategic approaches equip researchers with practical methodologies to enhance the safety profile of their CRISPR-based applications, facilitating the transition from basic research to clinical translation.
Data-Driven Decisions: Comparative Analysis and Clinical Validation
The CRISPR-Cas9 system has revolutionized genome editing by enabling precise and efficient genetic modifications across multiple biological systems [8]. Despite its growing therapeutic potential, key challenges remain in mitigating off-target effects, minimizing immunogenicity, and improving the delivery of CRISPR components into target cells [8]. The greatest challenge for therapeutic applications is the safe and efficient delivery of the system to target cells in the human body [2]. This application note provides a integrated analysis of delivery platforms, comparing quantitative efficiency metrics and providing detailed protocols for assessing editing outcomes. We focus on the critical physicochemical parameters that influence therapeutic success, guiding researchers in selecting optimal delivery strategies for their specific experimental needs.
CRISPR-Cas9 Delivery Cargo Formats
Three primary cargo formats exist for delivering CRISPR-Cas9 components into cells, each with distinct advantages and limitations that significantly impact editing efficiency [8] [2].
Plasmid DNA (pDNA) encodes both Cas9 and guide RNA (gRNA) sequences within the same vector. This approach offers simplicity and low-cost manipulation but suffers from the large size of Cas9 and the requirement for nuclear entry, which limits its genome editing efficiency [8]. The necessity for transcription and translation before Cas9 becomes active also delays editing activity.
Messenger RNA (mRNA) for Cas9 coupled with synthetic gRNA offers rapid genome editing with low toxicity, making it ideal for sensitive cells [8]. This system decreases off-target editing events due to transient Cas9 expression and avoids the need for nuclear import of DNA [8]. Liu et al. demonstrated high genome editing efficacy using bioreducible lipid nanoparticles for simultaneous delivery of Cas9 mRNA and gRNA [8].
Ribonucleoprotein (RNP) complexes consisting of preassembled Cas9 protein and gRNA provide the highest gene editing efficiency and specificity [8]. This format minimizes off-target effects and toxicity while enabling immediate genome editing activity without delivery delays [8]. Wei et al. demonstrated that lipid nanoparticles encapsulating RNPs achieved tissue-specific gene editing in murine lungs and liver [8].
Table 1: Comparison of CRISPR-Cas9 Delivery Cargo Formats
| Cargo Format | Editing Efficiency | Specificity | Toxicity | Persistence | Key Applications |
|---|---|---|---|---|---|
| Plasmid DNA | Moderate | Lower | Moderate | Prolonged | Stable cell line generation |
| mRNA + gRNA | High | Moderate | Low | Transient | Primary cell editing |
| RNP Complex | Highest | Highest | Lowest | Immediate, transient | Therapeutic applications |
Delivery Platform Efficiency Metrics
Physical Delivery Methods
Physical methods facilitate plasmid transfer and transportation of mRNA or RNPs with high efficiency, though their application may be limited by cell viability and specificity [8].
Table 2: Efficiency Metrics of Physical Delivery Methods
| Delivery Method | Target Cell/Model | Editing Efficiency | Key Parameters | References |
|---|---|---|---|---|
| Microinjection | HepG2 cells | ~40% | Direct cytoplasmic delivery | [8] |
| Electroporation (mouse zygotes) | Mouse embryos | Highly efficient (no quantitative data) | Electrical parameters optimization | [8] |
| Electroporation (CASGEVY) | Human HSPCs | Up to 90% indels in BCL11A enhancer | Clinical-grade optimization | [8] |
Viral Delivery Systems
Viral vectors vary in their genetic material and transport either DNA or RNA depending on their genomic structure, influencing whether they mediate transient expression or integrate into the host genome [8]. These systems offer high transduction efficiency but pose size constraints and potential immunogenic risks [2].
Non-Viral Delivery Systems
Non-viral systems provide safer alternatives by encapsulating plasmids, mRNA, or pre-formed Cas9:gRNA RNPs [8]. Their efficiency relies on uptake mechanisms and overcoming biological barriers [8]. Since effective encapsulation and delivery depend on electrostatic interactions, the opposite charges on Cas9 (positive) and oligonucleotides or Cas9:gRNA complexes (negative) must be balanced with well-designed carriers [8].
Lipid-based systems use cationic lipids to form stable lipoplexes that enhance payload protection, cellular uptake, and endosomal escape, ultimately improving genome editing efficiency [8]. Chen et al. developed a thermostable Cas9 variant (iGeoCas9) formulated in lipid nanoparticles, achieving efficient nuclease-mediated editing in the liver and lung [8].
Polymeric carriers and hybrid platforms represent emerging approaches that combine advantages of multiple material systems to optimize delivery efficiency while minimizing toxicity [8].
Quantitative Assessment of Editing Efficiency
qEva-CRISPR Method
The qEva-CRISPR method enables quantitative evaluation of CRISPR/Cas9-mediated editing, allowing parallel analysis of target and selected off-target sites [60]. This ligation-based dosage-sensitive method overcomes limitations of traditional assays by detecting all types of mutations, including point mutations and large deletions, with sensitivity that does not depend on the mutation type [60].
Key Advantages:
- Multiplex capability for simultaneous analysis of multiple targets
- Detection of all mutation types (indels, point mutations, large deletions)
- Successful analysis of targets in 'difficult' genomic regions
- Distinguishes between NHEJ and HDR repair outcomes
- Unbiased sgRNA screening for evaluating experimental conditions [60]
Experimental Protocol: qEva-CRISPR Workflow
Day 1: Sample Preparation and DNA Extraction
- Harvest transfected cells 72-96 hours post-transfection
- Extract genomic DNA using standardized kits (e.g., QIAamp DNA Blood Mini Kit)
- Quantify DNA concentration using fluorometric methods
- Normalize samples to 10-20 ng/μL in nuclease-free water
Day 2: Probe Hybridization and Ligation
- Prepare qEva-CRISPR probe mix specific for target and off-target sites
- Denature 100-200 ng genomic DNA at 98°C for 10 minutes
- Hybridize probes by incubating at 60°C for 16-18 hours
- Perform ligation reaction with ligase enzyme at 54°C for 15 minutes
- Inactivate ligase at 98°C for 5 minutes
Day 3: PCR Amplification and Quantification
- Amplify ligation products using universal fluorescent primers
- Perform capillary electrophoresis or next-generation sequencing
- Analyze peak patterns to quantify editing efficiency
- Calculate efficiency using formula: (mutant peak area / total peak area) × 100%
Diagram 1: qEva-CRISPR workflow for quantitative assessment of editing efficiency.
Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR-Cas9 Delivery Studies
| Reagent/Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| CRISPR Plasmids | pSpCas9(BB)-2A-GFP (PX458) | Expresses Cas9 and sgRNA from same vector | Contains GFP marker for transfection efficiency monitoring [60] |
| Lipofection Reagents | Lipofectamine LTX | Forms lipid-DNA complexes for cellular uptake | Optimized for difficult-to-transfect cell lines [60] |
| Electroporation Systems | Neon Transfection System | Electrical pulses create pores in cell membranes | Parameters: 1130-1450V, 10-30ms pulses [60] |
| Nucleases for Validation | T7 Endonuclease I, Surveyor Nuclease | Detects mismatches in heteroduplex DNA | Limited sensitivity for single-nucleotide changes [60] |
| Cell Culture Media | DMEM + 10% FBS + antibiotics | Supports cell growth and maintenance | Standardized conditions essential for reproducibility [60] |
| qEva-CRISPR Probes | Custom oligonucleotide probes | Target-specific hybridization and quantification | Designed with MLPA technology principles [60] |
Inter-platform Efficiency Comparison
Critical factors influencing delivery platform efficiency include cellular uptake mechanisms, endosomal escape capability, nuclear localization efficiency, and cargo stability [8]. The editing efficiency depends strongly on the delivery of CRISPR-Cas9 components into the cell nucleus [8]. Physical methods generally provide high efficiency ex vivo but limited in vivo applicability. Viral vectors offer exceptional transduction efficiency but present safety concerns including immunogenicity and insertional mutagenesis [2]. Non-viral systems balance safety and efficiency, with ongoing optimization focusing on material properties and surface functionalization [8].
Diagram 2: Relationship between delivery platforms, mechanisms, and efficiency profiles.
This application note provides a comprehensive framework for comparing efficiency metrics across CRISPR-Cas9 delivery platforms. The optimal delivery strategy depends on the specific research application, target cell type, and desired balance between efficiency and safety. As CRISPR technologies advance toward clinical translation, standardized assessment methods like qEva-CRISPR will be essential for accurate comparison of emerging delivery platforms. Researchers should consider both quantitative efficiency metrics and practical experimental parameters when selecting delivery systems for their genome editing applications.
The therapeutic application of CRISPR-Cas9 gene editing represents a paradigm shift in biomedical science, offering potential cures for genetic diseases that were once considered untreatable. However, the clinical success of this revolutionary technology is fundamentally constrained by one critical factor: the efficiency and safety of delivery systems. The CRISPR-Cas9 machinery—including the Cas nuclease and guide RNA (gRNA)—must be successfully transported into the nucleus of target cells to perform its editing function, a process fraught with biological barriers [10] [8]. The choice of delivery method directly influences key therapeutic outcomes, including editing efficiency, specificity, durability of effect, and safety profile [1] [9].
Recent clinical trials have validated both viral and non-viral delivery platforms, with significant advancements in lipid nanoparticle (LNP)-mediated in vivo delivery and continued refinement of ex vivo electroporation techniques. This application note synthesizes efficacy and safety data from landmark clinical studies completed in 2024-2025, with a specific focus on how delivery system selection has directly impacted therapeutic outcomes. Furthermore, we provide detailed protocols supporting the evaluation of novel delivery platforms and their edited products, creating an essential resource for researchers and drug development professionals navigating this rapidly evolving landscape.
Recent Clinical Trial Results: Efficacy and Safety Profiles
In Vivo Gene Editing via Lipid Nanoparticles (LNPs)
CTX310 for Dyslipidemias (ANGPTL3 Targeting)
A landmark Phase 1 trial (CRISPR-Cas9) demonstrated the safety and efficacy of CTX310, an LNP-formulated CRISPR-Cas9 therapy designed to disrupt the ANGPTL3 gene in hepatocytes via a single intravenous administration [61] [62] [63]. This trial represents a significant advance in in vivo CRISPR delivery, showing that systemic LNP delivery can achieve clinically meaningful gene editing in humans.
Table 1: Efficacy Outcomes from CTX310 Phase 1 Trial
| Dose (mg/kg) | N | Mean ANGPTL3 Reduction | Mean LDL-C Reduction | Mean Triglyceride Reduction | Timing of Assessment |
|---|---|---|---|---|---|
| 0.1 | 3 | +9.6% | +4.2% | +46.7% | Day 90 |
| 0.3 | 3 | +9.4% | +15.4% | +38.8% | Day 90 |
| 0.6 | 3 | -32.7% | -39.2% | -62.0% | Day 90 |
| 0.7 | 2 | -79.7% | -21.0% | -19.2% | Day 60 |
| 0.8 | 4 | -73.2% | -48.9% | -55.2% | Day 60 |
The safety profile was promising, with no dose-limiting toxicities or treatment-related serious adverse events (SAEs) reported [63]. Adverse events included mild-to-moderate infusion-related reactions (20% of participants) and one case of transient, asymptomatic liver transaminase elevation that resolved spontaneously [61] [62]. One sudden death occurred 179 days post-treatment in the lowest dose cohort but was deemed unrelated to CTX310 by investigators [62] [63]. The dose-dependent efficacy and acceptable safety profile observed in this trial underscore the potential of LNP delivery for in vivo gene editing, supporting continued clinical development.
Intellia Therapeutics Programs (hATTR and HAE)
Intellia's ongoing clinical programs further validate the LNP delivery platform for in vivo CRISPR-Cas9 gene editing. Their Phase 1 trial for hereditary transthyretin amyloidosis (hATTR) demonstrated that a single LNP infusion achieved rapid, deep, and durable reductions in serum TTR protein levels, with an average reduction of approximately 90% sustained for over two years of follow-up [5]. Similarly, their program for hereditary angioedema (HAE) showed that LNP-mediated knockdown of kallikrein resulted in an 86% reduction in the target protein and a significant decrease in HAE attacks, with 8 of 11 participants in the high-dose group being attack-free during the 16-week observation period [5].
A notable finding from Intellia's trials was the successful redosing of three participants who initially received a lower dose, marking the first report of multiple administrations of an in vivo CRISPR therapy [5]. This redosing capability, facilitated by the lower immunogenicity of LNPs compared to viral vectors, provides crucial flexibility for clinical management.
Personalized In Vivo CRISPR Therapy
In a groundbreaking case reported in May 2025, a multi-institutional team developed a bespoke in vivo CRISPR therapy for an infant with CPS1 deficiency, a rare metabolic disorder [5]. The treatment utilized LNP delivery and was developed, approved, and administered in just six months—an unprecedented timeline for a novel genetic therapy.
The infant received three IV infusions of the LNP-formulated CRISPR therapy, with each subsequent dose increasing the percentage of edited hepatocytes [5]. The patient showed significant clinical improvement, including reduced medication dependence and improved growth, with no serious side effects reported [5]. This case establishes a regulatory and technical precedent for rapid development of personalized CRISPR therapies for rare genetic disorders, highlighting the versatility of LNP-based delivery systems.
Ex Vivo CRISPR Editing for Hematological Disorders
CASGEVY (Exagamglogene Autotemcel)
CASGEVY, the first FDA-approved CRISPR-based therapy for sickle cell disease and transfusion-dependent beta thalassemia, utilizes ex vivo delivery via electroporation rather than in vivo delivery [8]. This approach involves extracting a patient's hematopoietic stem cells, editing them ex vivo using CRISPR-Cas9 delivered by electroporation, and then reinfusing the modified cells back into the patient.
Clinical trials demonstrated that this ex vivo strategy achieved high editing efficiency (up to 90% indels in the BCL11A gene target) and profound clinical benefits, with the majority of patients achieving freedom from vaso-occlusive crises or transfusion independence [8]. The electroporation delivery method enables precise control over editing efficiency and thorough quality control testing before patient reinfusion, though it involves a more complex and costly manufacturing process compared to in vivo approaches.
Experimental Protocols for Delivery System Evaluation
Protocol: Evaluating Gene Editing Outcomes via eGFP-to-BFP Conversion Assay
This protocol enables rapid, quantitative assessment of gene editing efficiency and DNA repair outcomes following CRISPR-Cas9 delivery, applicable for screening novel delivery systems [16].
1. Generation of eGFP-Positive Reporter Cell Lines
- Procedure: Seed HEK293T cells (or target cell line of interest) in 6-well plates at 70% confluency. Transfert with lentiviral packaging plasmids (psPAX2, pMD2.G) and a transfer plasmid encoding eGFP under a constitutive promoter. Harvest viral supernatant 48-72 hours post-transfection, filter through 0.45μm membrane, and transduce target cells with viral supernatant plus 8μg/mL polybrene. Select successfully transduced cells using flow cytometry (FACS) or antibiotic selection to establish a stable eGFP-positive population [16].
2. Delivery of CRISPR-Cas9 Components
- Delivery Optimization: For viral delivery of CRISPR components, utilize AAV vectors encoding Cas9 and BFP donor template with appropriate homology arms. For non-viral delivery, prepare Cas9 RNP complexes by incubating recombinant Cas9 protein with sgRNA targeting the eGFP sequence (5'-GGGCGAGGAGCTGTTCACC-3') at 37°C for 10 minutes. Deliver RNPs via electroporation (Neon System: 1400V, 20ms, 2 pulses) or lipid nanoparticles (formulate RNPs using ionizable lipids such as DLin-MC3-DMA at 3:1:1:0.3 lipid:PS:CH:PG ratio) [16].
3. Analysis of Editing Outcomes
- Flow Cytometry: Harvest cells 72-96 hours post-editing, wash with PBS, and analyze using flow cytometry with appropriate laser/filter configurations (eGFP: 488nm excitation/507nm emission; BFP: 405nm excitation/450nm emission). Calculate editing efficiency as percentage of BFP-positive cells among total live cells [16].
- Sequencing Validation: Isolate genomic DNA from edited populations, amplify target locus via PCR, and perform Sanger or next-generation sequencing to confirm precise HDR-mediated conversion and quantify indel frequencies from NHEJ [16].
Protocol: Extracellular Vesicle-Mediated Cas9 RNP Delivery
This protocol details a modular system for loading and delivering CRISPR-Cas9 components via engineered extracellular vesicles (EVs), offering a potentially safer alternative to viral vectors and synthetic nanoparticles [7].
1. Production of Cas9-Loaded EVs
- Plasmid Design: Construct plasmids encoding: (1) MCP-CD63 fusion protein (tandem MS2 coat proteins fused to N-terminus of CD63); (2) Cas9 (or variant); (3) MS2-sgRNA (sgRNA with MS2 aptamers incorporated in tetraloop and stemloop 2) [7].
- EV Generation: Co-transfect HEK293T cells with the three plasmids using PEI Max transfection reagent. Harvest conditioned media 48 hours post-transfection, centrifuge at 2,000 × g for 20 minutes to remove cells and debris, then concentrate using tangential flow filtration (100kDa MWCO) [7].
- EV Purification: Purify EVs by size exclusion chromatography (qEV original columns), then characterize by nanoparticle tracking analysis (mode ~75nm), transmission electron microscopy, and western blotting for EV markers (CD63, ALIX, TSG101) and absence of calnexin [7].
2. UV Activation and Functional Assay
- Cargo Release: Treat isolated EVs with 405nm UV light (100mJ/cm²) to cleave the PhoCl linker and release Cas9 RNP complexes from the EV membrane [7].
- Editing Assessment: Incubate target cells with UV-activated EVs for 48 hours, then analyze editing efficiency via T7E1 assay or targeted next-generation sequencing of the genomic locus targeted by the MS2-sgRNA [7].
The following diagram illustrates the modular EV-mediated Cas9 delivery system:
Diagram Title: Modular EV-Mediated Cas9 Delivery Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for CRISPR-Cas9 Delivery Research
| Reagent/Category | Specific Examples | Function/Application | Delivery Context |
|---|---|---|---|
| Viral Vectors | AAV (serotypes 2, 8, 9), Lentivirus (VSV-G pseudotyped) | High-efficiency in vivo delivery; tissue-specific tropism | AAV for liver targeting (4.7kb cargo limit); Lentivirus for ex vivo cell engineering |
| Lipid Nanoparticles | DLin-MC3-DMA, SM-102, ALC-0315 | Encapsulation and delivery of Cas9 mRNA, sgRNA, or RNP complexes | In vivo systemic delivery; organ-selective targeting (e.g., liver) via SORT molecules |
| Electroporation Systems | Neon Transfection System, Amaxa Nucleofector | Physical delivery of RNP complexes to hard-to-transfect cells | Ex vivo editing of hematopoietic stem cells, T cells, primary cells |
| Extracellular Vesicle Tools | MCP-CD63 fusion construct, MS2-sgRNA, PhoCl linker | Modular EV loading and UV-triggered release of Cas9 RNP | Alternative delivery with potentially improved biocompatibility |
| Editing Reporter Systems | eGFP-BFP conversion cassette, GUIDE-seq | Quantitative measurement of editing efficiency and specificity | Screening delivery system performance; assessing on-target vs. off-target activity |
| Cas9 Variants | HiFi Cas9, Cas12a (Cpf1), saCas9, ABE8e, BE4max | Improved specificity, altered PAM requirements, reduced size, base editing | Matching nuclease properties to delivery constraints (e.g., saCas9 for AAV packaging) |
Recent clinical trials have unequivocally demonstrated that delivery system selection is paramount to achieving safe and effective CRISPR-based therapies. The data from 2024-2025 highlight distinct advantages for different delivery modalities: LNP systems enable scalable in vivo administration with favorable safety profiles and potential for redosing; ex vivo electroporation provides precise control for hematological applications; and emerging EV-based platforms offer promising alternatives with modular design capabilities.
Future development will likely focus on overcoming remaining delivery challenges, including enhancing tissue specificity beyond the liver, improving editing efficiency in difficult-to-transfect cell types, and further reducing immunogenic potential. The continued refinement of both viral and non-viral delivery systems, coupled with robust analytical protocols for evaluating their performance, will accelerate the clinical translation of CRISPR-based therapies for an expanding range of genetic disorders.
The therapeutic application of CRISPR-Cas9 technology is fundamentally constrained by the challenge of efficiently delivering its molecular components into the nuclei of target cells. A critical and often underestimated factor determining the success of gene editing experiments is the pronounced dependence of delivery efficiency on cell type. Even when using identical delivery methods and reagents, different cell types can exhibit dramatically different transfection and editing outcomes due to variations in their physiology, membrane composition, endocytic trafficking, and nuclear import mechanisms [8] [29]. This application note, situated within a broader thesis on CRISPR-Cas9 delivery, synthesizes recent findings to provide researchers with a structured comparison of delivery efficiency across cell types and detailed protocols for optimizing delivery strategies based on cellular characteristics.
Quantitative Comparison of Delivery Efficiency Across Cell Types
The efficiency of CRISPR-Cas9 delivery is a composite metric, often measured as transfection efficiency (successful cellular uptake of CRISPR components) and editing efficiency (the percentage of cells with intended genetic modifications at the target locus). These metrics vary significantly based on the delivery method and the target cell line.
Table 1: Comparison of Delivery Efficiencies Across Cell Types and Methods
| Delivery Method | Cell Type / Model | Transfection Efficiency | Editing Efficiency | Key Findings | Citation |
|---|---|---|---|---|---|
| Electroporation (RNP) | Gilthead Seabream Brain 1 (SaB-1) | ~78% | Up to ~95% | High efficiency under optimized conditions (1800 V, 20 ms, 2 pulses). | [29] |
| Electroporation (RNP) | European Seabass Brain 1 (DLB-1) | ~75% | ~10% - 28% | Highly sensitive to parameters; locus-specific genomic rearrangements suspected. | [29] |
| Lipid Nanoparticles (LNP) | European Seabass Brain 1 (DLB-1) | Not Specified | ~25% | Achieved moderate editing in a difficult-to-transfect line. | [29] |
| Lipid Nanoparticles (LNP) | Gilthead Seabream Brain 1 (SaB-1) | Not Specified | Minimal | Demonstrated stark cell-line-dependent barrier to editing post-delivery. | [29] |
| Magnetofection (SPIONs) | Marine Fish Cell Lines (DLB-1, SaB-1) | Efficient Uptake | No detectable editing | Highlights post-entry barriers (e.g., endosomal escape, nuclear import) independent of uptake. | [29] |
| Extracellular Vesicles (EVs) | HEK293T (Producer) | N/A | N/A | Modular aptamer-based system successfully loaded Cas9 RNPs into EVs for delivery. | [7] |
The data in Table 1 underscores that high transfection efficiency does not guarantee successful gene editing. Intracellular barriers, such as endosomal entrapment, inefficient nuclear localization, and even the genomic stability of the target locus, can severely limit the final editing outcome [29]. Furthermore, the source of sgRNA (in vitro transcribed vs. chemically synthesized) can also impact editing efficiency in a cell-dependent manner [29].
Experimental Protocols for Assessing Cell-Type-Dependent Delivery
To achieve reproducible and efficient gene editing, it is essential to systematically evaluate and optimize delivery conditions for each new cell type. The following protocols provide a framework for this process.
Protocol: Optimization of Electroporation for RNP Delivery in Adherent Cell Lines
This protocol is adapted from a study on marine fish cell lines and can be adapted for other hard-to-transfect adherent cells [29].
Research Reagent Solutions:
- Cas9 Protein: Recombinantly expressed and purified Streptococcus pyogenes Cas9.
- sgRNA: Chemically synthesized, chemically modified sgRNA (e.g., from Synthego) for enhanced stability.
- Electroporation Buffer: Cell-type-specific optimized buffer, often provided by commercial kits.
- Cell Culture Media: Standard growth media supplemented with appropriate serum and antibiotics.
Procedure:
- Cell Preparation: Harvest adherent cells at ~80% confluency using a gentle dissociation reagent. Wash the cell pellet twice with PBS and resuspend in the electroporation buffer at a concentration of 1-5 x 10^6 cells/mL.
- RNP Complex Formation: Pre-complex the Cas9 protein with sgRNA at a molar ratio of 1:2 (e.g., 3 µM Cas9 with 6 µM sgRNA) in a separate tube. Incubate at room temperature for 10-20 minutes to form the RNP complex.
- Electroporation: Mix 10 µL of the cell suspension with 2-5 µL of the prepared RNP complex. Transfer the mixture to a 96-well electroporation cuvette. Apply electrical pulses using a predefined parameter matrix. For initial testing, a range of voltages (e.g., 1500-1800 V), pulse widths (10-20 ms), and pulse numbers (1-3) should be tested.
- Post-Electroporation Recovery: Immediately after pulsing, transfer the cells to pre-warmed complete culture media. Seed the cells onto tissue culture plates and incubate at standard conditions (e.g., 28°C or 37°C with 5% CO₂).
- Efficiency Assessment:
- Transfection Efficiency: At 1-4 hours post-electroporation, analyze cells using flow cytometry or confocal microscopy if using fluorescently labeled Cas9 (e.g., Cas9-Cy3).
- Cell Viability: At 24-48 hours post-electroporation, perform a viability assay (e.g., trypan blue exclusion).
- Editing Efficiency: At 48-72 hours post-electroporation, harvest cells and extract genomic DNA. Assess editing at the target locus via T7E1/Surveyor assay, targeted sequencing (e.g., Illumina MiSeq), or inference of CRISPR edits (ICE) analysis of Sanger sequencing data.
Protocol: Modular Loading of Cas9 RNP into Extracellular Vesicles (EVs)
This protocol describes a versatile strategy for loading various Cas9 variants into EVs via aptamer-binding, suitable for delivery to sensitive or hard-to-transfect cell types [7].
Research Reagent Solutions:
- Plasmids:
- pMCP-CD63-PhoCl: Expressing tandem MS2 coat protein (MCP) fused to the tetraspanin CD63, separated by the UV-cleavable PhoCl linker.
- pCas9: Expressing the Cas9 protein (or variant, e.g., ABE8e, dCas9-VPR).
- pMS2-sgRNA: Expressing the single-guide RNA with MS2 aptamers incorporated into its tetraloop and stemloop.
- Isolation Buffers: PBS or other physiological buffers suitable for TFF and SEC.
- Characterization Reagents: Antibodies for CD63, CD9, ALIX, TSG101 (EV markers) and Calnexin (negative marker) for Western Blot.
Procedure:
- EV Production and Loading: Co-transfect HEK293T cells (or another suitable producer cell line) with the three plasmids (pMCP-CD63-PhoCl, pCas9, pMS2-sgRNA) using a standard transfection method. The MCP-CD63 fusion is incorporated into the membranes of forming EVs, while the Cas9 RNP complex with protruding MS2 aptamers is assembled in the cytoplasm. The high-affinity MS2-MCP binding leads to the enrichment of the RNP inside the EVs during their biogenesis.
- EV Harvest and Isolation: 48 hours post-transfection, collect the cell culture supernatant. Centrifuge at low speed (e.g., 2,000 x g) to remove cells and debris, then at 10,000 x g to remove larger particles. Concentrate the EV-containing supernatant and exchange the buffer using Tangential Flow Filtration (TFF). Further purify the EVs using Size Exclusion Chromatography (SEC) to separate EVs from soluble proteins and non-vesicular contaminants.
- EV Characterization:
- Concentration and Size: Use Nanoparticle Tracking Analysis (NTA) to determine the particle size distribution and concentration.
- Purity: Perform Western Blot analysis to confirm the presence of EV markers (CD63, ALIX, TSG101) and the absence of negative markers (Calnexin).
- Cargo Validation: Use Western Blot to confirm Cas9 protein loading and digital droplet PCR (ddPCR) to quantify MS2-sgRNA loading compared to control EVs without the MCP-CD63 loader.
- Functional Delivery: Incubate the isolated, RNP-loaded EVs with the target recipient cells. To release the Cas9 RNP from the EV membrane inside the cell, expose the cell-EV culture to UV light (e.g., 405 nm), which cleaves the PhoCl linker, freeing the functional RNP into the cytoplasm [7].
The Scientist's Toolkit: Key Reagents for Delivery Optimization
Table 2: Essential Research Reagents for CRISPR-Cas9 Delivery Experiments
| Reagent / Tool | Function | Application Notes |
|---|---|---|
| Cas9 Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and sgRNA; offers high editing efficiency and rapid kinetics while minimizing off-target effects. | The gold standard cargo for electroporation and nanoparticle delivery. Reduces host immune responses compared to plasmid DNA. |
| Chemically Modified sgRNA | Synthetic sgRNA with phosphorothioate bonds and 2'-O-methyl analogs; increases nuclease resistance and stability. | Outperforms in vitro transcribed (IVT) sgRNA in many cell types, particularly in sensitive or primary cells [29]. |
| MS2-MCP Loading System | A modular system for loading Cas9 RNP into vesicles via RNA-protein interaction. | Enables high-efficiency loading of various Cas9 variants (e.g., base editors) into EVs without direct protein fusion [7]. |
| UV-Cleavable Linker (PhoCl) | A protein domain that undergoes specific backbone cleavage upon exposure to UV light. | Used in fusion proteins to enable controlled release of cargo (e.g., Cas9 RNP) after cellular uptake [7]. |
| Fluorescently Labeled Cas9 | Cas9 protein conjugated to a fluorophore (e.g., Cy3, Cy5). | Essential for quantifying transfection efficiency and visualizing intracellular and nuclear localization via flow cytometry or confocal microscopy [29]. |
The path to successful CRISPR-Cas9-mediated gene editing is inextricably linked to a deep understanding of the target cell's biology. There is no universal delivery method. As demonstrated, identical protocols can yield efficiencies ranging from undetectable to over 90% depending on the cell line [29]. A systematic, empirical approach—characterizing transfection, viability, and editing efficiency while being mindful of intracellular barriers and Cas9 protein behavior—is therefore non-negotiable for robust experimental outcomes and the successful translation of CRISPR technologies into therapeutic applications.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 system has emerged as a transformative technology in genetic engineering, offering unprecedented capability for precise genome modification. This revolutionary tool holds immense promise for treating countless genetic diseases by directly correcting pathogenic mutations [55]. However, a significant bottleneck hinders its clinical translation: the safe and efficient intracellular delivery of its molecular machinery [64] [65].
The CRISPR-Cas9 system, comprising the Cas9 nuclease and a guide RNA (gRNA), cannot passively cross cell membranes due to its large size and negative charge [7] [1]. Current delivery strategies, primarily viral vectors and lipid nanoparticles (LNPs), present substantial limitations. Viral vectors, while efficient, can trigger immunogenic responses and have limited cargo capacity [64] [1]. LNPs, famously used in COVID-19 vaccines, are safer but often suffer from inefficient endosomal escape, leading to degradation of their cargo before it reaches the nucleus [64] [66]. Structural nanomedicine, an emerging field that emphasizes the importance of a nanomaterial's architecture—not just its composition—offers a promising path forward [64] [67]. By designing sophisticated nanostructures, researchers are creating next-generation delivery vehicles that could unlock the full therapeutic potential of CRISPR.
A groundbreaking advance in this field is the development of Lipid Nanoparticle Spherical Nucleic Acids (LNP-SNAs) by researchers at Northwestern University [64] [67]. This platform strategically marries two powerful biotechnologies: the cargo-protecting capacity of LNPs and the superior cellular uptake properties of Spherical Nucleic Acids (SNAs).
The LNP-SNA is a core-shell nanostructure with distinct functional components. At its heart is an LNP core, which encapsulates the full suite of CRISPR editing tools—the Cas9 enzyme, gRNA, and a DNA repair template [64] [68]. Surrounding this core is a dense, radially oriented shell of short, synthetic DNA strands, forming the SNA architecture [64]. This DNA shell is not merely protective; it is functionally critical. The DNA interacts with cell surface receptors, facilitating rapid and efficient cellular internalization across a wide range of cell types, a process that is independent of transfection agents [64] [67] [69]. The entire structure is roughly 50 nanometers in diameter [67].
A key principle demonstrated by this technology is that the three-dimensional architecture of the nanomaterial is a primary determinant of its biological function. The globular, high-density DNA presentation of the SNA is fundamentally different from linear DNA and is recognized almost universally by cells, leading to active and rapid uptake [64]. This structural consideration is as important as the chemical ingredients themselves, underscoring the core tenet of structural nanomedicine [64].
Quantitative Performance Data
In rigorous laboratory tests, the LNP-SNA platform has demonstrated superior performance across multiple critical metrics compared to standard delivery systems. The following table summarizes the key quantitative findings from studies involving various human and animal cell types, including skin cells, white blood cells, human bone marrow stem cells, and human kidney cells [64] [67] [68].
Table 1: Performance Metrics of LNP-SNAs vs. Standard Lipid Nanoparticles
| Performance Metric | LNP-SNA Performance | Comparison to Standard LNP |
|---|---|---|
| Cellular Uptake Efficiency | Entered cells up to 3 times more effectively [64] [66] | 3x improvement [64] |
| Gene-Editing Efficiency | Boosted editing efficiency threefold [64] [68] | 3x improvement [64] |
| Precise DNA Repair (HDR) | Improved success rate by >60% [64] [67] | >60% improvement [64] |
| Cellular Toxicity | Caused far less toxicity [64] | Significantly reduced [64] |
The data unequivocally shows that the LNP-SNA architecture not only enhances the delivery and editing efficiency but also does so with a markedly improved safety profile. The >60% improvement in homology-directed repair (HDR) is particularly noteworthy, as achieving precise gene correction has been a major challenge in the field [55].
Detailed Experimental Protocol
This section provides a detailed methodology for the synthesis, application, and validation of LNP-SNAs for CRISPR-Cas9 delivery, as derived from the featured research.
Synthesis of LNP-SNAs
Objective: To fabricate LNP-SNAs carrying the complete CRISPR-Cas9 machinery. Materials:
- Lipid Nanoparticle (LNP) Core Components: Cationic or ionizable lipids, phospholipids, cholesterol, and PEG-lipids [65].
- CRISPR Payload: Cas9 protein (or mRNA), single-guide RNA (sgRNA), and optional single-stranded DNA (ssDNA) repair template for HDR [64].
- DNA Shell: Short, synthetic DNA strands (~20-30 nucleotides); these can be modified with chemical groups (e.g., thiols) for conjugation [64] [69].
- Buffers: Nuclease-free water, citrate buffer (pH 4.0), 1x PBS (pH 7.4).
- Equipment: Microfluidic mixer or tubing-based setup, bath sonicator, centrifugal filtration devices (e.g., 100 kDa MWCO).
Procedure:
- LNP Core Formation: Using a rapid-mixing microfluidic device, combine an aqueous phase containing the CRISPR payload (e.g., pre-complexed Cas9-ribonucleoprotein with or without donor DNA) with an ethanol phase containing the lipid mixture. This results in the spontaneous formation of LNPs encapsulating the cargo [65].
- Purification: Dialyze or use tangential flow filtration against 1x PBS (pH 7.4) to remove residual ethanol and exchange the buffer.
- DNA Shell Conjugation: Incubate the purified LNPs with an excess of the short DNA strands. For thiol-modified DNA, this process may rely on disulfide bond formation or use of a crosslinker. Incubate for 12-16 hours at room temperature with gentle agitation [64] [69].
- Purification of LNP-SNAs: Remove unbound DNA strands using centrifugal filtration or size-exclusion chromatography. The final LNP-SNA product can be suspended in 1x PBS and stored at 4°C.
In Vitro Cell Transduction and Gene Editing
Objective: To deliver the LNP-SNAs to target cells and assess gene-editing outcomes. Materials:
- Cell Lines: Relevant human cell types (e.g., HEK293T, primary T-cells, human bone marrow stem cells) [64].
- Cell Culture Media: Appropriate complete media (e.g., DMEM, RPMI-1640) with serum.
- LNP-SNAs (from Protocol 4.1).
- Control Formulations: Standard LNPs (without DNA shell) and/or naked CRISPR machinery.
- Equipment: Cell culture incubator (37°C, 5% CO2), flow cytometer, fluorescence microscope, genomic DNA extraction kit.
Procedure:
- Cell Seeding: Seed target cells in a multi-well plate (e.g., 24-well plate) at a density of 1-2 x 10^5 cells per well and culture overnight.
- Transduction: Replace the medium with fresh medium containing the LNP-SNAs at a predetermined concentration (e.g., 10-100 nM CRISPR cargo). Include controls (untreated cells, cells treated with standard LNPs).
- Incubation: Incubate cells for 48-72 hours to allow for cellular uptake, cargo release, and gene editing.
- Harvesting: Harvest cells for downstream analysis.
Analytical and Validation Methods
Objective: To quantify the efficiency of delivery and gene editing. 1. Cellular Uptake and Internalization:
- Flow Cytometry: If the LNP-SNA core is loaded with a fluorescent dye or the sgRNA is fluorescently labeled, analyze cells by flow cytometry to determine the percentage of positive cells and mean fluorescence intensity [64].
- Confocal Microscopy: Use to visually confirm intracellular localization of fluorescently tagged particles and confirm endosomal escape.
2. Cytotoxicity Assessment:
- Perform a standard MTT or CellTiter-Glo assay 24-48 hours post-transduction to assess cell viability relative to untreated controls. LNP-SNAs have been shown to cause "far less toxicity" than standard methods [64].
3. Gene-Editing Efficiency Analysis:
- T7 Endonuclease I Assay or Tracking of Indels by Decomposition (TIDE): Extract genomic DNA from harvested cells. Amplify the target genomic locus by PCR and treat with T7E1 enzyme, which cleaves mismatched heteroduplex DNA formed by indels. Analyze fragments by gel electrophoresis. Alternatively, use Sanger sequencing and the TIDE web tool to quantify insertion/deletion mutations [55].
- Flow Cytometry for Reporter Genes: If editing a fluorescent protein gene (e.g., GFP knockout), directly quantify the loss of fluorescence.
- Next-Generation Sequencing (NGS): For the most accurate and comprehensive quantification of editing efficiency and specificity, subject the PCR-amplified target site to NGS.
The experimental workflow for using LNP-SNAs in CRISPR gene editing, from synthesis to validation, is summarized below.
Diagram Title: LNP-SNA Experimental Workflow
The Scientist's Toolkit: Key Research Reagents
Successful implementation of the LNP-SNA platform relies on a set of core components and reagents. The table below details these essential materials and their functions.
Table 2: Essential Research Reagents for LNP-SNA CRISPR Delivery
| Reagent/Material | Function & Role in the System |
|---|---|
| Ionizable/Cationic Lipids | Forms the core structure of the LNP; enables encapsulation of nucleic acid/protein cargo via electrostatic interaction [65]. |
| Cas9 Ribonucleoprotein (RNP) | The active gene-editing complex; direct RNP delivery is transient, reducing off-target effects compared to DNA plasmid delivery [7] [1]. |
| Single-Guide RNA (sgRNA) | Directs the Cas9 protein to the specific genomic target sequence via complementary base-pairing [55]. |
| Synthetic DNA Strands | Forms the protective, functional shell around the LNP; facilitates high-efficiency cellular uptake by engaging cell surface receptors [64] [69]. |
| DNA Repair Template | A single-stranded or double-stranded DNA oligonucleotide providing the correct sequence for homology-directed repair (HDR) to achieve precise gene correction [64]. |
| Microfluidic Mixer | Essential equipment for producing uniform, monodisperse LNPs with high encapsulation efficiency via rapid mixing of aqueous and lipid phases [65]. |
Comparative Analysis with Other Delivery Platforms
The advent of LNP-SNAs provides a compelling alternative to existing delivery technologies. The following diagram and table contextualize this new platform against other prominent strategies.
Diagram Title: CRISPR Delivery Methods Comparison
Table 3: Comparison of CRISPR-Cas9 Delivery Platforms
| Delivery Platform | Key Advantages | Key Limitations |
|---|---|---|
| LNP-Spherical Nucleic Acid | High cellular uptake (3x standard LNP); Low toxicity; Boosts precise HDR by >60%; Modular & tunable shell [64] [67]. | Still in pre-clinical validation; long-term stability data being gathered [64]. |
| Standard Lipid Nanoparticle (LNP) | Proven clinical safety (mRNA vaccines); Scalable production; Protects nucleic acid cargo [65] [1]. | Inefficient endosomal escape; Can be cytotoxic; Lower editing efficiency [64] [66]. |
| Adeno-Associated Virus (AAV) | High transduction efficiency; Long-term transgene expression [1]. | Small payload capacity (<4.7 kb); Pre-existing immunity in patients; Risk of immunogenic response [64] [1]. |
| Lentiviral Vector (LV) | Large cargo capacity; Infects dividing and non-dividing cells [1]. | Integration into host genome (mutagenesis risk); Complex production [1]. |
| Extracellular Vesicles (EVs) | Native biocompatibility; Low immunogenicity; Potential for natural tissue targeting [7]. | Heterogeneous population; Complex manufacturing and loading at scale [7] [1]. |
The development of LNP-SNAs represents a paradigm shift in CRISPR delivery, moving beyond a purely chemical view of nanoparticles to a structural one. By prioritizing architecture, this platform directly addresses the critical bottlenecks of cellular uptake and endosomal escape that have plagued non-viral methods [64] [66]. The quantitative results—a threefold boost in editing efficiency and a greater than 60% improvement in precise DNA repair—demonstrate the tangible impact of this structural approach [64] [67].
The future of this technology is vibrant. The modular nature of the LNP-SNA allows for the DNA shell to be engineered with specific sequences (e.g., aptamers) to actively target particular cell types or tissues, further enhancing specificity and reducing off-target effects [64] [69]. The research team plans to validate the system in multiple in vivo disease models, a crucial step toward clinical translation [64]. Furthermore, the core concept is adaptable for delivering other large biomolecular therapeutics beyond CRISPR-Cas9, such as base editors, transcriptional regulators, and other nucleases [7].
As the field of structural nanomedicine matures, DNA-coated nanostructures like LNP-SNAs are poised to play a central role in realizing the promise of gene editing, potentially enabling therapies for a vast range of genetic disorders that are currently untreatable. The journey from bench to bedside is ongoing, with commercial partners like Flashpoint Therapeutics already working to advance this technology into clinical trials [64] [67].
The transition of CRISPR-Cas9 technology from research laboratories to clinical applications represents one of the most significant advancements in modern biotechnology. While the core gene-editing mechanism remains consistent across these domains, the practical considerations for delivery method selection diverge considerably based on distinct priorities and constraints. Research environments often prioritize editing efficiency, versatility, and cost-effectiveness, whereas clinical translation demands rigorous safety profiles, manufacturability, and predictable pharmacokinetics [10] [70]. This application note provides a structured framework for evaluating CRISPR-Cas9 delivery methods across the development continuum, offering detailed protocols and analytical tools to inform decision-making for researchers and therapeutic developers.
The fundamental challenge underlying all CRISPR applications remains efficient delivery of editing components to target cells [1]. This process involves two critical considerations: the molecular cargo format (DNA, mRNA, or ribonucleoprotein) and the delivery vehicle or method [1]. Each combination presents unique trade-offs between editing efficiency, persistence, specificity, and safety, with optimal choices varying significantly between basic research and clinical applications [10] [70].
Comparative Analysis of Delivery Methodologies
Quantitative Comparison of Delivery Platforms
Table 1: Delivery Method Comparison for Research Versus Clinical Applications
| Delivery Method | Cargo Format | Typical Use Context | Key Research Advantages | Key Clinical Advantages | Primary Research Limitations | Primary Clinical Limitations |
|---|---|---|---|---|---|---|
| Viral Vectors (AAV) | DNA | In vivo research & clinical trials | High efficiency for difficult-to-transfect cells; sustained expression for long-term studies [1] | Well-characterized regulatory profile; tissue-specific targeting [1] [71] | Limited packaging capacity (~4.7kb); potential for genomic integration [10] [1] | Immunogenicity concerns; pre-existing immunity in populations; potential for genotoxicity [72] [73] |
| Viral Vectors (Lentivirus) | DNA | Ex vivo research & clinical trials | Broad tropism; stable genomic integration for permanent expression [1] | Proven success in ex vivo therapies (e.g., hematopoietic stem cells) [71] | Insertional mutagenesis risk; complex production [1] | More extensive safety testing required due to integration risk [73] |
| Lipid Nanoparticles (LNPs) | mRNA, RNP | In vivo research & clinical trials | Flexibility in cargo encapsulation; suitability for diverse cell types [1] | FDA-approved delivery platform; organ-targeting capability (e.g., liver) [5] [71] | Variable efficiency across cell types; endosomal trapping [1] | Reactogenicity at high doses; liver-dominant distribution limits other targets [5] |
| Electroporation | RNP, mRNA | Ex vivo research & clinical trials | High efficiency for immune cells and stem cells; immediate editing with RNP [10] | Established in approved therapies (e.g., Casgevy); transient activity reduces off-target risks [5] [72] | Specialized equipment required; cell toxicity and mortality [10] | Limited to ex vivo applications; cell damage at suboptimal parameters [10] |
| Virus-Like Particles (VLPs) | Protein, RNP | Emerging research | Reduced immune recognition; transient editing window [1] | Potentially improved safety profile without viral genes [1] | Complex manufacturing; cargo size limitations [1] | Limited clinical validation; scale-up challenges [1] |
Decision Framework for Method Selection
The following workflow diagram outlines a systematic approach for selecting appropriate CRISPR-Cas9 delivery methods based on application requirements:
Diagram 1: CRISPR Delivery Method Selection Workflow. This decision tree outlines key considerations for selecting appropriate delivery methods based on application requirements, target tissue, and safety priorities.
Experimental Protocols and Workflows
Protocol 1: LNP-Mediated In Vivo Delivery for Liver-Directed Therapies
This protocol outlines methodology for lipid nanoparticle-mediated CRISPR delivery, particularly relevant for liver-directed therapies as demonstrated in recent clinical trials for hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) [5].
Reagents and Equipment
- CRISPR payload: Cas9 mRNA and sgRNA, or pre-complexed RNP
- Ionizable lipid: Proprietary or commercially available (e.g., DLin-MC3-DMA)
- Helper lipids: DSPC, cholesterol, PEG-lipid
- Formulation apparatus: Microfluidic mixer or T-tube configuration
- Purification equipment: Tangential flow filtration system
- Analytical instruments: Dynamic light scattering (DLS), nanoparticle tracking analysis
Step-by-Step Methodology
- Lipid Preparation: Prepare lipid mixture in ethanol at precise molar ratios (typically 50:10:38.5:1.5 ionizable lipid:DSPC:cholesterol:PEG-lipid)
- Aqueous Phase Preparation: Dilute CRISPR payload (mRNA at 0.2 mg/mL or RNP at 0.5 mg/mL) in citrate buffer (pH 4.0)
- Nanoparticle Formation: Combine lipid and aqueous phases using microfluidic mixer at 1:3 volumetric flow ratio (total flow rate 12 mL/min)
- Buffer Exchange: Dialyze or use TFF against PBS (pH 7.4) to remove ethanol and establish neutral pH
- Characterization: Determine particle size (target 70-100 nm), polydispersity index (<0.2), and encapsulation efficiency (>90%)
- Quality Control: Test for endotoxin (<5 EU/mL) and sterility
- In Vivo Administration: Administer via intravenous injection at dosage 0.5-3.0 mg CRISPR payload/kg body weight [5]
Key Parameters for Optimization
- Nitrogen-to-Phosphate (N/P) ratio: Critical for payload encapsulation and endosomal escape (typically 4-6)
- PEG-lipid content: Controls nanoparticle stability and pharmacokinetics (1-3 mol%)
- Storage conditions: Lyophilization may be required for long-term stability
Protocol 2: Electroporation for Ex Vivo Cell Engineering
This protocol details electroporation-based delivery for ex vivo applications, such as hematopoietic stem cell engineering used in Casgevy therapy for sickle cell disease and β-thalassemia [5].
Reagents and Equipment
- CRISPR payload: Pre-complexed Cas9-sgRNA RNP complex
- Cells for editing: Primary T-cells, hematopoietic stem cells, or other target population
- Electroporation system: Commercial platform (e.g., Lonza 4D-Nucleofector)
- Cell culture reagents: Appropriate media, cytokines, and supplements
- Validation tools: Next-generation sequencing, flow cytometry, functional assays
Step-by-Step Methodology
- RNP Complex Formation: Incubate purified Cas9 protein with sgRNA at 1:1.2 molar ratio in electroporation buffer for 10-15 minutes at room temperature
- Cell Preparation: Isolate and wash target cells, resuspend in appropriate electroporation buffer at 10-20×10^6 cells/mL
- Electroporation Setup: Combine cell suspension with RNP complex (typically 2-10 μg RNP per 10^6 cells) in electroporation cuvette
- Pulse Application: Apply optimized electrical parameters (e.g., 1500V, 20ms pulse for primary T-cells)
- Post-Electroporation Recovery: Immediately transfer cells to pre-warmed culture medium with supportive cytokines
- Culture and Expansion: Maintain cells for 48-72 hours before assessing editing efficiency
- Functional Validation: Perform targeted NGS for on-target and off-target analysis, assess phenotype and functionality
Critical Optimization Parameters
- Cell viability: Typically 50-70% post-electroporation, with >80% recovery after 24 hours
- Editing efficiency: Target >70% modification for therapeutic efficacy
- Cell-specific parameters: Electrical settings, recovery media, and RNP concentrations require optimization for each cell type
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for CRISPR-Cas9 Delivery Studies
| Reagent/Material | Function | Research Applications | Clinical Considerations | Leading Providers/Sources |
|---|---|---|---|---|
| High-Fidelity Cas9 Variants | Engineered Cas9 with reduced off-target effects | Basic research where specificity is paramount; off-target profiling studies [72] | Essential for therapeutic applications to minimize genotoxicity [72] | Integrated DNA Technologies, Thermo Fisher Scientific, Synthego |
| Ionizable Lipids | pH-responsive lipids for LNP formulation | In vivo delivery optimization; structure-activity relationship studies | Clinical-grade materials with established safety profiles (e.g., DLin-MC3-DMA) | Avanti Polar Lipids, BroadPharm, proprietary formulations |
| AAV Serotypes | Viral vectors with tissue-specific tropism | Tissue-specific delivery studies; long-term expression models | Serotype selection based on target tissue and pre-existing immunity | Vigene Biosciences, Addgene, VectorBuilder |
| Electroporation Systems | Physical delivery via electrical pulses | Ex vivo editing of primary cells; difficult-to-transfect cells | GMP-compatible systems for clinical cell processing | Lonza, Bio-Rad, MaxCyte |
| Ribonucleoprotein (RNP) Complex | Pre-complexed Cas9 and guide RNA | Rapid, transient editing with minimal off-target effects [1] | Preferred cargo format for ex vivo therapies due to safety profile [5] | Custom assembly from purified components |
| Off-Target Assessment Tools | Methods to detect unintended edits | Comprehensive safety profiling; gRNA validation | Regulatory requirement for therapeutic development [72] | GUIDE-seq, CIRCLE-seq, proprietary NGS assays |
Safety and Validation Considerations
Comprehensive Safety Profiling
The clinical translation of CRISPR therapies requires rigorous safety assessment beyond basic editing efficiency measurements. Recent studies have revealed that CRISPR editing can generate unexpected structural variations, including large deletions, chromosomal translocations, and complex rearrangements that may pose oncogenic risks [72].
Table 3: Safety Assessment Methods for Research Versus Clinical Development
| Risk Category | Research-Grade Assessment | Clinical-Grade Assessment | Recommended Mitigation Strategies |
|---|---|---|---|
| Off-Target Effects | In silico prediction tools; targeted NGS of predicted sites [74] | Genome-wide methods (e.g., GUIDE-seq, CIRCLE-seq); long-read sequencing [72] | High-fidelity Cas variants; optimized gRNA design; RNP delivery [72] |
| On-Target Structural Variations | PCR-based sizing assays; Southern blotting | CAST-Seq; LAM-HTGTS; long-range PCR with NGS [72] | Avoid DNA-PKcs inhibitors; monitor p53 pathway activation [72] |
| Immunogenicity | In vitro cytokine release assays | Extensive in vivo toxicology studies; clinical monitoring | Consider patient pre-existing immunity; use of non-viral delivery when possible [73] |
| Tumorigenicity | Cell transformation assays; p53 pathway monitoring | Long-term follow-up in animal models; integration site analysis | Careful donor cell selection; extensive genomic stability assessment [72] |
Analytical Methods Diagram
Diagram 2: CRISPR Editing Validation Workflow. Comprehensive analytical methods required to fully characterize editing outcomes, from basic efficiency measurements to complex structural variation detection.
The maturation of CRISPR-Cas9 delivery methods continues to bridge the gap between research innovation and clinical implementation. The current landscape demonstrates that no single delivery approach optimally serves all applications, necessitating context-specific evaluation of the cost-benefit considerations outlined in this document. Research applications can leverage the versatility of viral vectors and rapidly evolving nanoparticle systems, while clinical development requires more stringent safety-focused optimization, often favoring non-viral approaches despite their sometimes lower efficiency.
Future directions in delivery technology will likely focus on enhancing tissue specificity beyond liver tropism, improving safety profiles through novel capsid engineering or nanoparticle formulations, and developing more sophisticated control systems for temporal regulation of editing activity. The ongoing clinical validation of multiple delivery platforms, including the notable successes of LNP-based in vivo delivery and electroporation-based ex vivo approaches, provides a robust foundation for the next generation of CRISPR-based therapeutics. As these technologies evolve, the framework presented here will help researchers and therapeutic developers navigate the complex trade-offs between efficiency, specificity, safety, and manufacturability across the development continuum.
Conclusion
The successful implementation of CRISPR-Cas9 technology is fundamentally dependent on selecting the appropriate delivery method, which must be tailored to specific experimental or therapeutic contexts. Viral vectors offer high efficiency but face immunogenicity and cargo size limitations, while non-viral methods like LNPs provide improved safety profiles and redosing capabilities, as demonstrated in recent clinical trials. Critical challenges remain in achieving cell-type specificity, enhancing nuclear localization, and minimizing off-target effects. Future directions will likely focus on novel nanostructures like LNP-SNAs that show promise in boosting editing efficiency, the development of cell-specific targeting systems, and the integration of AI to optimize gRNA design and predict editing outcomes. As delivery technologies continue to evolve, they will unlock CRISPR's full potential to treat a broader range of genetic disorders and advance personalized medicine approaches.
References
- 1. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 2. Delivery Strategies of the CRISPR-Cas9 Gene-Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723556/]
- 3. 5 Reasons Why Ribonucleoproteins Are a Better ... [https://www.synthego.com/blog/crispr-plasmid-pitfalls/]
- 4. Strategies in the delivery of Cas9 ribonucleoprotein for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7738854/]
- 5. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 6. Optimizing CRISPR delivery for drug discovery [https://www.drugdiscoverynews.com/optimizing-crispr-delivery-for-drug-discovery-16487]
- 7. A modular strategy for extracellular vesicle-mediated ... [https://www.nature.com/articles/s41467-025-65995-3]
- 8. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://www.mdpi.com/1422-0067/26/9/4420]
- 9. Overcoming the Delivery Challenges in CRISPR/Cas9 ... [https://www.medsci.org/v22p3625.htm]
- 10. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 11. innovations and challenges in rAAV vector-based CRISPR ... [https://www.nature.com/articles/s41434-025-00573-2]
- 12. Optimizing viral transduction in immune cell therapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12046913/]
- 13. Lipid nanoparticle delivery of the CRISPR/Cas9 system ... [https://www.nature.com/articles/s41598-025-03671-8]
- 14. Delivering CRISPR: a review of the challenges and approaches [https://pmc.ncbi.nlm.nih.gov/articles/PMC6058482/]
- 15. CRISPOR: intuitive guide selection for CRISPR/Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6030908/]
- 16. Protocol to rapidly screen CRISPR-Cas9 gene editing ... [https://www.sciencedirect.com/science/article/pii/S2666166725003569]
- 17. Enhancing Specificity, Precision, Accessibility, Flexibility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12302564/]
- 18. Unlocking mRNA-driven CRISPR-Cas9 gene therapy via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594903/]
- 19. Recent advances in therapeutic gene-editing technologies [https://www.sciencedirect.com/science/article/pii/S152500162500200X]
- 20. Advancements in CRISPR/Cas systems for disease treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC12254762/]
- 21. Revolution of AAV in Drug Discovery: From Delivery System to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178111/]
- 22. AAV-based CRISPR-Cas9 genome editing: Challenges ... [https://www.sciencedirect.com/science/article/pii/S2468451123000739]
- 23. Customizable virus-like particles deliver CRISPR–Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12015117/]
- 24. Advancing gene editing: the role of lipid nanoparticles in ... [https://www.drugtargetreview.com/article/188056/advancing-gene-editing-the-role-of-lipid-nanoparticles-in-crispr-delivery/]
- 25. Endosomal escape and current obstacles in ionizable lipid ... [https://www.sciencedirect.com/science/article/pii/S0378517325011007]
- 26. Molecular Dynamics Simulation of Lipid Encapsulating... Nanoparticles [https://pmc.ncbi.nlm.nih.gov/articles/PMC11433737/]
- 27. Engineering of mRNA vaccine platform with reduced lipids ... [https://www.nature.com/articles/s41467-025-63965-3]
- 28. & gene delivery - Soft Matter Physics - Fakulty of Physics - LMU... LNPs [https://www.physik.lmu.de/softmatter/en/raedler-group/lnps-gene-delivery/]
- 29. Comparative Analysis of CRISPR/Cas9 Delivery Methods in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610623/]
- 30. Comparative analysis of lipid Nanoparticle-Mediated ... [https://www.sciencedirect.com/science/article/pii/S093964112400033X]
- 31. CRISPR/Cas9 systems: Delivery technologies and ... [https://www.sciencedirect.com/science/article/pii/S1818087623000818]
- 32. CRISPR This Way: Choosing Between Delivery System [https://en.vectorbuilder.com/resources/vector-academy/lessons/crispr-delivery-systems.html]
- 33. Opening a new chapter for clinical precision gene therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12290018/]
- 34. Virus-like particles: Innovative strategies for combatting ... [https://www.sciencedirect.com/science/article/pii/S2950194625001190]
- 35. Engineering ARMMs for improved intracellular delivery of ... [https://www.sciencedirect.com/science/article/pii/S2773041725000186]
- 36. Extracellular vesicle-mediated delivery of CRISPR ... [https://pubmed.ncbi.nlm.nih.gov/41017153/]
- 37. Engineering a streamlined virus-like particle for ... [https://www.nature.com/articles/s41467-025-64181-9]
- 38. Engineered virus-like particle-assembled Vegfa-targeting ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03774-5]
- 39. In vivo delivery of CRISPR-Cas9 therapeutics - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8424283/]
- 40. CRISPR Clinical Trials: A 2024 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2024/]
- 41. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 42. Peptide-enabled ribonucleoprotein delivery for CRISPR ... [https://pubmed.ncbi.nlm.nih.gov/40032999/]
- 43. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 44. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 45. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 46. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 47. Engineered circular guide RNAs enhance miniature ... [https://www.nature.com/articles/s41467-025-58367-4]
- 48. Enhanced Cellular Uptake of Compact Cas Proteins [https://pubmed.ncbi.nlm.nih.gov/41020188/]
- 49. mRNA trans-splicing dual AAV vectors for (epi)genome ... [https://www.nature.com/articles/s41467-023-42386-0]
- 50. A dual AAV system enables the Cas9-mediated correction of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4786489/]
- 51. CRISPR-Cas9 Gene Therapy: Non-Viral Delivery and Stimuli ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11820414/]
- 52. Endo/Lysosomal-Escapable Lipid Nanoparticle Platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300936/]
- 53. Advancing endosomal escape of polymeric nanoparticles [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d4mh01781a]
- 54. Exploring non-viral methods for the delivery of CRISPR-Cas ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03848-4]
- 55. Overcoming the Delivery Challenges in CRISPR/Cas9 Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434829/]
- 56. A multistep platform identifies spleen-tropic lipid nanoparticles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542943/]
- 57. Peeling back the layers of immunogenicity in Cas9-based ... [https://www.sciencedirect.com/science/article/pii/S1525001625005350]
- 58. Peeling back the layers of immunogenicity in Cas9-based ... [https://pubmed.ncbi.nlm.nih.gov/40605271/]
- 59. Rational engineering of minimally immunogenic nucleases ... [https://www.nature.com/articles/s41467-024-55522-1]
- 60. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 61. CRISPR Therapeutics Announces Positive Phase 1… [https://crisprtx.com/about-us/press-releases-and-presentations/crispr-therapeutics-announces-positive-phase-1-clinical-data-for-ctx310-demonstrating-deep-and-durable-angptl3-editing-triglyceride-and-lipid-lowering]
- 62. Phase 1 Trial of CRISPR-Cas9 Gene Editing Targeting ... [https://pubmed.ncbi.nlm.nih.gov/41211945/]
- 63. Phase 1 Trial of CRISPR-Cas9 Gene Editing Targeting ... [https://www.acc.org/Latest-in-Cardiology/Clinical-Trials/2025/11/23/20/14/CRISPR-Cas9]
- 64. CRISPR's efficiency triples with DNA-wrapped nanoparticles [https://news.northwestern.edu/stories/2025/09/crisprs-efficiency-triples-with-dna-wrapped-nanoparticles]
- 65. Nanotechnology-Based Delivery of CRISPR/Cas9 for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346122/]
- 66. New nanostructure makes CRISPR edits safer and three ... [https://www.drugtargetreview.com/news/186004/new-nanostructure-makes-crispr-edits-safer-and-three-times-faster/]
- 67. CRISPR's Efficiency Triples With Spherical Nucleic Acid ... [https://news.feinberg.northwestern.edu/2025/09/05/crisprs-efficiency-triples-with-spherical-nucleic-acid-delivery-system/]
- 68. New Nanostructure Enhances CRISPR Delivery [https://www.regmednet.com/new-nanostructure-enhances-crispr-delivery/]
- 69. Improving DNA Nanostructure Stability: A Review of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11060068/]
- 70. What Are the Limitations of CRISPR-Cas9? [https://synapse.patsnap.com/article/what-are-the-limitations-of-crispr-cas9]
- 71. Advancing gene editing therapeutics: Clinical trials and ... [https://www.sciencedirect.com/science/article/pii/S2162253125002203]
- 72. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 73. CRISPR Gene Therapy: Applications, Limitations, and ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.01387/full]
- 74. Ethical and Scientific Concerns Relating to CRISPR/Cas Gene ... [https://criticaldebateshsgj.scholasticahq.com/article/144179-ethical-and-scientific-concerns-relating-to-crispr-cas-gene-therapy]