CRISPR Genome Editing: A Foundational Guide for Research and Therapeutic Development
This article provides a comprehensive introduction to CRISPR genome editing for researchers and drug development professionals.
CRISPR Genome Editing: A Foundational Guide for Research and Therapeutic Development
Abstract
This article provides a comprehensive introduction to CRISPR genome editing for researchers and drug development professionals. It covers foundational concepts, from the core mechanisms of CRISPR-Cas9 to advanced base and prime editing systems. The guide explores diverse methodological applications in both basic research and clinical trials, addresses key troubleshooting challenges like off-target effects and delivery, and offers a comparative analysis of validation techniques. By synthesizing current research and clinical progress, this resource aims to equip new researchers with the knowledge to effectively implement and validate CRISPR technologies in their work.
The CRISPR Revolution: From Bacterial Immunity to Programmable Gene Editing
The ability to precisely modify the genome represents one of the most transformative advancements in modern biology, enabling researchers to investigate gene function, model diseases, and develop innovative therapies for genetic disorders [1]. The evolution of genome editing platforms—from early programmable nucleases to the current CRISPR-dominated landscape—has progressively democratized access to precision genetic engineering. This evolution began with protein-engineered systems like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs), which established the feasibility of targeted DNA double-strand breaks (DSBs) but required complex design processes [1] [2]. The discovery of CRISPR-Cas systems marked a revolutionary turning point, shifting the paradigm from protein-based to RNA-guided targeting and making genome editing more accessible, cost-effective, and versatile than ever before [1] [2]. This technical guide provides new researchers with a comprehensive overview of these core platforms, their mechanisms, applications, and experimental considerations within the context of contemporary biomedical research.
Historical Background of Genome Editing Techniques
Meganucleases
Meganucleases, also known as homing endonucleases, were among the earliest classes of programmable nucleases used in genome editing [2]. These naturally occurring enzymes recognize large DNA target sequences (14-40 base pairs) and induce site-specific DSBs [2]. While they exhibit high specificity and minimal off-target activity, their historical limitation has been the difficulty of reprogramming target specificity, though recent engineering advances by companies like Precision BioSciences have addressed this challenge [2].
Zinc Finger Nucleases (ZFNs)
ZFNs emerged as the first generation of programmable nucleases, combining a zinc finger DNA-binding domain with the FokI restriction endonuclease domain [2]. Each zinc finger motif recognizes a specific DNA triplet, and multiple fingers are assembled to target longer sequences [1] [2]. A significant limitation of ZFNs is their context-dependent binding, where the activity of individual fingers can be influenced by their neighbors, making design complex and often requiring extensive optimization [3]. The construction of ZFN expression plasmids for a new target could take several months, limiting their widespread adoption [2].
Transcription Activator-Like Effector Nucleases (TALENs)
TALENs represented a significant advancement in design flexibility, utilizing TALE proteins from the plant pathogen Xanthomonas [2]. Each TALE repeat recognizes a single nucleotide through repeat-variable di-residues (RVDs), with specific RVD codes (NG for T, NI for A, HD for C, and NN for G) enabling more straightforward target recognition compared to ZFNs [2]. While TALENs offered improved design simplicity and higher success rates, their large size and challenging delivery, particularly via viral vectors, remained significant limitations [2].
Mechanism of Action: A Comparative Analysis
Fundamental DNA Recognition Mechanisms
Each genome editing platform operates through distinct DNA recognition and cleavage mechanisms:
- ZFNs: Use protein-DNA interactions where zinc finger domains recognize DNA triplets. The FokI nuclease domain must dimerize to become active, requiring two ZFN monomers binding to opposite DNA strands with proper orientation and spacing [2].
- TALENs: Similarly rely on protein-DNA interactions but with a simpler one-repeat-to-one-nucleotide recognition code. Like ZFNs, TALENs also use the FokI nuclease that requires dimerization for activity [2].
- CRISPR-Cas9: Utilizes RNA-DNA base pairing where a guide RNA (gRNA) directs the Cas9 nuclease to complementary DNA sequences. The system requires a protospacer adjacent motif (PAM) sequence adjacent to the target site for recognition [2] [3].
DNA Repair Pathways
All three platforms create double-strand breaks (DSBs) that are repaired by endogenous cellular mechanisms [2]:
- Non-Homologous End Joining (NHEJ): An error-prone repair pathway that often results in small insertions or deletions (indels), frequently leading to gene knockouts [1] [2].
- Homology-Directed Repair (HDR): A precise repair mechanism that uses a DNA template to facilitate accurate gene corrections or insertions, though this pathway occurs less frequently than NHEJ [1] [2].
DNA Repair Pathways Following Genome Editing. This diagram illustrates the two primary cellular repair mechanisms activated after a double-strand break is introduced by genome editing tools. NHEJ typically results in gene knockouts, while HDR enables precise edits using a donor template.
Technical Comparison of Genome Editing Platforms
The following tables provide a comprehensive technical and practical comparison of the three major genome editing platforms, highlighting their key characteristics and relative advantages for research applications.
Table 1: Molecular Characteristics and Performance Metrics
| Feature | ZFNs | TALENs | CRISPR-Cas9 |
|---|---|---|---|
| DNA Recognition | Protein-based (Zinc fingers) | Protein-based (TALE repeats) | RNA-based (Guide RNA) |
| Nuclease | FokI | FokI | Cas9 |
| Target Specificity | High (12-18 bp per monomer) | High (14-20 bp per monomer) | Moderate to High (20 bp + PAM) |
| Recognition Code | Complex (DNA triplet per finger) | Simple (1 nucleotide per repeat) | Simple (Watson-Crick base pairing) |
| Off-Target Effects | Lower than CRISPR | Lower than CRISPR | Higher (but improving with new variants) |
| PAM Requirement | No | No | Yes (NGG for SpCas9) |
| Typical Editing Efficiency | Variable (context-dependent) | High (>90% in some studies) | High (often >70%) |
| Multiplexing Capacity | Limited | Limited | High (multiple gRNAs) |
Data compiled from [1] [2] [3]
Table 2: Practical Research Considerations
| Parameter | ZFNs | TALENs | CRISPR-Cas9 |
|---|---|---|---|
| Design Complexity | High (requires expert knowledge) | Moderate (modular but repetitive) | Low (simple gRNA design) |
| Design Timeline | ~1 month | ~1 month | Within a week |
| Cost | High | Medium | Low |
| Delivery Method | Primarily plasmid vectors | Primarily plasmid vectors | Multiple options (viral, LNP, etc.) |
| Scalability | Limited | Limited | High (ideal for high-throughput) |
| Accessibility | Low (proprietary platforms) | Moderate | High (widely accessible) |
| Time for Stable Cell Line | Months | Months | Weeks |
| Best Applications | High-precision therapeutic edits | Validated high-specificity edits | Functional genomics, screening, therapeutics |
Data compiled from [1] [2] [3]
CRISPR-Cas Systems: A Technical Revolution
Mechanism of CRISPR-Cas9
The CRISPR-Cas9 system has become the most widely utilized genome editing platform due to its straightforward design, low cost, high efficiency, and short experimental cycle [2]. The system consists of two key components: the Cas9 nuclease and a guide RNA (gRNA) that combines CRISPR RNA (crRNA) and trans-activating CRISPR RNA (tracrRNA) into a single molecule [3]. The gRNA directs Cas9 to complementary DNA sequences adjacent to a protospacer adjacent motif (PAM), which for the commonly used Streptococcus pyogenes Cas9 (SpCas9) is "NGG" [3]. Upon binding, Cas9 creates a blunt-ended double-strand break 3-4 nucleotides upstream of the PAM site [2].
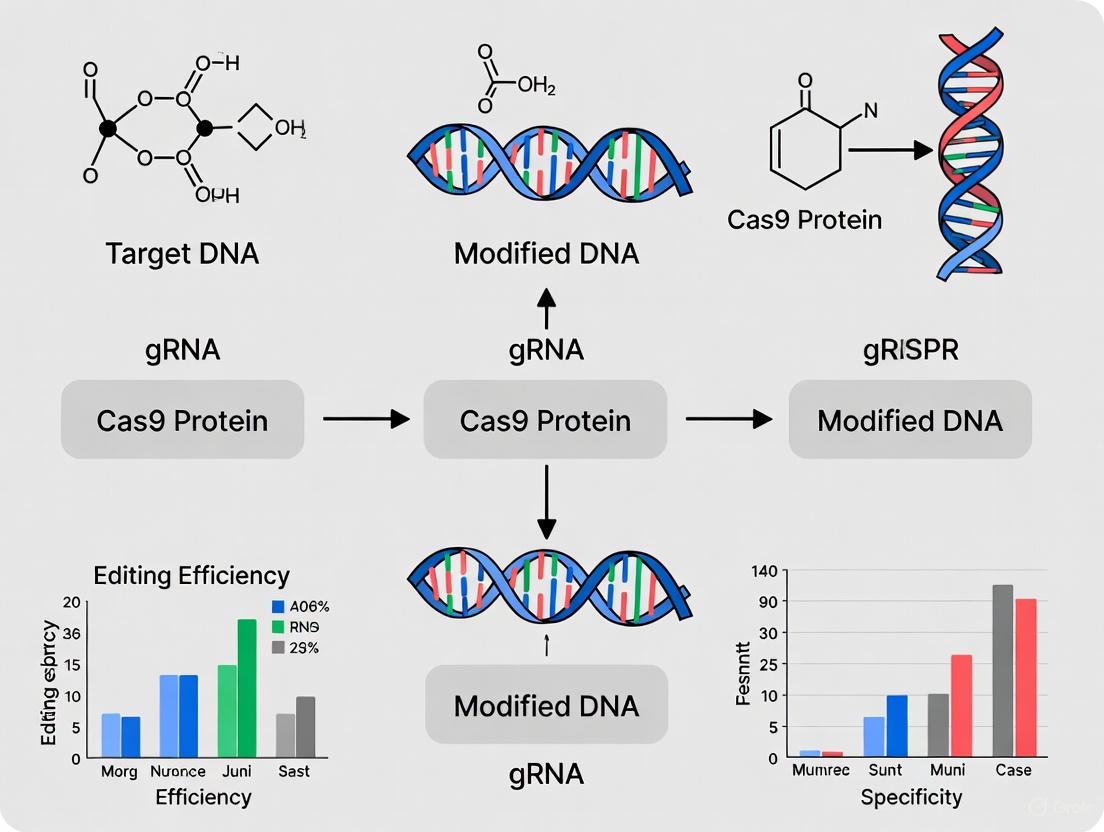
CRISPR-Cas9 Target Recognition and Cleavage. This diagram shows the CRISPR-Cas9 complex, where the guide RNA directs the Cas9 protein to a specific DNA sequence adjacent to a PAM sequence, resulting in a double-strand break.
CRISPR Screening and Functional Genomics
One of CRISPR's most significant advantages is its scalability for high-throughput functional genomics screens. CRISPR screening enables researchers to systematically knock out or activate genes across the entire genome to identify essential genes, uncover novel drug targets, and optimize combination therapy strategies [1]. Crown Bioscience and other organizations leverage CRISPR screening to accelerate drug discovery, enabling loss-of-function and gain-of-function studies at an unprecedented scale [1].
Advanced CRISPR Technologies
The CRISPR toolkit has expanded significantly beyond the standard Cas9 system:
- Base Editing: Allows single-nucleotide changes without creating DSBs, reducing off-target risks [1] [4]. Companies like Beam Therapeutics are leveraging base editing for therapeutic applications like sickle cell disease and beta-thalassemia [5].
- Prime Editing: Capable of introducing complex edits without DSBs, expanding CRISPR's therapeutic potential [1] [4]. Recent studies have successfully used prime editing to correct pathogenic mutations in inherited retinal diseases [6].
- Epigenetic Editing: Systems like those developed by Chroma Medicine (now nChroma Bio) modify gene expression without changing DNA sequences by writing or erasing epigenetic marks [5].
- Compact Cas Variants: Proteins like Cas12, Cas13, and CasΦ from companies like Mammoth Biosciences offer smaller sizes for improved delivery and new applications like RNA targeting [1] [5].
Experimental Protocols and Methodologies
General Workflow for Genome Editing Experiments
A standard genome editing experiment follows these key steps:
- Target Selection: Identify specific genomic target site considering accessibility, chromatin state, and potential off-target sites.
- Design and Synthesis: Create ZFNs/TALENs or gRNAs using appropriate design tools and algorithms.
- Delivery: Introduce editing components into target cells using appropriate methods (see Section 6.2).
- Validation: Confirm editing efficiency and specificity using sequencing and functional assays.
- Analysis: Assess phenotypic outcomes and potential off-target effects.
Delivery Methods
Efficient delivery of editing components remains a critical challenge:
- Viral Vectors: Lentiviruses and adenoviruses can package CRISPR components, though size limitations exist for larger nucleases [1].
- Lipid Nanoparticles (LNPs): Particularly effective for in vivo delivery, especially to the liver. Successfully used in clinical trials for hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) [7] [5].
- Electroporation: Effective for ex vivo editing of hematopoietic stem cells and immune cells.
- AAV Vectors: Useful for in vivo gene therapy but limited by packaging capacity.
Recent advances have demonstrated the potential for redosing with LNP-delivered CRISPR therapies, as they don't trigger the same immune responses as viral vectors [7].
Research Reagent Solutions Toolkit
The following table outlines essential reagents and their applications in genome editing research:
Table 3: Essential Research Reagents for Genome Editing
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Nucleases | SpCas9, SaCas9, FokI | Core editing enzymes that create double-strand breaks |
| Guide RNAs | Synthetic crRNA/tracrRNA, sgRNA | Target recognition molecules for CRISPR systems |
| Delivery Vehicles | Lentivirus, AAV, Lipid Nanoparticles (LNPs) | Vectors for introducing editing components into cells |
| Design Tools | CRISPR-GPT, various web tools | AI-assisted design of gRNAs and experimental planning |
| Editing Enhancers | NHEJ inhibitors, HDR enhancers | Small molecules that improve editing efficiency and precision |
| Detection Assays | T7E1, TIDE, NGS-based methods | Methods to quantify editing efficiency and off-target effects |
| Cell Culture Media | GMP-grade media, stem cell media | Specialized formulations for maintaining edited cells |
Data compiled from [1] [2] [8]
Applications and Current Landscape
Therapeutic Applications
Genome editing technologies have demonstrated remarkable success in clinical applications:
- CRISPR Therapeutics: The first FDA-approved CRISPR-based medicine, Casgevy, treats sickle cell disease and transfusion-dependent beta thalassemia [7]. Intellia Therapeutics has shown promising results with in vivo CRISPR treatments for hATTR and HAE, achieving over 90% reduction in disease-related proteins [7] [5].
- Traditional Methods: ZFNs and TALENs continue to find applications in specific therapeutic areas. Cellectis has reported promising Phase 1 results for lasme-cel, an allogeneic CAR-T therapy likely developed using TALEN-based gene editing [6].
- Novel Applications: Companies like Eligo Bioscience are pioneering microbiome editing using CRISPR to target specific bacterial populations without disrupting the overall microbiome balance [5].
Agricultural and Industrial Applications
In agriculture, genome editing technologies have been deployed to develop crops with improved yield, disease resistance, and environmental resilience [3]. CRISPR-Cas9 has emerged as the most promising tool for agricultural applications due to its scalability and user-friendly design, potentially addressing food security challenges for a growing global population [3].
Research and Drug Discovery
Beyond direct therapeutics, genome editing platforms have become indispensable tools for basic research and drug discovery. CRISPR screening enables systematic functional genomics studies, while engineered cell lines and animal models provide robust platforms for target validation and compound screening [1].
Future Directions and Innovations
The genome editing field continues to evolve rapidly with several promising developments:
- AI Integration: Tools like CRISPR-GPT from Stanford Medicine use artificial intelligence to assist researchers in designing experiments, predicting off-target effects, and troubleshooting design flaws, potentially accelerating therapeutic development [8].
- Improved Delivery Systems: Ongoing research focuses on developing novel delivery methods, including cell-specific LNPs and improved viral vectors, to expand the range of treatable tissues beyond the liver [7] [6].
- Enhanced Specificity: New engineered Cas variants with improved fidelity and reduced off-target effects are continuously being developed [1] [4].
- Expanded Applications: The combination of genome editing with other technologies like organ-on-chip models provides more clinically relevant preclinical testing platforms [6].
The evolution of genome editing platforms from ZFNs and TALENs to CRISPR systems has transformed molecular biology and therapeutic development. While traditional methods maintain relevance for specific high-precision applications requiring validated edits, CRISPR has emerged as the dominant platform due to its simplicity, cost-effectiveness, and versatility. For new researchers entering the field, understanding the comparative advantages, limitations, and appropriate applications of each platform is essential for designing successful experiments. As the technology continues to advance with improvements in specificity, delivery, and AI-assisted design, genome editing is poised to drive further innovations across biomedical research, therapeutic development, and agricultural biotechnology.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated (Cas) system is an adaptive immune mechanism found in bacteria and archaea that provides protection against invading viruses and foreign genetic material [9] [10]. This natural defense system has been repurposed as a revolutionary genome-editing technology that enables precise manipulation of DNA sequences in virtually any organism [11] [12]. The CRISPR-Cas9 system has transformed biomedical research and therapeutic development due to its simplicity, efficiency, and programmability compared to previous gene-editing tools like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) [13] [14].
At its core, the CRISPR-Cas9 system consists of two fundamental components: the Cas9 endonuclease, which creates double-strand breaks in DNA, and a guide RNA (gRNA), which directs Cas9 to a specific genomic location [13] [15]. The system functions with remarkable precision by leveraging the complementary base-pairing rules of nucleic acids, allowing researchers to target specific DNA sequences simply by redesigning the gRNA [10] [16]. This technical guide will explore the core mechanisms of CRISPR-Cas9, focusing on the structure and function of gRNA, the critical role of Protospacer Adjacent Motif (PAM) sites, and the molecular events leading to double-strand break creation and repair.
The Guide RNA (gRNA): Molecular Address for Target Recognition
Structure and Components of gRNA
The guide RNA serves as the targeting mechanism of the CRISPR-Cas9 system, providing specificity through complementary base pairing. In its engineered form for laboratory applications, the gRNA is typically implemented as a single guide RNA (sgRNA) that combines two naturally occurring RNA molecules into a single construct [15]. The sgRNA consists of:
- crRNA (CRISPR RNA) component: A 17-20 nucleotide sequence that is complementary to the target DNA region and provides targeting specificity through Watson-Crick base pairing [13] [15].
- tracrRNA (trans-activating crRNA) component: A scaffold sequence that facilitates binding to the Cas9 protein and is essential for Cas9-mediated cleavage activity [15].
- Linker loop: A synthetic component that connects the crRNA and tracrRNA into a single molecular entity in engineered sgRNAs [15].
The gRNA forms a ribonucleoprotein (RNP) complex with the Cas9 enzyme through interactions between the tracrRNA scaffold and surface-exposed, positively-charged grooves on Cas9 [13]. This binding induces a conformational change in Cas9, shifting it into an active DNA-binding configuration while leaving the spacer region of the gRNA free to interact with target DNA [13].
gRNA Design Considerations
Effective gRNA design is critical for successful CRISPR experiments, impacting both on-target efficiency and off-target effects. Key design parameters include:
- Specificity: The target sequence should be unique within the genome to minimize off-target effects [13]. Bioinformatics tools are essential for identifying specific targets.
- GC Content: Optimal GC content should range between 40-80% to ensure sufficient stability without excessive nonspecific binding [15].
- Seed Sequence: The 8-10 bases at the 3' end of the gRNA targeting sequence (adjacent to the PAM) are particularly critical for target recognition and cleavage efficiency [13].
- Length: For commonly used SpCas9, gRNA targeting sequences typically range from 17-23 nucleotides [15].
Table 1: gRNA Design Parameters and Recommendations
| Parameter | Optimal Range | Functional Significance |
|---|---|---|
| Length | 17-23 nucleotides | Balances specificity and efficiency |
| GC Content | 40-80% | Ensures appropriate stability and binding affinity |
| Seed Sequence | 8-10 bases at 3' end | Critical for initial recognition and cleavage efficiency |
| Specificity | Unique in genome | Minimizes off-target effects |
Several computational tools have been developed to facilitate optimal gRNA design, including CHOPCHOP, CRISPRscan, and Synthego's design tool, which incorporate these parameters to predict gRNA efficiency and specificity [15].
Protospacer Adjacent Motif (PAM): The Self vs. Non-Self Discriminator
PAM Recognition and Function
The Protospacer Adjacent Motif (PAM) is a short, conserved DNA sequence adjacent to the target site (protospacer) that is essential for Cas9-mediated cleavage [9] [14]. The PAM sequence plays a critical role in the natural bacterial immune system by enabling discrimination between "self" and "non-self" DNA, preventing autoimmunity by ensuring that the CRISPR locus itself is not targeted [9] [13]. The PAM is not part of the bacterial host genome but is located next to the protospacer region in invading DNA [14].
For the most commonly used Cas9 from Streptococcus pyogenes (SpCas9), the canonical PAM sequence is 5'-NGG-3', where "N" represents any nucleotide base [13] [14]. The Cas9 enzyme will not bind or cleave target DNA if this PAM sequence is not present immediately downstream of the target sequence [14]. The PAM is recognized directly by the Cas9 protein, not by the gRNA, and this recognition is essential for initiating the DNA unwinding that allows gRNA to hybridize with the target DNA [9].
PAM-Dependent Target Activation
The mechanism of PAM recognition and subsequent target activation involves several coordinated steps:
- Initial Scanning: Cas9 surveillance complexes efficiently scan DNA sequences for PAM recognition [9].
- PAM Binding: Once Cas9 binds the PAM sequence, it undergoes conformational changes that facilitate DNA unwinding [9].
- Seed Sequence Interrogation: The seed sequence near the PAM is checked for complementarity with the gRNA spacer [9].
- R-loop Formation: If seed sequence matching occurs, the gRNA continues to anneal to the target DNA, forming a triple-stranded R-loop structure [9].
- Cas9 Activation: Complete hybridization induces another conformational change in Cas9, activating its nuclease domains [13].
The stringency of PAM recognition varies among different CRISPR-Cas systems and between the adaptation and interference stages, leading to proposals to classify PAM elements as spacer acquisition motifs (SAMs) and target interference motifs (TIMs) [9].
PAM Sequences for Different Cas Enzymes
Different Cas enzymes recognize distinct PAM sequences, which determines their targeting range and applications. The following table summarizes PAM sequences for several commonly used Cas enzymes:
Table 2: PAM Sequences for Different Cas Enzymes
| Cas Enzyme | Source Organism | PAM Sequence | Notes |
|---|---|---|---|
| SpCas9 | Streptococcus pyogenes | 5'-NGG-3' | Most widely used; abundant PAM |
| SaCas9 | Staphylococcus aureus | 5'-NNGRR(N)-3' | Smaller size for viral delivery |
| Cas12a (Cpf1) | Acidaminococcus spp. | 5'-TTTV-3' | Staggered DNA cuts; simpler gRNA |
| Cas12a Ultra | Engineered | 5'-TTTN-3' | Enhanced activity; TTTT may work with reduced potency |
| AsCas12f | Axidibacillus sulfuroxidans | Varies | Compact size (one-third of SpCas9) for AAV delivery |
The PAM requirement represents a significant constraint in CRISPR targeting, inspiring the development of engineered Cas variants with altered PAM specificities, such as xCas9 (recognizes NG, GAA, and GAT), SpCas9-NG (recognizes NG), SpG (recognizes NGN), and SpRY (recognizes NRN/NYN) [13] [12].
Double-Strand Break Creation and DNA Repair Mechanisms
Molecular Mechanism of DNA Cleavage
Upon successful PAM recognition and target binding, Cas9 undergoes a final conformational change that activates its nuclease domains to create a double-strand break (DSB) in the target DNA [13]. The Cas9 enzyme contains two distinct nuclease domains:
- HNH Domain: Cleaves the DNA strand complementary to the gRNA (target strand)
- RuvC Domain: Cleaves the non-complementary DNA strand (non-target strand)
These coordinated cleavage events result in a blunt-ended DSB located approximately 3-4 nucleotides upstream of the PAM sequence [13]. The precision of this cleavage is determined by the gRNA-DNA complementarity, particularly in the seed sequence adjacent to the PAM [13].
Diagram 1: CRISPR-Cas9 Target Recognition and Cleavage Mechanism
DNA Repair Pathways
Cells employ two primary pathways to repair CRISPR-induced DSBs, each with distinct molecular mechanisms and outcomes:
Non-Homologous End Joining (NHEJ)
NHEJ is the dominant and more efficient repair pathway in most cells, particularly in non-dividing cells [13]. This pathway directly ligates the broken DNA ends without requiring a repair template, making it error-prone and frequently resulting in small insertions or deletions (indels) at the cleavage site [17] [13]. These indels can disrupt the open reading frame of the targeted gene, causing frameshift mutations and premature stop codons that effectively knock out gene function [13]. The error-prone nature of NHEJ is leveraged in knockout experiments to generate loss-of-function mutations.
Homology-Directed Repair (HDR)
HDR is a less efficient but high-fidelity repair pathway that requires a homologous DNA template to accurately repair the break [13]. This pathway is more active in dividing cells and during the S and G2 phases of the cell cycle [12]. In CRISPR applications, researchers can supply an exogenous donor DNA template with homology arms flanking the desired modification, enabling precise gene editing such as nucleotide substitutions, gene insertions, or gene corrections [17] [12].
Diagram 2: DNA Repair Pathways After CRISPR-Cas9 Cleavage
Advanced CRISPR Editing Systems
To overcome limitations of standard CRISPR-Cas9 editing, particularly the reliance on error-prone NHEJ, researchers have developed advanced engineered systems:
- Base Editing: Uses modified Cas9 (nCas9 or dCas9) fused to a deaminase enzyme to directly convert one DNA base to another (C-to-T or A-to-G) without creating DSBs [12].
- Prime Editing: Employs nCas9 fused to an engineered reverse transcriptase and a prime editing guide RNA (pegRNA) to copy edited genetic information directly into the target site, enabling precise changes without DSBs [12].
- CRISPR Interference/Activation (CRISPRi/CRISPRa): Utilizes catalytically dead Cas9 (dCas9) fused to transcriptional repressors or activators to modulate gene expression without altering DNA sequence [12].
Experimental Protocols and Methodologies
CRISPR-Cas9 Workflow for Gene Knockout
A standard protocol for generating gene knockouts using CRISPR-Cas9 involves the following key steps:
gRNA Design and Selection:
- Identify target sequences (20 nucleotides) adjacent to PAM sites (5'-NGG-3' for SpCas9) within the gene of interest
- Use design tools (CHOPCHOP, CRISPRscan, Synthego) to minimize off-target effects
- Select 2-4 gRNAs for testing to ensure at least one efficient guide
gRNA Delivery Format Selection:
- Choose between plasmid-expressed sgRNA, in vitro transcribed (IVT) sgRNA, or synthetic sgRNA based on experimental needs
- Synthetic sgRNA typically offers highest efficiency and consistency [15]
Cas9 Delivery:
- Select appropriate Cas9 variant (wildtype, high-fidelity, etc.)
- Choose delivery method: plasmid DNA, mRNA, or recombinant protein
Co-delivery of gRNA and Cas9:
- Transferd cells with gRNA and Cas9 using appropriate method (lipofection, electroporation, viral delivery)
- For RNP delivery, pre-complex purified Cas9 protein with gRNA before delivery
Validation and Analysis:
- Assess editing efficiency 48-72 hours post-delivery (genomic DNA extraction, T7E1 assay, TIDE analysis, or NGS)
- Clone edited cells and screen for homozygous knockouts
- Validate knockout at protein level (Western blot, immunofluorescence)
- Confirm phenotype through functional assays
PAM Identification Methods
Several experimental approaches have been developed to identify functional PAM sequences for various CRISPR-Cas systems:
- Plasmid Depletion Assays: A randomized DNA library is inserted adjacent to a target sequence within a plasmid that is transformed into a host with an active CRISPR-Cas system. Plasmids with inactive PAM sequences are retained and identified via next-generation sequencing [9].
- PAM-SCANR (PAM Screen Achieved by NOT-gate Repression): Uses a catalytically dead Cas9 variant (dCas9) added to a target library. Successful binding to a functional PAM represses GFP expression, enabling identification of functional PAM motifs through FACS sorting and sequencing [9].
- In Vitro Cleavage Selection: Involves cleavage of target DNA libraries with multiple PAM sequences followed by sequencing of enriched cleavage products or remaining uncleaved targets [9].
- Bioinformatic Analysis: Computational alignment of protospacers from phage genomes to identify conserved PAM elements using tools like CRISPRFinder and CRISPRTarget [9].
Research Reagent Solutions
Table 3: Essential Reagents for CRISPR-Cas9 Experiments
| Reagent Category | Specific Examples | Function & Applications |
|---|---|---|
| Cas9 Enzymes | SpCas9 (Wildtype), HiFi Cas9, eSpCas9(1.1), SpCas9-HF1, HypaCas9 | Creates DSBs; high-fidelity variants reduce off-target effects |
| Specialized Cas Variants | Cas9 nickase (Cas9n), dCas9, Base editors, Prime editors | Specific applications; nicking, gene regulation, precise editing |
| gRNA Formats | Plasmid-expressed sgRNA, IVT sgRNA, Synthetic sgRNA | Targets Cas9 to specific genomic loci; synthetic offers highest efficiency |
| Delivery Systems | Lipofection reagents, Electroporation systems, AAV vectors, Lentiviral vectors | Introduces CRISPR components into cells |
| Detection & Validation | T7E1 assay kits, Next-generation sequencing, Antibodies for Western blot | Confirms editing efficiency and functional knockout |
| Cell Culture | Selection antibiotics, Culture media, Transfection enhancers | Maintains cells and improves editing efficiency |
The core mechanism of CRISPR-Cas9—comprising gRNA-mediated targeting, PAM recognition, and DSB creation—represents a powerful technological platform that has revolutionized genetic engineering. The simplicity of reprogramming targeting specificity through gRNA design, combined with the precision of Cas9-mediated cleavage, has enabled diverse applications from basic research to clinical therapies. Understanding the molecular details of these core mechanisms is essential for researchers to design effective experiments, troubleshoot issues, and develop novel CRISPR-based applications. As CRISPR technology continues to evolve with the development of more precise editing systems and improved delivery methods, its impact on biological research and therapeutic development will undoubtedly expand, offering new opportunities to address previously intractable genetic diseases and biological questions.
The CRISPR-Cas9 system has revolutionized genetic research by providing an unprecedented ability to edit genomic DNA with precision and simplicity. This technology, derived from a bacterial adaptive immune system, functions as programmable molecular scissors that can induce double-strand breaks (DSBs) at specific locations in the genome [18] [19]. However, the CRISPR-Cas9 machinery itself does not perform the genetic modification; rather, it creates a targeted DSB that activates the cell's endogenous DNA repair mechanisms [20] [21]. The outcome of genome editing is ultimately determined by which of these cellular pathways repairs the break.
Two primary DNA repair pathways compete to repair CRISPR-induced DSBs: Non-Homologous End Joining (NHEJ) and Homology-Directed Repair (HDR) [22] [18]. These pathways have distinct mechanisms, efficiencies, and outcomes, making them suitable for different research applications. Understanding how to harness these pathways is fundamental for researchers aiming to perform specific genetic modifications, from simple gene knockouts to precise nucleotide substitutions. The strategic selection between NHEJ and HDR enables a wide range of applications, including gene function studies, disease modeling, and therapeutic development [22] [18].
DNA Repair Mechanism Fundamentals
Non-Homologous End Joining (NHEJ): The Quick Fixer
NHEJ is the cell's primary and most efficient mechanism for repairing DSBs throughout most of the cell cycle [20]. This pathway functions by directly ligating the broken DNA ends together without requiring a template. While this process is fast and efficient, its template-independent nature makes it error-prone, often resulting in small insertions or deletions (indels) at the repair site [20] [21].
The error-prone characteristic of NHEJ is precisely what makes it particularly valuable for gene knockout studies. When these indels occur within the coding sequence of a gene, they can disrupt the reading frame, leading to premature stop codons and effectively inactivating the gene [18] [20]. The efficiency of NHEJ is notably high because it is active in approximately 90% of the cell cycle and does not depend on a homologous donor template [18].
Homology-Directed Repair (HDR): The Precision Pathway
In contrast to NHEJ, HDR is a precise repair mechanism that requires a homologous DNA template to accurately repair the DSB [22] [20]. This pathway utilizes either the sister chromatid (naturally available during S and G2 phases of the cell cycle) or an exogenously supplied donor template containing homologous sequences flanking the desired edit [18] [23].
HDR's template-dependent nature allows researchers to introduce specific genetic modifications, including point mutations, sequence insertions, or gene replacements, with high precision [22] [21]. To leverage HDR for genome editing, scientists design a donor DNA template that contains the desired modification flanked by homology arms—sequences that match the regions surrounding the DSB. This template guides the repair process, resulting in the precise incorporation of the genetic change into the genome [20] [21]. However, HDR is generally less efficient than NHEJ because it is restricted to the S and G2 phases of the cell cycle where homologous DNA is naturally available [18] [23].
Table 1: Key Characteristics of NHEJ and HDR Pathways
| Characteristic | NHEJ | HDR |
|---|---|---|
| Repair Template | Not required | Required (donor DNA with homology arms) |
| Efficiency | High (active in ~90% of cell cycle) | Low (restricted to S/G2 phases) |
| Precision | Error-prone (generates indels) | Precise (faithfully copies template) |
| Primary Application | Gene knockouts | Gene knockins, precise edits |
| Key Limitation | Introduces random mutations | Low efficiency compared to NHEJ |
| Cell Cycle Dependence | Active throughout cell cycle | Primarily in S and G2 phases |
Strategic Pathway Selection for Research Goals
Application-Based Decision Framework
Choosing between NHEJ and HDR depends primarily on the specific research objective. The following guidelines help researchers align their experimental design with the appropriate DNA repair pathway:
Use NHEJ for Gene Knockouts: When the goal is to disrupt gene function through frameshift mutations or premature stop codons, NHEJ is the preferred pathway. Its high efficiency makes it ideal for creating loss-of-function mutations in various model organisms [20] [21]. For knockout experiments, researchers need Cas9 nuclease (delivered as protein or plasmid), single guide RNAs (sgRNA) complexed with Cas9, and PCR primers for edit validation [20].
Use HDR for Precise Genetic Modifications: When the research requires precise edits—including gene knockins, point mutations, or the introduction of specific sequences such as fluorescent protein tags—HDR is the necessary approach [20] [21]. Successful HDR editing requires Cas9-sgRNA complexes and a carefully designed donor template with appropriate homology arms [22].
Quantitative Comparison of Editing Outcomes
Table 2: Experimental Planning Guide for NHEJ vs. HDR Applications
| Experimental Parameter | NHEJ-Based Editing | HDR-Based Editing |
|---|---|---|
| Primary Research Goal | Gene disruption/knockout | Precise editing/knockin |
| Essential Reagents | Cas9 nuclease, sgRNA | Cas9 nuclease, sgRNA, donor template |
| Template Design | Not applicable | Critical (homology arms: 0.8-1kb for dsDNA; 30-90nt for ssODN) |
| Typical Efficiency | High (varies by cell type) | Low to moderate (varies by cell type and locus) |
| Validation Approach | INDEL detection (T7E1, TIDE, sequencing) | Specific modification confirmation (PCR, sequencing) |
| Common Challenges | Off-target effects | Low efficiency, random integration |
| Optimal Cell State | Proliferating or non-dividing cells | Actively dividing cells (S/G2 phase) |
Advanced HDR Enhancement Methodologies
Overcoming Efficiency Limitations
The naturally lower efficiency of HDR compared to NHEJ has prompted the development of sophisticated strategies to enhance precise editing outcomes. These methodologies focus on shifting the cellular repair balance toward HDR:
Cell Cycle Synchronization: Since HDR is naturally restricted to S and G2 phases, synchronizing cells to these phases can significantly improve HDR efficiency. This can be achieved through chemical treatments such as thymidine-aphidicolin block or serum starvation and refeeding [18].
NHEJ Pathway Inhibition: Suppressing key NHEJ factors through chemical inhibitors or RNA interference can reduce competition with HDR. Small molecule inhibitors targeting DNA-PKcs (e.g., NU7441, KU0060648), 53BP1, or Ligase IV have shown promise in enhancing HDR efficiency [24]. However, recent studies indicate that some NHEJ inhibitors, particularly DNA-PKcs inhibitors, may increase the risk of large structural variations and chromosomal translocations, requiring careful evaluation of this approach [25].
Engineered HDR Promoters: Genetic engineering approaches have identified and enhanced natural HDR factors. For instance, expression of an engineered RAD18 variant (e18) has been shown to stimulate CRISPR-mediated HDR by suppressing the localization of the NHEJ-promoting factor 53BP1 to DSBs [24]. Similarly, dominant-negative 53BP1 mutants and Cas9-CtIP fusions have demonstrated improved HDR outcomes across multiple cell types [24].
Donor Template Design and Delivery
Optimizing the donor template is crucial for successful HDR experiments:
Template Format Selection: Single-stranded oligodeoxynucleotides (ssODNs) are ideal for introducing point mutations or short tags, while double-stranded DNA donors (with 0.8-1kb homology arms) are better suited for larger insertions [24].
Homology Arm Length: For ssODN templates, 30-90 nucleotide homology arms typically provide optimal results, while dsDNA templates require longer homology arms (0.8-1kb) for efficient recombination [24].
Strategic Placement: Positioning the desired edit as close as possible to the Cas9 cleavage site significantly improves incorporation efficiency, as resection extends asymmetrically from the break [20].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for CRISPR Genome Editing
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Cas9 Nuclease | Creates double-strand breaks at target sites | Can be delivered as protein, mRNA, or plasmid; quality affects efficiency |
| Guide RNA (sgRNA) | Targets Cas9 to specific genomic loci | Design critical for specificity; can be synthesized or transcribed in vitro |
| Donor Template | Provides homologous sequence for HDR | Format (ssODN vs. dsDNA) depends on edit size; homology arms essential |
| NHEJ Inhibitors | Shifts repair balance toward HDR | Chemical inhibitors (e.g., SCR7) or genetic approaches (e.g., dn53BP1) |
| HDR Enhancers | Promotes homologous recombination | Engineered factors (e.g., e18, RAD52) improve precise editing efficiency |
| Delivery Vehicle | Introduces editing components into cells | Viral vectors, electroporation, lipofection, or microinjection |
Emerging Safety Considerations and Future Directions
As CRISPR technologies advance toward clinical applications, understanding and mitigating potential risks becomes increasingly important. Recent studies have revealed that CRISPR editing can induce not only small indels but also large structural variations (SVs), including chromosomal translocations and megabase-scale deletions [25]. These unintended genomic alterations raise substantial safety concerns for therapeutic applications.
Notably, some HDR-enhancing strategies, particularly those involving DNA-PKcs inhibitors, have been associated with exacerbated genomic aberrations, including increased frequencies of large deletions and chromosomal translocations [25]. These findings highlight the complex trade-offs between editing efficiency and genomic integrity that researchers must consider when designing experiments.
Future directions in the field include the development of more refined precision editing tools, such as base editors and prime editors, which can modify DNA without creating DSBs, thereby potentially reducing unwanted genomic alterations [26] [25]. Additionally, improved analytical methods that can detect large structural variations are becoming essential for comprehensive evaluation of editing outcomes [25].
Visualizing DNA Repair Pathways and Experimental Workflows
DNA Repair Pathway Selection Following CRISPR-Induced DNA Break
Experimental Workflow for Pathway Selection and Optimization
The discovery of the CRISPR-Cas9 system has revolutionized genetic engineering, enabling targeted genome modification across diverse cell types and organisms. While Cas9 facilitates gene disruption via double-strand breaks (DSBs), its reliance on error-prone repair pathways can lead to undesirable outcomes such as insertions/deletions (indels) and chromosomal rearrangements. This review details the mechanisms, applications, and methodologies of two advanced precision gene editors that overcome these limitations: base editing and prime editing. These technologies allow for precise nucleotide changes without requiring DSBs or donor DNA templates, significantly expanding the therapeutic potential of CRISPR-based technologies for correcting pathogenic genetic variants.
Traditional CRISPR-Cas9 genome editing operates by inducing a site-specific double-strand break (DSB) in the DNA, which is subsequently repaired by the cell's endogenous repair mechanisms. The two primary repair pathways are non-homologous end joining (NHEJ), an error-prone process that often results in small insertions or deletions (indels) that disrupt the target gene, and homology-directed repair (HDR), which can incorporate a donor DNA template to achieve precise edits [18]. However, the efficiency of HDR is typically low, especially in non-dividing cells, and the concurrent activity of NHEJ often results in a high frequency of indels at the target site [27].
A significant proportion of human genetic diseases are caused by single-nucleotide variants (SNVs), accounting for an estimated 58% of known pathogenic genetic variants [28]. Correcting these point mutations requires a level of precision that is challenging to achieve with standard Cas9. Furthermore, the generation of DSBs carries an inherent risk of chromosomal abnormalities and genotoxicity. These limitations have driven the development of newer, more precise editing tools that can directly rewrite genetic information without creating DSBs, namely base editing and prime editing [29] [27].
Base Editing
Mechanism of Action
Base editing is a CRISPR-based technology that directly converts one DNA base into another at a target genomic locus without making a DSB. A base editor is a fusion protein consisting of a catalytically impaired Cas protein (such as a nickase, nCas9, or dead Cas9, dCas9) and a deaminase enzyme [28] [30]. The complex is guided to a specific DNA sequence by a guide RNA (gRNA). Once bound, the Cas protein partially unwinds the DNA, creating an R-loop that exposes a single-stranded DNA region to the deaminase. The deaminase then chemically modifies a specific base within a defined "editing window" [30].
There are two primary classes of base editors:
Cytosine Base Editors (CBEs): These editors use a cytidine deaminase (e.g., APOBEC1) to convert cytosine (C) into uracil (U). The cell's DNA replication and repair machinery then interpret this U as a thymine (T), ultimately effecting a C•G to T•A base pair conversion. To prevent the cell's base excision repair (BER) pathway from reversing this change, CBEs are often fused with a uracil glycosylase inhibitor (UGI) [28] [30]. The first CBE, BE3, was developed in 2016 [28].
Adenine Base Editors (ABEs): ABEs perform an A•T to G•C conversion. Since no natural DNA adenine deaminase was known, researchers engineered one from the E. coli tRNA adenosine deaminase (TadA). This engineered TadA deaminates adenine (A) to inosine (I), which is read as guanine (G) by DNA polymerases. ABEs typically function as heterodimers, incorporating both a wild-type and an engineered TadA monomer for optimal efficiency [28] [30]. The first ABE, ABE7.10, was reported in 2017 [28].
The use of a Cas9 nickase (nCas9) that cuts the non-edited DNA strand further improves editing efficiency by directing the cellular mismatch repair system to preferentially replace the non-edited base, thereby favoring the incorporation of the new base [30].
The following diagram illustrates the core mechanism of a cytosine base editor (CBE):
Base Editing Mechanism (CBE)
Experimental Protocol for Base Editing
A typical workflow for a base editing experiment in mammalian cells is outlined below.
Step 1: gRNA Design and Cloning
- Design gRNAs so that the target base is positioned within the editing window of the base editor (typically nucleotides 4-8 for SpCas9-based editors, counting from the PAM-distal end) [28].
- Select the appropriate base editor: Choose a CBE (e.g., BE4max) for C-to-T edits or an ABE (e.g., ABE8e) for A-to-G edits, considering the specific PAM requirements of the Cas variant used.
- Clone the selected gRNA sequence into a plasmid vector that will express the gRNA in your target cells.
Step 2: Delivery of Base Editing Components
- Transfect or transduce the target cells with the base editor and gRNA constructs. Common delivery methods include:
- Plasmid Transfection: Co-transfect a plasmid expressing the base editor with a plasmid expressing the gRNA.
- mRNA/gRNA Electroporation: Deliver in vitro transcribed mRNA encoding the base editor along with synthetic gRNA via electroporation for more transient expression.
- Viral Delivery: Use lentiviral or adenoviral vectors (AdV) for harder-to-transfect cells. Adeno-associated viruses (AAVs) are challenging for full-length base editors due to packaging size constraints but can be used with dual-vector systems or smaller Cas orthologs [27].
Step 3: Analysis of Editing Outcomes
- Harvest genomic DNA from treated cells 48-72 hours post-delivery.
- Amplify the target genomic region by PCR.
- Sequence the PCR amplicons using Sanger sequencing or next-generation sequencing (NGS) to quantify editing efficiency and assess purity (the proportion of desired edits versus bystander edits within the window).
- Analyze for potential off-target effects using methods like whole-genome sequencing or targeted sequencing of sites nominated by in silico prediction tools [31].
Research Reagent Solutions for Base Editing
The table below lists essential reagents required for a base editing experiment.
| Research Reagent | Function & Description |
|---|---|
| Base Editor Plasmid | Expresses the fusion protein (e.g., nCas9-deaminase-UGI for CBE). Available from nonprofit repositories (Addgene) or commercial suppliers [28]. |
| gRNA Expression Plasmid | A vector containing the U6 promoter for expression of the sgRNA. The gRNA sequence is cloned into this plasmid. |
| Delivery Reagents | Chemical transfection reagents (e.g., lipofection), electroporation kits, or viral packaging systems (lentivirus, AdV) for introducing constructs into cells. |
| Target Cell Line | The mammalian cell line intended for editing (e.g., HEK293T, primary T cells, iPSCs). |
| PCR & NGS Reagents | Primers for amplifying the target locus, PCR master mix, and kits for preparing NGS libraries to analyze editing outcomes. |
Prime Editing
Mechanism of Action
Prime editing is a "search-and-replace" genome editing technology that can mediate all 12 possible base-to-base conversions, as well as small insertions and deletions, without requiring DSBs or donor DNA templates [32] [33]. A prime editor is a fusion protein consisting of a Cas9 nickase (H840A) and an engineered reverse transcriptase (RT) [32] [34]. The system is guided by a specialized prime editing guide RNA (pegRNA), which both specifies the target site and encodes the desired edit.
The multi-step mechanism of prime editing is as follows:
- Targeting and Nicking: The prime editor complex binds to the target DNA site as directed by the spacer sequence of the pegRNA. The Cas9 nickase nicks the DNA strand containing the PAM sequence (the "PAM strand") [34].
- Hybridization and Reverse Transcription: The 3' end of the nicked DNA strand hybridizes with the primer binding site (PBS) on the pegRNA. The reverse transcriptase then uses the RT template sequence of the pegRNA to synthesize a new DNA flap containing the desired edit(s) [32] [33].
- Flap Resolution and Incorporation: Cellular enzymes resolve the resulting DNA structure, which features a 5' flap (the original, unedited sequence) and a 3' flap (the newly synthesized, edited sequence). The cell preferentially incorporates the 3' edited flap [34].
- Repair of the Complementary Strand: The edited strand now contains the new sequence, while the complementary strand remains unedited, creating a heteroduplex. To permanently install the edit, a second nicking sgRNA can be supplied (in the PE3/PE3b systems) to nick the non-edited strand. This encourages the cell's mismatch repair system to use the edited strand as a template, resulting in a stable, fully edited DNA duplex [32] [33].
The following diagram illustrates this multi-step process:
Prime Editing Mechanism
Experimental Protocol for Prime Editing
Implementing prime editing requires careful optimization of several components. A standard protocol is described below.
Step 1: pegRNA Design and Cloning
- Design the pegRNA spacer sequence to bind the target site. The PAM sequence must be present on the strand that will be nicked.
- Design the RT template sequence to be ~10-16 nucleotides long and include the desired edit(s) in the center. The template must also include downstream homology to facilitate flap alignment.
- Design the PBS sequence to be ~8-15 nucleotides long, with a melting temperature (Tm) of approximately 30°C, to ensure efficient primer binding [33] [34].
- Clone the pegRNA sequence into an appropriate expression vector. Consider using engineered pegRNAs (epegRNAs) with 3' RNA structural motifs to enhance stability and increase editing efficiency [33].
Step 2: Delivery of Prime Editing Components
- Co-deliver the prime editor and pegRNA expression constructs into target cells. Given the large size of the PE and the pegRNA, efficient delivery is a key challenge.
- Plasmid Transfection: Suitable for easily transfected cell lines.
- mRNA/pegRNA Electroporation: Delivering PE as mRNA and pegRNA as synthetic RNA can improve efficiency and reduce off-target effects in primary cells.
- Viral Delivery: Lentiviral vectors can be used, but AAVs require splitting the system due to size constraints (e.g., using dual AAVs or smaller Cas orthologs) [34].
- For higher efficiency (PE3 system), co-deliver a second sgRNA expression construct designed to nick the non-edited strand after the initial edit is installed [32].
Step 3: Analysis and Optimization
- Analyze editing efficiency as described for base editing (PCR followed by Sanger sequencing or NGS).
- Optimize the system if efficiency is low. This can involve testing pegRNAs with different PBS lengths and RT template designs, using epegRNAs, or employing advanced PE systems like PE4 or PE5, which incorporate a dominant-negative mismatch repair protein (MLH1dn) to temporarily inhibit MMR and boost efficiency [33].
Research Reagent Solutions for Prime Editing
The table below lists essential reagents for a prime editing experiment.
| Research Reagent | Function & Description |
|---|---|
| Prime Editor Plasmid | Expresses the fusion protein (nCas9-Reverse Transcriptase). Common versions include PE2, PEmax, PE4, and PE5 [33]. |
| pegRNA Expression Plasmid | A vector for expressing the complex pegRNA. The pegRNA sequence (spacer, scaffold, PBS, RT template) is cloned into this plasmid. |
| sgRNA Plasmid (for PE3) | For the PE3 system, a second plasmid expressing a standard sgRNA to nick the non-edited strand. |
| Delivery Reagents | Electroporation systems (e.g., Neon, Amaxa) or chemical transfection reagents optimized for large mRNA/RNA or plasmid DNA. |
| Target Cell Line | The cell type for editing; efficiency can vary significantly between cell lines. |
| Sequencing & Analysis Tools | NGS platforms and bioinformatics pipelines for deep sequencing to assess precise editing outcomes and indel byproducts. |
Comparative Analysis of Advanced Editing Systems
The table below provides a direct comparison of the capabilities and characteristics of Cas9, base editing, and prime editing.
| Feature | CRISPR-Cas9 (HDR) | Base Editing | Prime Editing |
|---|---|---|---|
| DNA Cleavage | Double-strand break (DSB) | Single-strand nick (or no cut) | Single-strand nick |
| Typical Editing Outcome | Insertions, deletions (NHEJ); precise edits with donor (HDR) | Point mutations: C>G, G>A (CBE); T>C, A>G (ABE) | All 12 base substitutions, small insertions, small deletions |
| Efficiency of Precise Edit | Low (HDR typically <10%) | Moderate to high | Variable; often lower than base editing |
| DSB-Related Byproducts | High (indels, translocations) | Very low | Low |
| Donor DNA Template Required | Yes (for HDR) | No | No (the pegRNA acts as the template) |
| Editing Window / PAM Constraint | Constrained by PAM location | Constrained by editing window (~4-8 bp) and PAM | Less constrained; edits can be >30 bp from PAM |
| Bystander Edits | Not applicable | Possible (edits of same base type in window) | No (edits are specific to the RT template design) |
| Therapeutic Potential | Moderate (limited by HDR efficiency) | High for specific SNVs (therapies in clinical trials) | Very high (can address ~89% of known pathogenic SNVs) |
Base editing and prime editing represent significant leaps forward in the field of precision genome editing. By moving beyond the requirement for double-strand breaks, these technologies offer a safer and more precise means of correcting disease-causing mutations. Base editors provide a highly efficient solution for specific transition mutations, while prime editors offer unparalleled versatility in the types of edits they can introduce. Ongoing research focuses on improving the efficiency, delivery, and specificity of these tools. As these technologies continue to mature, they hold immense promise for developing transformative therapies for a wide spectrum of genetic diseases, paving the way for a new era in genetic medicine.
Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated (Cas) systems represent a revolutionary genome engineering technology derived from bacterial adaptive immune systems. These systems protect bacteria from invading viruses by storing snippets of viral DNA in their own genomes, which then serve as guides to recognize and cleave matching foreign DNA sequences upon re-exposure. Scientists have harnessed this natural system to create a programmable genome editing tool that enables precise modification of DNA sequences in virtually any organism. The core CRISPR-Cas9 system consists of two fundamental components: a Cas nuclease that functions as molecular scissors to cut DNA, and a guide RNA (gRNA) that directs the nuclease to a specific genomic target sequence. This simple yet powerful architecture has democratized genome editing, making what was once a complex, specialized technique accessible to researchers across biological disciplines.
The transformative potential of CRISPR technology extends far beyond basic research into therapeutic applications for genetic diseases. Before CRISPR, gene editing approaches like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) required researchers to design and generate custom protein pairs for every genomic target, a process that was both time-consuming and expensive. CRISPR's comparative simplicity—where changing target specificity only requires designing a new RNA guide sequence—has dramatically accelerated the pace of biological research and therapeutic development. This technical overview traces the key milestones from the initial discovery of CRISPR mechanisms to the first FDA-approved CRISPR therapy, providing new researchers with essential context for understanding this rapidly evolving field.
Historical Development of CRISPR Technology
The development of CRISPR from a curious genetic sequence to a precision genome editing tool spans several decades of international scientific discovery. This timeline highlights the key breakthroughs that enabled the current CRISPR revolution.
Table 1: Key Historical Milestones in CRISPR Development
| Year | Key Discovery | Lead Researchers | Significance |
|---|---|---|---|
| 1987 | Unusual repetitive DNA sequences observed | Japanese researchers (Osaka University) | First documented discovery of what would later be recognized as CRISPR [35] |
| 2000-2005 | CRISPR characterized as bacterial immune system | Francisco Mojica, Alexander Bolotin | Recognition of CRISPR as adaptive immunity with spacers derived from foreign DNA [36] [37] |
| 2007 | Experimental demonstration of adaptive immunity | Philippe Horvath (Danisco) | First experimental proof that CRISPR provides resistance against viruses in bacteria [36] [37] |
| 2011 | tracrRNA discovery | Emmanuelle Charpentier | Identification of trans-activating CRISPR RNA essential for Cas9 function [36] |
| 2012 | CRISPR-Cas9 as programmable gene editing system | Charpentier & Doudna; Siksnys | Biochemical characterization demonstrating reprogrammable DNA cleavage [36] [35] |
| 2013 | First eukaryotic genome editing | Feng Zhang; George Church | Adaptation of CRISPR-Cas9 for use in human and mouse cells [36] [37] |
The initial discovery phase (1987-2007) began with the identification of unusual repetitive DNA structures in prokaryotes. Francisco Mojica at the University of Alicante played a pivotal role in recognizing these sequences as a distinct class present across diverse microorganisms and hypothesizing their function in microbial immunity. Between 2005-2007, multiple research groups independently established that these CRISPR sequences indeed functioned as an adaptive immune system, with Alexander Bolotin discovering the Cas9 protein and its associated PAM sequence, and Philippe Horvath providing the first experimental demonstration in Streptococcus thermophilus.
The tool development phase (2011-2013) transformed this bacterial immunity system into a programmable genome editing technology. The critical discovery of tracrRNA by Emmanuelle Charpentier in 2011 completed our understanding of the natural Cas9 complex. In 2012, teams led by Charpentier and Jennifer Doudna, along with Virginijus Siksnys, concurrently published papers demonstrating how the system could be engineered for programmable DNA cleavage. Their work showed that the crRNA and tracrRNA could be fused into a single-guide RNA (sgRNA), dramatically simplifying the system for practical applications. The following year, teams led by Feng Zhang and George Church independently published the first demonstrations of CRISPR-Cas9 genome editing in eukaryotic cells, establishing the technology as a transformative tool for genetic research and therapeutic development.
Core CRISPR Mechanism and Methodology
Molecular Components of the CRISPR-Cas9 System
The CRISPR-Cas9 system requires two fundamental molecular components for targeted DNA modification. First, the Cas9 endonuclease serves as the executive component that creates double-strand breaks in DNA. The most commonly used Cas9 enzyme is derived from Streptococcus pyogenes (SpCas9), which contains two nuclease domains: HNH, which cleaves the DNA strand complementary to the guide RNA, and RuvC, which cleaves the non-complementary strand. Second, the guide RNA (gRNA) provides the targeting specificity through complementary base pairing. The gRNA is a chimeric RNA molecule comprising a CRISPR RNA (crRNA) component that contains the ~20 nucleotide spacer sequence complementary to the target DNA, and a trans-activating crRNA (tracrRNA) that serves as a scaffolding backbone for Cas9 binding.
A critical requirement for Cas9 recognition and cleavage is the presence of a Protospacer Adjacent Motif (PAM) sequence immediately adjacent to the target site. For SpCas9, the PAM sequence is 5'-NGG-3', where "N" represents any nucleotide. The PAM is not part of the guide RNA target sequence but is essential for Cas9 activation. Upon encountering a PAM sequence, Cas9 undergoes a conformational change that enables DNA unwinding and subsequent RNA-DNA hybridization. If the guide RNA sequence demonstrates sufficient complementarity to the target DNA, particularly in the 8-12 base "seed sequence" proximal to the PAM, Cas9 activates its nuclease domains to create a blunt-ended double-strand break approximately 3-4 nucleotides upstream of the PAM sequence.
DNA Repair Mechanisms and Editing Outcomes
The cellular response to CRISPR-induced double-strand breaks determines the final editing outcome. Cells primarily utilize two distinct DNA repair pathways:
Non-Homologous End Joining (NHEJ): This dominant repair pathway in most mammalian cells directly ligates the broken DNA ends without a template. NHEJ is error-prone, frequently resulting in small insertions or deletions (indels) at the cleavage site. When these indels occur within protein-coding sequences, they often produce frameshift mutations that disrupt the open reading frame, leading to premature stop codons and effective gene knockout. NHEJ is highly efficient and suitable for gene disruption applications.
Homology-Directed Repair (HDR): This pathway uses a homologous DNA template to precisely repair the break. By providing an exogenous donor template with homologous arms flanking the desired modification, researchers can harness HDR to introduce specific sequence changes, including point mutations, gene insertions, or reporter tags. HDR occurs at significantly lower frequencies than NHEJ and is cell cycle-dependent, primarily occurring in the S and G2 phases, making precise genome editing more challenging.
Experimental Workflow for CRISPR Genome Editing
A standard CRISPR experiment follows a systematic workflow encompassing design, editing, and analysis phases:
Design Phase: Researchers identify target genomic loci and design gRNA sequences using specialized bioinformatics tools. Optimal gRNAs demonstrate perfect complementarity to the intended target while minimizing similarity to off-target sites elsewhere in the genome. Computational algorithms help predict gRNA efficiency and specificity, with considerations for GC content, position within the gene, and absence of polymorphic nucleotides in the target sequence.
Editing Phase: The CRISPR components are delivered to target cells using appropriate methods. For most in vitro applications, plasmid DNA encoding both Cas9 and gRNA sequences is transfected into cells. For more sensitive primary cells or in vivo applications, Cas9-gRNA ribonucleoprotein (RNP) complexes can be directly delivered, reducing off-target effects and enabling faster editing. The choice of delivery method depends on cell type, efficiency requirements, and application.
Analysis Phase: Editing efficiency is validated using various molecular techniques. The T7 Endonuclease I assay or Surveyor assay detects mismatched DNA heteroduplexes formed between wild-type and edited sequences. For precise quantification of editing rates, next-generation sequencing provides the most comprehensive analysis, revealing the spectrum of induced mutations and potential off-target events.
The Path to Clinical Application
First FDA-Approved CRISPR Therapy: Casgevy
In December 2023, the U.S. Food and Drug Administration approved Casgevy (exagamglogene autotemcel), marking a historic milestone as the first CRISPR-based gene therapy to receive regulatory authorization [38]. Developed through collaboration between Vertex Pharmaceuticals and CRISPR Therapeutics, Casgevy is approved for treating sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT) in patients 12 years and older.
Casgevy employs an ex vivo approach where a patient's own hematopoietic stem cells are collected and genetically modified outside the body. Using CRISPR-Cas9, the BCL11A gene is precisely edited at its erythroid-specific enhancer region. BCL11A encodes a transcriptional repressor that normally suppresses fetal hemoglobin (HbF) production after birth. By disrupting this repressor, the edited stem cells produce elevated levels of HbF, which does not sickle and can effectively compensate for the defective adult hemoglobin in SCD patients [38].
The approval was based on compelling clinical trial results. In the pivotal trial for sickle cell disease, 29 of 31 evaluable patients (93.5%) achieved freedom from severe vaso-occlusive crises for at least 12 consecutive months during the 24-month follow-up period. All treated patients achieved successful engraftment with no instances of graft failure or rejection. The safety profile was manageable, with the most common side effects including low levels of platelets and white blood cells, mouth sores, nausea, musculoskeletal pain, abdominal pain, vomiting, febrile neutropenia, headache, and itching [38].
Table 2: Clinical Trial Results for FDA-Approved CRISPR Therapies
| Therapy | Indication | Trial Design | Efficacy Results | Common Adverse Events |
|---|---|---|---|---|
| Casgevy | Sickle Cell Disease | Single-arm, multi-center trial (44 patients) | 29/31 (93.5%) free from severe vaso-occlusive crises for ≥12 months | Thrombocytopenia, leukopenia, stomatitis, nausea, musculoskeletal pain |
| Casgevy | Transfusion-Dependent Beta Thalassemia | Single-arm, multi-center trial | Significant reduction or elimination of transfusion requirements | Similar to SCD profile |
| Lyfgenia | Sickle Cell Disease | Single-arm, 24-month multicenter study (32 patients) | 28/32 (88%) achieved complete resolution of vaso-occlusive events | Stomatitis, cytopenias, febrile neutropenia; includes boxed warning for hematologic malignancy |
Concurrently, the FDA approved Lyfgenia (lovotibeglogene autotemcel), a lentiviral vector-based gene therapy that modifies a patient's hematopoietic stem cells to produce HbAT87Q, a gene-therapy-derived hemoglobin that functions similarly to normal adult hemoglobin but with reduced sickling potential [38]. Both therapies represent significant advances in the treatment of hemoglobinopathies, offering potentially curative options for conditions that were previously managed only symptomatically.
Expanding Clinical Applications
The success of Casgevy has accelerated clinical development of CRISPR therapies across diverse disease areas. Notable advances include:
Hereditary Transthyretin Amyloidosis (hATTR): Intellia Therapeutics has pioneered the first systemic in vivo CRISPR-Cas9 therapy administered intravenously. Unlike ex vivo approaches, this treatment uses lipid nanoparticles (LNPs) to deliver CRISPR components directly to liver cells, reducing production of the misfolded transthyretin (TTR) protein that causes disease. Clinical trials demonstrated rapid, deep (∼90%), and sustained reduction in TTR protein levels with a favorable safety profile [7].
Hereditary Angioedema (HAE): Using similar LNP delivery technology, Intellia is testing a CRISPR therapy that reduces levels of kallikrein, a key mediator of inflammatory attacks in HAE. Phase I/II results showed an 86% reduction in kallikrein and significant reduction in the number of attacks, with 8 of 11 participants in the high-dose group attack-free during the 16-week study period [7].
Oncology Applications: CRISPR-based approaches are advancing cancer immunotherapy, particularly allogeneic CAR-T cell therapies. CRISPR Therapeutics has developed CTX112, an allogeneic CAR T-product targeting CD19+ B-cell malignancies, which incorporates edits designed to evade the immune system, enhance potency, and reduce T-cell exhaustion. Preliminary data show strong efficacy with a tolerable safety profile, earning the therapy RMAT (Regenerative Medicine Advanced Therapy) designation from the FDA [39].
Research Reagent Solutions
Successful CRISPR experimentation requires carefully selected molecular tools and reagents. The following table outlines essential components for designing and implementing CRISPR studies.
Table 3: Essential Research Reagents for CRISPR Experiments
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Cas Nucleases | SpCas9, SpCas9-HF1, eSpCas9, Cas12a (Cpf1) | DNA cleavage; high-fidelity variants reduce off-target effects; different PAM specificities |
| Guide RNA Vectors | U6-promoter driven sgRNA plasmids, tRNA-gRNA arrays | gRNA expression; multiplexed targeting approaches |
| Delivery Systems | Lentiviral particles, electroporation, lipid nanoparticles (LNPs) | Introduction of CRISPR components into cells; choice depends on cell type and application |
| Validation Tools | T7E1 assay, Surveyor assay, NGS platforms | Assessment of editing efficiency and specificity |
| Cell Culture Reagents | Cytokines, selection antibiotics, serum-free media | Maintenance and expansion of edited cells, particularly for stem cell applications |
The selection of appropriate Cas enzyme variants is critical for experimental success. While wild-type SpCas9 remains widely used, high-fidelity variants like HypaCas9 and eSpCas9(1.1) offer reduced off-target editing while maintaining robust on-target activity. For specialized applications, Cas12a provides alternative PAM requirements and staggered DNA cuts beneficial for certain editing approaches. Guide RNA design has been streamlined through bioinformatics platforms that predict on-target efficiency and potential off-target sites, with algorithms continually improving through machine learning approaches.
Delivery method optimization depends on the target cell type and application. Plasmid transfection works well for easily transfectable cell lines, while lentiviral transduction provides efficient delivery for difficult-to-transfect primary cells. For the highest editing efficiency with minimal off-target effects, preassembled Cas9-gRNA ribonucleoprotein (RNP) complexes delivered via electroporation have emerged as the gold standard for clinical applications. Recent advances in lipid nanoparticle (LNP) technology have enabled efficient in vivo delivery, expanding CRISPR applications to direct therapeutic interventions.
Emerging Trends and Future Directions
The CRISPR field continues to evolve rapidly with several emerging trends shaping future research and clinical applications. Artificial intelligence is playing an increasingly important role in experimental design, with tools like CRISPR-GPT—an AI copilot developed at Stanford Medicine—helping researchers generate optimized designs, analyze data, and troubleshoot experiments [8]. This AI assistance is particularly valuable for flattening the learning curve for new researchers and accelerating the therapeutic development timeline.
Delivery technologies represent another area of intense innovation. While viral vectors remain important for ex vivo applications, non-viral delivery methods—particularly lipid nanoparticles (LNPs)—have demonstrated remarkable success for in vivo therapies. The ability to administer multiple doses of LNP-encapsulated CRISPR components without triggering significant immune responses represents a significant advantage over viral delivery methods [7]. Researchers are also developing novel LNPs with tropism for organs beyond the liver, which would dramatically expand the treatable disease spectrum.
The clinical landscape for CRISPR therapies continues to broaden beyond monogenic diseases. Cardiovascular applications are showing particular promise, with therapies targeting angiopoietin-related protein 3 (ANGPTL3) for hypercholesterolemia and LPA for elevated lipoprotein(a) advancing through clinical trials [39]. These programs demonstrate the potential of CRISPR to address common polygenic conditions with significant public health impact. Additionally, the successful development of a personalized CRISPR treatment for an infant with CPS1 deficiency—from design to delivery in just six months—establishes a precedent for rapid development of bespoke therapies for ultra-rare genetic disorders [7].
Despite these promising developments, challenges remain in the CRISPR therapeutic landscape. Manufacturing complexities, reimbursement strategies for high-cost therapies, and ensuring equitable access represent significant hurdles. Additionally, the field continues to navigate appropriate safety safeguards, particularly for in vivo applications. However, the unprecedented pace of innovation in CRISPR technology suggests these challenges will likely be addressed as the field matures, potentially ushering in a new era of genetic medicine with CRISPR at its core.
CRISPR in Action: Research and Therapeutic Applications from Bench to Bedside
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated (Cas) system, originally identified as a bacterial immune mechanism, has emerged as a revolutionary tool for precision genome editing in cancer research [40]. This technology enables researchers to target specific genetic mutations that drive tumor growth and manipulate immune cell functions to enhance anticancer activity. The core mechanism involves a Cas nuclease directed by a guide RNA (gRNA) to recognize and cleave specific DNA sequences via Watson-Crick base pairing, creating double-strand breaks (DSBs) that activate cellular DNA repair pathways [25]. The system's precision, efficiency, and programmability have transformed oncology research, allowing for the functional interrogation of cancer genomes and the development of innovative therapies that were not possible with earlier gene-editing technologies like zinc-finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) [41] [42].
Cancer is fundamentally a genetic disease caused by accumulated mutations in oncogenes and tumor suppressor genes. CRISPR technology provides an unprecedented ability to model these mutations, study their functional consequences, and develop targeted interventions [43]. The application of CRISPR in oncology spans multiple domains: identifying genetic dependencies through genome-wide screens, creating precise cellular and animal models of tumorigenesis, developing engineered immune cells for immunotherapy, and directly targeting cancer-driving genes [42]. This technical guide explores the core mechanisms of CRISPR systems and their specific applications in inactivating oncogenes and enhancing cancer immunotherapies, providing both theoretical foundations and practical methodologies for researchers entering this rapidly advancing field.
Molecular Mechanisms of CRISPR-Cas Systems
Core Components and Mechanisms
The CRISPR-Cas system operates through a relatively simple yet powerful mechanism comprising two core components: the Cas nuclease and a guide RNA (gRNA). The gRNA is a synthetic RNA chimera that combines the functions of the naturally occurring crRNA (CRISPR RNA) and tracrRNA (trans-activating crRNA) [42]. The crRNA segment contains a 20-base pair spacer sequence that is complementary to the target DNA, enabling precise recognition through base pairing, while the tracrRNA serves as a scaffold that facilitates the binding of the crRNA to the Cas protein [40]. The Cas nuclease-gRNA complex scans the genome for protospacer adjacent motifs (PAMs), short DNA sequences adjacent to the target site that are essential for recognition. Once the complex identifies a matching sequence with the correct PAM, the Cas nuclease induces a double-strand break (DSB) in the DNA [25].
The cellular response to these DSBs activates one of two primary DNA repair pathways: non-homologous end joining (NHEJ) or homology-directed repair (HDR). NHEJ is an error-prone process that often results in small insertions or deletions (indels) at the cleavage site, which can effectively knockout gene function when these mutations disrupt the reading frame. HDR, while less frequent in human cells, allows for precise gene modifications when a DNA repair template is provided [25]. The choice between these pathways has significant implications for cancer research applications, with NHEJ being predominantly exploited for gene knockouts and HDR enabling precise sequence modifications.
Major CRISPR Systems and Their Applications
Several CRISPR systems with distinct properties have been harnessed for cancer research, each offering unique advantages for specific applications. The following table summarizes the key characteristics of the major CRISPR systems used in oncology:
Table 1: Major CRISPR Systems and Their Applications in Cancer Research
| System | Target | PAM Requirement | Key Activities | Primary Research Applications |
|---|---|---|---|---|
| Cas9 | DNA | 5'-NGG-3' | DSB creation, cis-cleavage | Gene knockout, activation, repression via defective Cas9 (dCas9) [40] [43] |
| Cas12a | DNA | 5'-TTTN-3' | DSB creation, trans-cleavage of ssDNA | Multiplexed editing, diagnostic applications [40] [42] |
| Cas13 | RNA | Non-specific | trans-cleavage of ssRNA | RNA targeting, knockdown, base editing [40] [42] |
| Base Editors | DNA | Varies by Cas | Chemical conversion of bases without DSBs | Point mutation correction, SNP modeling [44] [45] |
| Prime Editors | DNA | Varies by Cas | Reverse transcription of edited sequence | Precise gene editing without DSBs [45] |
The trans-cleavage activity of Cas12 and Cas13 systems has been particularly valuable for diagnostic applications, enabling the detection of specific cancer-associated mutations with exceptional sensitivity [40]. Meanwhile, newer base editing and prime editing technologies offer more precise genetic modifications without creating double-strand breaks, potentially reducing unwanted genomic consequences [45].
CRISPR Strategies for Oncogene Inactivation
Mechanism of Oncogene Inactivation
Oncogenes are normal cellular genes that, when mutated or overexpressed, drive tumor development and progression. CRISPR-based inactivation of oncogenes typically exploits the error-prone NHEJ pathway to introduce frameshift mutations that disrupt gene function. The process begins with the identification of critical exonic regions within the target oncogene. Researchers design gRNAs with spacer sequences complementary to these regions, ensuring high on-target efficiency and minimal off-target activity through careful bioinformatic analysis [43]. Upon delivery into cancer cells, the Cas nuclease (most commonly Cas9) induces DSBs at the target site, triggering NHEJ repair that results in small insertions or deletions. When these indels disrupt the reading frame or critical protein domains, they effectively knockout oncogene function [43].
This approach has been successfully applied to numerous oncogenes across different cancer types. For example, CRISPR-mediated inactivation of the MYC oncogene has demonstrated significant reduction in tumor growth in lymphoma models [43]. Similarly, targeting mutant KRAS alleles, which are driving oncogenes in pancreatic, colorectal, and lung cancers, has shown promising antitumor effects in preclinical studies. The strategy is particularly valuable for oncogenes that are currently "undruggable" by conventional small molecules or antibodies [42].
Experimental Protocol for Oncogene Inactivation
A detailed step-by-step protocol for CRISPR-mediated oncogene inactivation:
Target Selection and gRNA Design: Identify critical exonic regions in the target oncogene using domain mapping and functional annotation. Design 3-5 gRNAs targeting each region using established algorithms (e.g., CRISPRscan, ChopChop). Prioritize gRNAs with high on-target and low off-target scores [43].
Vector Construction: Clone selected gRNA sequences into appropriate CRISPR plasmids (e.g., lentiCRISPRv2, pXPR系列). Verify sequences by Sanger sequencing. For in vivo applications, consider using all-in-one vectors expressing both Cas9 and gRNAs [42].
Delivery System Optimization: For in vitro studies, use lentiviral transduction with appropriate controls (non-targeting gRNAs). Determine viral titer and multiplicity of infection (MOI) to achieve optimal infection efficiency with minimal toxicity. For in vivo delivery, optimize lipid nanoparticles (LNPs) or adeno-associated virus (AAV) vectors based on target tissue tropism [7] [45].
Validation of Editing Efficiency: 48-72 hours post-transduction, harvest cells and extract genomic DNA. Use T7E1 assay or TIDE analysis for initial efficiency assessment. For precise quantification, perform amplicon sequencing of the target region. Calculate indel percentage and characterize specific mutations [43].
Functional Validation: Evaluate oncogene knockdown at protein level by Western blot or flow cytometry. Assess functional consequences using cell proliferation assays (MTT, CellTiter-Glo), colony formation assays, and apoptosis detection (Annexin V staining) [43].
Off-Target Assessment: Perform genome-wide off-target analysis using GUIDE-seq or CIRCLE-seq. Validate potential off-target sites by targeted sequencing. Include appropriate controls to distinguish specific from nonspecific effects [25].
The following diagram illustrates the experimental workflow for CRISPR-mediated oncogene inactivation:
CRISPR-Enhanced Immunotherapies
Engineering CAR-T Cells with CRISPR
Chimeric antigen receptor (CAR) T-cell therapy has demonstrated remarkable success in treating hematological malignancies, but limitations including T-cell exhaustion, fratricide, and limited persistence have hindered its efficacy, particularly in solid tumors. CRISPR technology has emerged as a powerful approach to overcome these challenges by genetically enhancing CAR-T cells [44] [43]. The CELLFIE platform represents a comprehensive CRISPR screening system for identifying gene knockouts that enhance CAR-T cell function across multiple clinical objectives, including proliferation, target cell recognition, activation, apoptosis resistance, and exhaustion mitigation [44].
Genome-wide CRISPR screens in primary human CAR-T cells have identified several gene knockouts that significantly enhance antitumor activity. Among the most notable discoveries is RHOG knockout, which functions as a potent CAR-T cell enhancer both individually and in combination with FAS knockout [44]. RHOG, a member of the Rho family GTPases, normally regulates T-cell receptor signaling and actin cytoskeleton reorganization. Surprisingly, its deletion enhances CAR-T cell function, demonstrating that evolutionary optimizations for natural T cells may not always align with therapeutic requirements for engineered CAR-T cells [44]. Similarly, knocking out PRDM1, which encodes a transcription factor that drives T-cell exhaustion, has shown significant improvements in CAR-T cell persistence and function [44].
Experimental Protocol for CAR-T Cell Engineering
A detailed methodology for CRISPR-enhanced CAR-T cell generation:
T-Cell Isolation and Activation: Isolate primary human T-cells from donor blood using Ficoll density gradient centrifugation and negative selection kits. Activate cells using anti-CD3/CD28 beads or antibodies for 24-48 hours [44].
CRISPR Component Delivery: Electroporate activated T-cells with Cas9 mRNA (2-5 μg/10^6 cells) and synthetic gRNAs (1-2 μg/10^6 cells) targeting immunomodulatory genes (e.g., RHOG, FAS, PDCD1). Alternatively, use lentiviral vectors encoding both CAR and gRNAs for integrated delivery [44].
CAR Transduction: Transduce edited T-cells with lentiviral vectors encoding CAR constructs (typically 2nd or 3rd generation CARs with CD28 or 4-1BB costimulatory domains). Determine optimal multiplicity of infection (MOI) for maximum CAR expression with minimal toxicity [44] [43].
Expansion and Phenotyping: Expand CAR-T cells in IL-2 or IL-7/IL-15 supplemented media for 10-14 days. Monitor cell growth and phenotype using flow cytometry for CAR expression (via detection tags), T-cell markers (CD3, CD4, CD8), and memory subsets (CD45RA, CD62L, CCR7) [44].
Functional Assays: Evaluate in vitro cytotoxicity against target cancer cells using real-time cell analysis (e.g., xCelligence) or flow cytometry-based killing assays. Measure cytokine production (IFN-γ, IL-2, TNF-α) upon tumor antigen exposure using ELISA or Luminex [44] [43].
In Vivo Validation: Utilize immunodeficient mouse models (e.g., NSG) engrafted with human cancer cells (1-5 × 10^6 cells) via IV or subcutaneous injection. Administer CAR-T cells (5-10 × 10^6 cells/mouse) and monitor tumor growth by bioluminescence imaging or caliper measurements. Assess T-cell persistence and exhaustion markers in blood and tumor tissues over time [44].
The following diagram illustrates the signaling pathways modified in CRISPR-enhanced CAR-T cells:
Advanced Research Applications and Tools
High-Content CRISPR Screening Platforms
The integration of CRISPR screening with multi-parametric readouts has dramatically advanced the discovery of genetic modifiers in cancer biology. The CELLFIE platform exemplifies this approach, enabling genome-wide CRISPR screens in primary human CAR-T cells with readouts capturing key aspects of T-cell function, including proliferation, activation, apoptosis, and exhaustion [44]. This system utilizes the CROP-seq-CAR vector, which co-delivers sequences for the CAR and gRNA with a single lentivirus, supporting high CAR expression while enabling sequencing-based tracking of gRNA-encoded perturbations [44].
Recent advances have extended CRISPR screening to in vivo contexts through adapted CROP-seq methods in xenograft models of human leukemia, allowing for the identification of gene knockouts that enhance CAR-T cell efficacy in physiologically relevant environments [44]. These screens have revealed context-specific genetic dependencies that differ markedly between in vitro and in vivo conditions, highlighting the importance of model selection in functional genomics. The platform also supports combinatorial CRISPR screens to identify synergistic gene pairs and saturation base-editing screens to characterize functional variants, providing a comprehensive toolkit for immune cell engineering [44].
Research Reagent Solutions
Table 2: Essential Research Reagents for CRISPR Oncology Applications
| Reagent Category | Specific Examples | Key Functions | Application Notes |
|---|---|---|---|
| CRISPR Editors | Cas9 mRNA, HiFi Cas9, Base editors (ABEmax, AncBE4max), Prime editors | Core editing components; introduce genetic modifications | HiFi Cas9 reduces off-target effects; Base editors enable precise nucleotide changes without DSBs [44] [45] |
| Delivery Systems | Lentiviral vectors (CROP-seq-CAR), Lipid nanoparticles (LNPs), AAV vectors | Deliver CRISPR components into target cells | LNPs preferred for in vivo delivery; Lentiviral vectors provide stable integration for screening [7] [44] |
| gRNA Libraries | Brunello genome-wide library, Custom focused libraries | Enable large-scale genetic screens | Brunello library provides high coverage of human genome; Custom libraries target specific gene families [44] |
| Detection Tools | GUIDE-seq, CIRCLE-seq, Amplicon sequencing | Assess editing efficiency and specificity | GUIDE-seq provides genome-wide off-target profiling; Amplicon sequencing quantifies indel frequency [25] |
| Cell Culture Reagents | Anti-CD3/CD28 beads, IL-2, IL-7, IL-15 | Support T-cell activation and expansion | Cytokine combinations influence T-cell differentiation toward memory or effector phenotypes [44] |
Clinical Translation and Safety Considerations
Current Clinical Landscape
The translation of CRISPR-based oncology therapies from preclinical research to clinical application has accelerated dramatically in recent years. As of 2025, there are over 100 ongoing clinical trials evaluating CRISPR-based cancer therapies, spanning multiple modalities including engineered immune cells, direct in vivo gene editing, and combination approaches [7] [45]. Notable examples include Intellia Therapeutics' phase I trial of nexiguran ziclumeran for hereditary ATTR amyloidosis, which achieved sustained 90-92% reductions in disease-causing TTR protein over 24 months, demonstrating the potential for long-lasting effects from CRISPR interventions [45]. In the cancer immunotherapy domain, BRL Medicine's BRL-201, a non-viral PD1-integrated CAR-T therapy engineered using CRISPR-Cas9 to insert an anti-CD19 CAR into the PD1 locus, has maintained a lymphoma patient cancer-free for over five years with no lasting adverse effects [45].
The clinical landscape continues to expand with novel approaches entering trials. KSQ Therapeutics recently dosed the first patient in a Phase 1/2 trial of KSQ-004EX, a CRISPR-Cas9-engineered tumor-infiltrating lymphocyte (TIL) therapy that inactivates SOCS1 and Regnase-1, genes identified via CRISPRomics screening as limiting TIL function [46]. Similarly, YolTech Therapeutics is advancing YOLT-101, a base-editing therapy for heterozygous familial hypercholesterolemia (HeFH), representing the first in vivo base-editing candidate cleared for trials in both China and the US [46].
Safety Considerations and Risk Mitigation
While CRISPR technology holds tremendous therapeutic potential, comprehensive safety assessment remains paramount for clinical translation. Recent studies have revealed that beyond well-documented concerns about off-target mutagenesis, CRISPR editing can induce large structural variations (SVs), including chromosomal translocations and megabase-scale deletions [25]. These undervalued genomic alterations raise substantial safety concerns, particularly when editing occurs in hematopoietic stem cells (HSCs) or other long-lived populations where oncogenic transformations could have severe consequences.
Several strategies have been developed to mitigate these risks:
High-Fidelity Cas Variants: Engineered Cas9 variants with enhanced specificity (e.g., HiFi Cas9) significantly reduce off-target activity while maintaining robust on-target editing [25].
Alternative Editing Platforms: Base editors and prime editors enable precise genetic modifications without creating double-strand breaks, substantially reducing the risk of large structural variations [45].
Improved Delivery Systems: Lipid nanoparticles (LNPs) have demonstrated favorable safety profiles compared to viral vectors, with reduced immunogenicity and the potential for redosing without triggering significant immune responses [7].
Advanced Analytical Methods: Techniques like CAST-Seq and LAM-HTGTS enable comprehensive detection of structural variations and chromosomal rearrangements, providing more complete safety profiles during preclinical development [25].
The field continues to evolve with a growing emphasis on balancing editing efficiency with precision, recognizing that for many therapeutic applications, even moderate editing levels may suffice when coupled with effective selection or functional advantages for corrected cells [25].
Future Perspectives and Emerging Technologies
The integration of artificial intelligence with CRISPR technology represents one of the most promising directions for advancing oncology applications. Tools like CRISPR-GPT, an AI agent developed at Stanford Medicine, accelerate experimental design and troubleshooting by leveraging years of published data to hone CRISPR strategies and predict potential pitfalls [8]. This AI copilot approach has demonstrated the ability to flatten CRISPR's steep learning curve, enabling researchers with limited experience to successfully design and execute complex editing experiments on their first attempt [8]. As these systems evolve, they are expected to dramatically accelerate the optimization of gRNA designs, prediction of editing outcomes, and identification of novel therapeutic targets.
Emerging delivery technologies also promise to expand the therapeutic reach of CRISPR oncology applications. Companies like Aera Therapeutics are developing protein nanoparticle systems based on naturally occurring human proteins that can package and deliver genetic therapies beyond the current limitation of primarily liver applications [45]. Similarly, advances in virus-like particles and novel capsid designs are enabling more efficient in vivo delivery to diverse tissues, potentially opening solid tumors to more effective CRISPR-based interventions [45] [46].
The continued refinement of CRISPR tools, including more compact Cas proteins with relaxed PAM requirements, enhanced base editors with improved product purity, and prime editors with higher efficiency, will further expand the therapeutic landscape [45]. As these technologies mature, combined with increasingly sophisticated delivery systems and AI-driven design tools, CRISPR-based approaches are poised to transform oncology research and clinical practice, potentially enabling the development of personalized genetic medicines for cancer patients with unprecedented speed and precision.
The treatment of monogenic blood disorders has been revolutionized by the advent of CRISPR-Cas9 genome editing technology. Sickle cell disease (SCD) and beta-thalassemia, both caused by mutations in the β-globin gene (HBB), represent the most advanced success stories in clinical application of CRISPR therapies. Two primary strategic approaches have demonstrated remarkable efficacy: the direct correction of the disease-causing mutation in the HBB gene and the indirect approach of reactivating fetal hemoglobin (HbF) by targeting repressor genes such as BCL11A [47] [48].
The first CRISPR-based therapy, Casgevy (exagamglogene autotemcel, or exa-cel), received FDA approval in late 2023 for patients aged 12 years and older with severe SCD or transfusion-dependent beta-thalassemia (TDT) [7] [49]. This therapy employs an ex vivo approach where a patient's own hematopoietic stem cells (HSCs) are collected, edited outside the body using CRISPR-Cas9 to disrupt the BCL11A gene, and then reinfused into the patient [47] [50]. This process leads to sustained production of fetal hemoglobin, which compensates for the defective adult hemoglobin, thereby alleviating disease symptoms [51] [49].
Table 1: Comparison of CRISPR Therapeutic Approaches for Hemoglobinopathies
| Feature | Direct HBB Correction | BCL11A Targeted Disruption (Casgevy) |
|---|---|---|
| Target | β-globin gene (HBB) [47] | BCL11A enhancer region [51] |
| Mechanism | Gene knock-in via HDR to correct point mutation [47] | Gene knockout to disrupt enhancer function [51] |
| Outcome | Production of functional adult hemoglobin [47] | Reactivation of fetal hemoglobin (HbF) [51] [47] |
| Development Status | Preclinical and early-stage trials [47] | FDA-approved (2023) [7] [49] |
| Technical Challenge | Requires high-efficiency HDR [47] | Relies on NHEJ pathway [51] |
Molecular Mechanisms of Action
BCL11A Disruption and Chromatin Architecture
Recent research has elucidated the precise molecular mechanism through which Casgevy achieves its therapeutic effect. The BCL11A gene encodes a transcriptional repressor that normally silences fetal hemoglobin expression during the transition from fetal to adult development [51]. CRISPR-Cas9 targets a specific enhancer region of BCL11A that is critical for its expression in erythroid cells.
The enhancer forms a specific three-dimensional chromatin "rosette" structure that maintains high-level BCL11A expression by facilitating multiple contacts with critical regulatory elements [51]. When CRISPR-Cas9 introduces a double-strand break in this enhancer, it disrupts this chromatin architecture, allowing repressive proteins to access and silence the BCL11A gene [51]. The subsequent reduction in BCL11A protein levels de-represses fetal hemoglobin genes, leading to robust HbF production that compensates for the defective adult hemoglobin in SCD and beta-thalassemia [51].
Emerging Alternative Approaches
Beyond BCL11A disruption, several advanced genome editing strategies are under investigation:
- Base Editing: Converts the sickle cell mutation (GTG) to a non-pathogenic Makassar β-globin variant (GCG) without double-strand breaks, offering a potentially safer alternative [47] [48].
- Prime Editing: Enables precise correction of the HBB mutation without donor DNA templates, supporting all 12 possible base-to-base conversions [48].
- Epigenetic Editing: Uses catalytically inactive Cas9 (dCas9) fused to transcriptional regulators to modulate gene expression without altering DNA sequence [48].
- Enhancer RNA Targeting: Emerging research shows that targeting enhancer-derived RNAs with antisense oligonucleotides can achieve similar BCL11A silencing without permanent genome modification [51].
The following diagram illustrates the mechanistic basis of the BCL11A targeted approach:
Figure 1: Mechanism of BCL11A Targeting by CRISPR. Disrupting the enhancer prevents formation of the chromatin rosette structure needed for BCL11A expression, leading to fetal hemoglobin reactivation.
Clinical Trial Outcomes and Efficacy Data
Casgevy (exa-cel) Clinical Performance
The CLIMB-SCD-121 and CLIMB-THAL-111 trials demonstrated transformative results for patients with severe hemoglobinopathies. Participants showed robust and sustained improvements in both clinical parameters and quality of life measures [49].
Table 2: Clinical Efficacy Outcomes from Casgevy Trials
| Parameter | Sickle Cell Disease (SCD) | Transfusion-Dependent Beta-Thalassemia (TDT) |
|---|---|---|
| Patients Evaluated | 42 adolescents and adults [49] | 54 adolescents and adults [49] |
| Follow-up Duration | Median 33.6 months [49] | Median 38.4 months [49] |
| HbF Increase | Significant elevation sustained >2 years [7] | Significant elevation sustained >2 years [7] |
| Vaso-occlusive Crises (SCD) | Resolution in majority of patients [49] | Not applicable |
| Transfusion Independence (TDT) | Not applicable | Achieved in majority of patients [49] |
| Quality of Life Improvement | Clinically meaningful improvements across physical, social, emotional domains [49] | Clinically meaningful improvements in overall health [49] |
In Vivo CRISPR Therapy Advancements
Beyond ex vivo approaches, recent clinical advances have demonstrated the feasibility of in vivo CRISPR therapies. A landmark case reported in 2025 involved an infant with CPS1 deficiency who received a personalized in vivo CRISPR therapy developed and delivered in just six months [7]. The treatment used lipid nanoparticles (LNPs) for delivery and was administered via IV infusion, with the patient safely receiving multiple doses to increase editing efficiency [7].
Similarly, Intellia Therapeutics reported phase I results for hereditary transthyretin amyloidosis (hATTR) using LNP-delivered CRISPR, showing ~90% reduction in disease-related protein levels sustained over two years [7]. These successes demonstrate the expanding potential of in vivo genome editing for monogenic disorders.
Detailed Experimental Protocol
Ex Vivo Cell Processing for Casgevy
The manufacturing process for autologous CRISPR-edited hematopoietic stem cell therapy involves multiple precisely controlled steps:
HSC Collection: Hematopoietic stem cells are collected from the patient via apheresis after mobilization with granulocyte colony-stimulating factor (G-CSF) [50].
Cell Processing and Activation: Cells are processed to enrich for CD34+ hematopoietic stem/progenitor cells and activated for editing [50].
CRISPR Electroporation: Cells are transfected with CRISPR-Cas9 components targeting the BCL11A enhancer region via electroporation [50]. The specific guide RNA sequence is designed to minimize off-target effects while maximizing on-target efficiency.
Quality Control Testing: Edited cells undergo rigorous quality assessment, including:
- Determination of editing efficiency at the target locus
- Evaluation of viability and cell number
- Sterility testing for microbial contamination
- Off-target editing assessment in predicted off-target sites
Patient Conditioning: Patients receive myeloablative conditioning with busulfan to create marrow niche space for the edited cells [50].
Cell Reinfusion: The CRISPR-edited CD34+ cells are infused back into the patient via intravenous infusion [50].
Engraftment Monitoring: Patients are monitored closely for neutrophil and platelet recovery, typically occurring within 2-4 weeks post-infusion [50].
The following workflow diagram summarizes the key steps in the therapeutic development process:
Figure 2: Ex Vivo Gene Therapy Workflow. Key steps from cell collection through patient monitoring.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for CRISPR-Based Hemoglobinopathy Research
| Reagent/Category | Function | Examples/Specifications |
|---|---|---|
| CRISPR-Cas9 System | Target DNA cleavage | SpCas9, high-fidelity variants [52] |
| Guide RNA Design | Target specificity | Designed to minimize off-target effects [8] |
| Delivery Vehicles | Cellular delivery | Lentiviral vectors, LNPs, electroporation systems [7] [48] |
| HSC Culture Media | Cell maintenance | Serum-free media with cytokine cocktails [50] |
| Flow Cytometry | Cell analysis | CD34+ selection, HbF detection [49] |
| Anti-CRISPR Proteins | Safety control | AcrIIA4 family proteins for Cas9 inhibition [53] |
| gRNA Synthesis Kits | Guide production | In vitro transcription or synthetic oligo kits [8] |
Emerging Technologies and Future Directions
AI-Driven CRISPR Design
Artificial intelligence is revolutionizing CRISPR therapeutic development. Large language models like ProGen2 are now generating novel CRISPR-Cas proteins with optimal properties for gene editing [52]. The OpenCRISPR-1 system, designed entirely by AI, demonstrates comparable or improved activity and specificity relative to natural Cas9 despite being 400 mutations away in sequence [52].
Additionally, AI tools like CRISPR-GPT serve as experimental "copilots," helping researchers design experiments, predict off-target effects, and troubleshoot designs [8]. This technology significantly reduces the trial-and-error period typically required for CRISPR experiment optimization, potentially accelerating therapeutic development from years to months [8].
Enhanced Safety Systems
Improving CRISPR safety remains a critical research focus. Recent advances include:
- Anti-CRISPR Technologies: The LFN-Acr/PA system uses a protein-based delivery approach to introduce anti-CRISPR proteins into human cells, rapidly shutting down Cas9 activity after editing is complete and reducing off-target effects by up to 40% [53].
- Novel Delivery Systems: Lipid nanoparticles (LNPs) show particular promise for in vivo delivery, with natural affinity for the liver and reduced immunogenicity compared to viral vectors [7].
- Advanced Editing Platforms: Base editors and prime editors offer more precise genetic modifications without double-strand breaks, potentially improving the safety profile of future therapies [48].
The clinical success of CRISPR-based therapies for sickle cell disease and beta-thalassemia represents a paradigm shift in the treatment of monogenic disorders. The approval of Casgevy validates both the scientific approach of BCL11A targeting and the broader potential of genome editing as a therapeutic modality. Ongoing advances in delivery systems, AI-assisted design, and safety controls continue to address the challenges of efficiency, specificity, and accessibility. As these technologies mature, they promise to expand the reach of CRISPR medicine to address a broader spectrum of genetic disorders with increasing precision and safety.
The therapeutic application of CRISPR-Cas9 genome editing fundamentally depends on the efficient delivery of its molecular components—typically the Cas nuclease and a guide RNA (gRNA)—into the nucleus of target cells. The choice between in vivo and ex vivo editing strategies directly dictates the available delivery options, each with distinct advantages and limitations [54]. In vivo delivery involves administering the CRISPR components directly into the patient's body, requiring sophisticated vectors to protect the payload and target the correct tissues. In contrast, ex vivo editing involves extracting cells from the patient, genetically modifying them in a controlled laboratory setting, and then reinfusing the edited cells back into the patient [55]. The delivery modality not only influences editing efficiency but also has critical implications for safety, immunogenicity, and the potential for off-target effects [56] [57]. This guide provides a technical comparison of the primary delivery systems—viral vectors and lipid nanoparticles (LNPs)—within the context of these two overarching strategies, providing new researchers with a foundation for selecting appropriate methodologies for their therapeutic goals.
Core Delivery Technologies
Viral Vector Delivery Systems
Viral vectors are engineered viruses that have been modified to deliver therapeutic genetic material while lacking the ability to cause disease. They are among the most widely used delivery vehicles in gene therapy and genome editing.
- Adeno-Associated Viruses (AAVs): AAVs are small, non-pathogenic viruses with a favorable safety profile, making them a leading candidate for in vivo CRISPR delivery [58] [56]. Their key advantage is their ability to transduce both dividing and non-dividing cells and mediate long-term transgene expression from episomal DNA. A significant limitation is their constrained packaging capacity of approximately 4.7 kb, which is insufficient for the standard Streptococcus pyogenes Cas9 (SpCas9) and its gRNA expressed from a single vector [58] [54]. Innovative strategies to overcome this include:
- Compact Cas Orthologs: Using smaller Cas proteins, such as those from Staphylococcus aureus (SaCas9) or Campylobacter jejuni (CjCas9) [58].
- Dual-Vector Systems: Splitting the Cas9 and gRNA expression cassettes across two separate AAV vectors that co-infect the same cell [58].
- Novel Effectors: Employing even smaller, ancestral nucleases like IscB and TnpB, which offer enhanced compatibility with AAV packaging constraints [58].
- Lentiviral Vectors (LVs): LVs are RNA viruses that integrate their genetic payload into the host genome, enabling persistent transgene expression. This makes them particularly suited for ex vivo applications, such as the engineering of T cells or hematopoietic stem cells (HSPCs) [59] [55]. A primary safety concern with LVs is the risk of insertional mutagenesis, where integration disrupts a tumor suppressor gene or activates an oncogene [59] [56]. The development of self-inactivating (SIN) vectors has helped mitigate this risk.
- Adenoviral Vectors (AdVs): AdVs have a large packaging capacity (up to 36 kb), enabling them to deliver full-length CRISPR-Cas9 systems and donor DNA templates in a single vector [56]. Similar to AAVs, they remain episomal, avoiding the risk of insertional mutagenesis. However, they often elicit strong immune responses, which can lead to rapid clearance of the vector and potential toxicity, limiting their use in repeated administrations [59].
Table 1: Comparison of Common Viral Vectors for CRISPR Delivery
| Vector Type | Packaging Capacity | Integration Profile | Primary Applications | Key Advantages | Key Challenges |
|---|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | ~4.7 kb | Primarily episomal | In vivo delivery | Favorable safety profile, high tissue specificity [58] | Limited cargo capacity, pre-existing immunity [58] [54] |
| Lentivirus (LV) | ~8 kb | Integrating | Ex vivo cell engineering (T cells, HSPCs) [55] | Sustained long-term expression, high transduction efficiency [59] | Risk of insertional mutagenesis [59] |
| Adenovirus (AdV) | Up to 36 kb | Episomal | In vivo delivery, vaccination | Very large cargo capacity, high tropism [56] | Significant immunogenicity, strong inflammatory response [59] |
Non-Viral Delivery: Lipid Nanoparticles (LNPs)
Lipid Nanoparticles (LNPs) are synthetic, spherical vesicles composed of ionizable lipids, phospholipids, cholesterol, and PEG-lipids that self-assemble to encapsulate nucleic acid payloads [60]. They have emerged as a powerful non-viral platform for delivering CRISPR components, particularly in the following forms:
- CRISPR-mRNA/sgRNA: LNPs encapsulate mRNA encoding the Cas9 protein and a separate sgRNA. After cellular uptake and endosomal escape, the mRNA is translated into functional Cas9 protein in the cytoplasm, which then complexes with the sgRNA to form an active nuclease [61].
- Ribonucleoprotein (RNP): LNPs can be formulated to deliver pre-assembled Cas9 protein-gRNA complexes directly into the cell cytoplasm [62] [63]. RNP delivery offers a rapid onset of action, short intracellular half-life that minimizes off-target effects, and avoids the need for transcription or translation [56] [63].
A critical advancement in LNP technology is the development of Selective Organ Targeting (SORT) LNPs. By incorporating additional SORT molecules, researchers can engineer LNPs to preferentially deliver their payload to specific organs beyond the liver, such as the lungs and spleen [56]. Recent research has also focused on formulating LNPs with thermostable Cas9 orthologs, such as the engineered iGeoCas9, which maintains its structure and function during the LNP formulation process, leading to high editing efficiency in the liver and lungs of mice after a single intravenous injection [63].
Table 2: LNP-Delivered Cargo Formats for CRISPR-Cas9
| Cargo Format | Components Delivered | Mechanism of Action | Advantages | Disadvantages |
|---|---|---|---|---|
| mRNA + sgRNA | mRNA encoding Cas9; sgRNA | In situ translation of Cas9 protein, then RNP formation | Avoids plasmid integration, scalable production [54] | Can trigger immune responses (TLR activation), slower onset than RNP [63] |
| Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and gRNA | Immediate activity upon cytoplasmic delivery | Rapid editing, reduced off-target effects, minimal immunogenicity [62] [63] | Formulation challenges, stability during manufacturing [63] |
In Vivo vs. Ex Vivo Editing: A Technical Comparison
The strategic decision between in vivo and ex vivo editing has profound implications for the entire research and development pipeline, from vector selection to clinical trial design.
In Vivo Genome Editing
In vivo editing aims to deliver CRISPR therapeutics directly to the target cells within the patient's body. This approach is particularly advantageous for targeting organs that are difficult to remove and culture, such as the brain, liver, or muscle.
- Delivery Modalities: AAV vectors are a dominant platform due to their excellent in vivo stability and tissue tropism [58] [54]. LNPs are also gaining prominence, especially for liver-targeted therapies and, increasingly, for other tissues using SORT technology [56] [63].
- Key Considerations:
- Tissue Tropism and Targeting: The choice of vector serotype (for AAV) or LNP composition is critical to ensure efficient delivery to the desired organ [58] [63].
- Immune Response: Pre-existing antibodies against viral capsids or the bacterial-derived Cas9 protein can neutralize the therapy and pose safety risks [54] [57]. LNPs and RNP delivery generally exhibit lower immunogenicity [60] [63].
- Scalability and Manufacturing: LNPs have a proven, scalable manufacturing pathway, as demonstrated by their use in COVID-19 vaccines. AAV production at a commercial scale remains more complex and costly [60].
Ex Vivo Genome Editing
Ex vivo editing involves harvesting cells from a patient, genetically modifying them under controlled conditions in a GMP facility, and then reinfusing the edited cells. This approach is the foundation of CAR-T cell therapies and is being explored for hematopoietic stem cell (HSC) therapies.
- Delivery Modalities: Electroporation has been the traditional workhorse for delivering CRISPR RNPs or mRNAs into cells ex vivo [62] [55]. However, LNPs are emerging as a less toxic and highly efficient alternative [62]. Lentiviral vectors are also widely used for delivering complex transgenes, such as chimeric antigen receptors (CARs), in ex vivo settings [59] [55].
- Key Considerations:
- Cytotoxicity: Electroporation causes significant cell death, membrane damage, and activates stress and inflammatory pathways, reducing the yield of viable edited cells [62]. LNP-mediated delivery dramatically reduces this cytotoxicity, leading to higher cell yields and improved growth post-editing [62].
- DNA Damage Response (DDR): In HSPCs, electroporation of CRISPR components activates a robust p53-dependent DDR, which can impair the cells' reconstitution potential. LNP delivery dampens this DDR, preserving clonogenic activity [62].
- Quality Control: The ex vivo process allows for rigorous quality control, including sequencing of the edited cell product and functional validation before patient infusion.
Table 3: In Vivo vs. Ex Vivo Genome Editing at a Glance
| Feature | In Vivo Editing | Ex Vivo Editing |
|---|---|---|
| Workflow | Direct administration to patient | Cell extraction, external modification, reinfusion |
| Primary Delivery Vehicles | AAV, LNPs [58] [54] | Electroporation, LNPs, Lentivirus [62] [55] |
| Therapeutic Examples | EDIT-101 for LCA10 (retina) [58], Liver-directed therapies [63] | CAR-T therapies (e.g., for cancer), Gene-edited HSPCs for sickle cell disease [55] |
| Key Challenges | Immune responses, off-target effects, tissue-specific targeting [54] [57] | Cell viability post-editing, preserving stem cell potential, complex manufacturing [62] |
| Manufacturing | Complex for viral vectors; more scalable for LNPs [60] | Complex, patient-specific (autologous); requires GMP facilities |
Experimental Protocols and Workflows
Protocol: LNP-Mediated Ex Vivo Editing of Human T Cells
This protocol outlines a method for editing human T cells using CRISPR LNPs, a less toxic alternative to electroporation [62].
- T Cell Activation: Isolate CD4+ T cells from human peripheral blood mononuclear cells (PBMCs). Activate the cells using CD3/CD28 activation beads and culture in IL-2 containing media for 72 hours.
- LNP Formulation: Formulate LNPs using a commercial kit (e.g., GenVoy-ILM T Cell Kit). Encapsulate the CRISPR payload, which can be either:
- Cas9 mRNA and sgRNA, or
- Pre-complexed Cas9 RNP.
- Cell Transfection: Seed the activated T cells at a concentration of 5 × 10^5 cells/mL. Add the formulated CRISPR LNPs to the cell culture medium. To enhance LNP uptake, add recombinant human ApoE (0.1 μg/mL) to the medium.
- Incubation and Wash: Incubate the cells with the LNPs for 24 hours. Wash the cells with DPBS to remove excess LNPs and reseed them in fresh culture medium.
- Analysis: Assess editing efficiency 72-96 hours post-transfection using next-generation sequencing (NGS) or the T7 endonuclease I assay on purified genomic DNA. Evaluate cell viability and phenotype via flow cytometry.
Ex Vivo T Cell Editing via LNP
Protocol: In Vivo Genome Editing Using AAV Vectors
This generalized protocol describes the process for conducting an in vivo gene editing experiment in a mouse model using AAV vectors [58].
- Vector Design and Production:
- For large Cas9 orthologs like SpCas9, employ a dual-AAV system. Design one vector to express a compact Cas9 ortholog (e.g., SaCas9) and the other to express the target sgRNA. Alternatively, use a single AAV vector if a compact Cas effector (e.g., IscB, TnpB) is employed.
- Package the expression cassettes into the desired AAV serotype (e.g., AAV8 for liver tropism, AAV5 for retina) using a standard triple-transfection method in HEK293T cells, followed by purification and concentration via ultracentrifugation.
- In Vivo Administration:
- Anesthetize the mouse. For liver-directed editing, administer the AAV vectors via systemic injection (e.g., tail vein injection). For retinal editing, use a subretinal injection technique. The typical dose ranges from 1e11 to 1e13 vector genomes (vg) per animal.
- Tissue Harvesting and Analysis:
- Sacrifice the animals at the predetermined endpoint (e.g., 2-4 weeks post-injection). Harvest the target tissue (e.g., liver, retina).
- Extract genomic DNA from the tissue. Quantify editing efficiency using digital droplet PCR (ddPCR) or deep sequencing of the target locus.
- For functional analysis, assess the phenotypic outcome, such as protein expression restoration via immunohistochemistry or measurement of relevant biochemical markers.
In Vivo Editing via AAV Delivery
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for CRISPR-Cas9 Delivery Experiments
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Cas9 Protein | Component of RNP complexes for direct nuclease delivery. | SpCas9 (Aldevron); Thermostable variants like iGeoCas9 for improved LNP formulation [62] [63]. |
| CleanCap Cas9 mRNA | In situ production of Cas9 protein after LNP or electroporation delivery. | 5-moU modified (Trilink) for enhanced stability and reduced immunogenicity [62]. |
| Synthetic sgRNA | Guides Cas9 to the specific genomic target site. | Chemically modified (Synthego) for improved stability and editing efficiency [62]. |
| AAV Serotypes | Determines tissue tropism for in vivo delivery. | AAV8 (liver), AAV5 (retina), AAV9 (broad tropism) [58]. |
| Ionizable Lipids | Critical component of LNPs for encapsulating nucleic acids and enabling endosomal escape. | DLin-MC3-DMA; novel biodegradable lipids for improved safety [63]. |
| GenVoy-ILM Kit | Commercial LNP formulation kit for ex vivo cell editing. | Precision Nanosystems [62]. |
| ApoE Protein | Enhances LNP uptake in cells expressing LDL receptors. | Recombinant human ApoE is added during LNP transfection [62]. |
| AAV6 Vector | Commonly used as HDR donor template in ex vivo editing of hematopoietic cells. | High transduction efficiency in HSPCs [62]. |
The landscape of CRISPR-Cas9 delivery is diverse and rapidly evolving. The choice between in vivo and ex vivo editing, and the subsequent selection of a delivery modality (viral vs. non-viral), is not a one-size-fits-all decision but a strategic one based on the target disease, tissue, and specific therapeutic goals. Viral vectors, particularly AAVs, offer high transduction efficiency and durable expression for in vivo use but face challenges related to packaging capacity and immunogenicity. LNPs present a versatile, scalable, and less immunogenic alternative, with RNP delivery emerging as a method to maximize editing precision and minimize off-target effects. For new researchers, the key is to align the delivery system with the biological and clinical constraints of the project. As the field progresses, the convergence of these technologies—such as using engineered LNPs to deliver novel, thermostable Cas effectors—promises to further expand the therapeutic potential of CRISPR genome editing.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) system, derived from a bacterial adaptive immune mechanism, has revolutionized biological research and therapeutic development. While its ability to create double-stranded breaks (DSBs) in DNA via the Cas9 nuclease for gene knockout or correction is well-established, the technology's utility has expanded far beyond these initial applications [64] [19] [11]. This guide explores two advanced frontiers: epigenetic editing, which allows for programmable alteration of gene expression without changing the underlying DNA sequence, and CRISPR-based diagnostic applications, which leverage the system's precise recognition capabilities for detection and quantification of nucleic acids. These developments are transforming basic research and creating new avenues for therapeutic intervention and molecular diagnostics.
Epigenetic Editing with CRISPR
Fundamental Principles and Mechanisms
Epigenetics refers to heritable changes in gene expression that do not involve alterations to the underlying DNA sequence. Key mechanisms include DNA methylation, histone modification, chromatin remodeling, and noncoding RNA interactions [65]. CRISPR-based epigenetic editing rewrites these epigenetic marks at specific genomic loci to activate or repress target genes. The primary strategy involves using a catalytically deactivated Cas9 (dCas9) that retains its DNA-binding capability but lacks nuclease activity. This dCas9 serves as a programmable targeting module when fused to various epigenetic effector domains (epieffectors) [65].
The dCas9-epieffector complex is guided to specific genomic loci by a customizable guide RNA (gRNA). Upon binding, the fused effector domain catalyzes the deposition or removal of epigenetic marks, such as methyl or acetyl groups, thereby modulating the local chromatin state and influencing gene expression [65]. This approach enables precise temporal and spatial control over epigenetic states, facilitating functional studies of specific epigenetic marks and offering potential therapeutic pathways for diseases characterized by epigenetic dysregulation.
Key Epigenetic Effector Systems
Several dCas9-epieffector systems have been developed for targeted epigenetic modification, each with distinct functions and applications. The table below summarizes the primary epigenetic editing tools currently available.
Table 1: Key dCas9-Epieffector Systems for Epigenome Editing
| dCas9-Effector Complex | Type of Epigenetic Modification | Primary Function | Reported Applications |
|---|---|---|---|
| dCas9-KRAB | Induces histone methylation (H3K9me3) | Gene downregulation [65] | Silencing of multiple globin genes in K562 cells [65] |
| dCas9-DNMT3A | Catalyzes DNA methylation | Gene repression [65] | Methylation of targeted CpG sites within gene promoters [65] |
| dCas9-p300 core | Catalyzes histone acetylation (H3K27ac) | Gene activation [65] | Activation of Myod and Oct4 genes; upregulation of hemoglobin genes [65] |
| dCas9-LSD1 | Removes histone acetylation marks | Gene downregulation [65] | Downregulation of Tbx3 and impairment of pluripotency in embryonic stem cells [65] |
| dCas9-TET | Catalyzes DNA demethylation | Gene activation [65] | Reactivation of epigenetically silenced genes in cell lines [65] |
| dCas9-VP64/VPR | Recruits transcriptional activators | Strong gene activation [65] | Activation of silenced Oct4; aided neuronal differentiation of iPSCs [65] |
Experimental Protocol for Targeted Gene Activation Using dCas9-p300
This protocol provides a methodology for targeted gene activation in mammalian cells using the dCas9-p300 core activator system, which acetylates histone H3 at lysine 27 (H3K27ac) to create an open chromatin state permissive to transcription.
Materials Required:
- Plasmids: dCas9-p300 core fusion construct (e.g., Addgene #61357); sgRNA expression vector (e.g., pU6-sgRNA from Addgene)
- Cells: Mammalian cell line of interest (e.g., HEK293T, K562, or iPSCs)
- Reagents: Cell culture media and transfection reagent (e.g., lipofectamine, calcium phosphate, or electroporation kit)
- Controls: Non-targeting sgRNA; dCas9-only vector
Procedure:
- sgRNA Design and Cloning: Design a 20-nucleotide sgRNA sequence targeting a regulatory region (e.g., promoter or enhancer) of your gene of interest. The target site must be adjacent to a Protospacer Adjacent Motif (PAM) with the sequence 5'-NGG-3'. Clone the annealed oligonucleotides into the BsmBI site of your sgRNA expression vector. Validate the construct by Sanger sequencing using a U6 promoter primer [64] [65].
- Cell Transfection: Culture cells to 70-90% confluency in an appropriate medium. Co-transfect the dCas9-p300 plasmid and the sgRNA plasmid at an optimal ratio (e.g., 1:1 to 1:3 mass ratio). Include controls transfected with non-targeting sgRNA and dCas9-p300. For hard-to-transfect cells, use electroporation or viral delivery [66] [65].
- Incubation and Analysis: Harvest cells 48-72 hours post-transfection.
- Efficiency Validation: Assess editing efficiency by quantifying changes in H3K27ac enrichment at the target locus using Chromatin Immunoprecipitation (ChIP)-qPCR.
- Functional Output: Measure mRNA expression levels of the target gene using RT-qPCR and quantify changes in protein expression via Western blot or immunofluorescence.
Advanced Strategies for Enhanced Epigenome Editing
To improve the efficiency and robustness of epigenetic editing, several advanced systems have been engineered:
- dCas9-SunTag System: This system utilizes a dCas9 fused to a repeating peptide array (SunTag), which can recruit multiple copies of an epieffector protein (e.g., TET1 or DNMT3A). This multiplexed recruitment significantly augments the editing effect, leading to higher rates of demethylation (up to 90% at some loci) and stronger gene activation compared to single effector fusions [65].
- CRISPR-SAM (Synergistic Activation Mediator): This system incorporates modified sgRNAs containing RNA aptamers that recruit additional activator proteins (e.g., MS2-p65-HSF1). This creates a synergistic effect, resulting in very strong transcriptional activation of endogenous genes, which is particularly useful for manipulating cell fate or activating silenced genes [65].
Diagram 1: Mechanism of CRISPR-based Epigenetic Editing. The dCas9 protein, fused to an epigenetic effector, is guided to a specific genomic locus by a gRNA. Upon binding, the effector domain modifies local epigenetic marks (e.g., acetylation, methylation), altering the chromatin state and resulting in targeted gene activation or repression.
CRISPR-Based Diagnostic Applications
Fundamentals of CRISPR Diagnostics
CRISPR diagnostics leverage the inherent precision of CRISPR-Cas systems to recognize specific nucleic acid sequences, coupled with the collateral activity of certain Cas proteins, to create highly sensitive and specific detection tools. The most well-established system for diagnostics uses Cas12 and Cas13 proteins. Upon recognizing their target DNA or RNA sequence, these enzymes become activated and cleave not only the target but also surrounding non-target single-stranded DNA or RNA molecules (reporter molecules) in a phenomenon known as trans- or collateral cleavage [67]. This collateral activity provides a powerful signal amplification mechanism that can be coupled to a detectable output, such as fluorescence.
SEEKER: A Quantitative Search Engine for DNA Data Storage
A novel and powerful application of CRISPR diagnostics is in the field of DNA data storage. Search Enabled by Enzymatic Keyword Recognition (SEEKER) is a method that uses CRISPR-Cas12a to perform quantitative keyword searches within information encoded in synthetic DNA [67].
Principle of Operation: SEEKER utilizes the collateral activity of Cas12a. A crRNA is designed to be complementary to a DNA sequence representing a "keyword." If the keyword is present in the amplified DNA data pool, Cas12a is activated and cleaves a single-stranded DNA fluorophore-quencher (ssDNA-FQ) reporter. This cleavage separates the fluorophore from the quencher, generating a fluorescent signal. The key feature of SEEKER is that the growth rate of the fluorescence intensity is proportional to the frequency of the keyword in the file, enabling quantitative searching [67].
Table 2: Key Components of the SEEKER Diagnostic System
| Component | Function | Specifications/Notes |
|---|---|---|
| Cas12a Enzyme | RNA-guided nuclease; performs targeted and collateral cleavage | Recognizes a T-rich PAM (5'-TTTN-3'); collateral activity is triggered upon target binding [67] |
| crRNA (Query) | Guides Cas12a to the target DNA sequence (the "keyword") | Sequence is computationally determined from the recovered dictionary of the DNA data storage system [67] |
| ssDNA-FQ Reporter | Signal generation molecule; cleaved collateraly by activated Cas12a | Fluorophore and quencher are attached to a short ssDNA; cleavage generates fluorescence [67] |
| Target DNA Amplicons | Amplified data files from the DNA storage pool to be searched | Generated via PCR using file-specific primers; serves as the substrate for the CRISPR search [67] |
| Microfluidic Chip | Platform for parallelized searching | 3D-printed chip with multiple reaction chambers; allows simultaneous querying of multiple files or with multiple keywords [67] |
Experimental Protocol for Keyword Search Using SEEKER
This protocol outlines the steps to perform a quantitative keyword search in DNA-encoded text data using the SEEKER method.
Materials Required:
- Oligo Pool: Synthetic DNA pool containing the encoded data and reference (dictionary) strands.
- PCR Reagents: Polymerase, dNTPs, and file-specific primer pairs.
- SEEKER Reaction Mix: Recombinant Cas12a enzyme, custom-synthesized crRNA (designed to match the keyword sequence), ssDNA-FQ reporter (e.g., 5'-6-FAM-TTATT-3IABkFQ-3'), and reaction buffer.
- Equipment: Real-time PCR machine or fluorometer for fluorescence detection; 3D-printed microfluidic chip (optional for parallelization).
Procedure:
- Data Recovery and Query Design: Amplify and sequence the reference strands from the DNA storage pool to recover the dictionary. Computationally map the text keyword of interest to its corresponding nucleotide sequence using the dictionary. Synthesize the corresponding crRNA [67].
- File Amplification: Perform PCR on the DNA storage pool using specific primer pairs to amplify the individual files of interest. Purify the amplicons to remove excess primers and dNTPs [67].
- SEEKER Reaction Setup: For each file to be queried, set up a 20 µL reaction containing:
- 1x Cas12a reaction buffer
- 50 nM Cas12a enzyme
- 50 nM crRNA (keyword query)
- 100-500 nM ssDNA-FQ reporter
- 10-50 ng of the purified file amplicon
- Run reactions in a real-time PCR machine to monitor fluorescence (FAM channel) every minute for 1-2 hours.
- Data Analysis: Calculate the fluorescence growth rate (slope of the fluorescence curve over time) for each reaction. The growth rate is quantitatively correlated with the frequency of the keyword in the original file. Compare results to positive (file known to contain the keyword) and negative (no template or non-targeting crRNA) controls [67].
Diagram 2: SEEKER Workflow for DNA Data Search. The Cas12a-crRNA complex binds to its target DNA sequence (the keyword) within amplified data files. This binding activates the complex, triggering indiscriminate cleavage of nearby ssDNA-FQ reporters. The resulting fluorescence intensity grows at a rate proportional to the keyword's frequency in the file, enabling quantitative searching.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Advanced CRISPR Applications
| Reagent / Solution | Critical Function | Application Notes |
|---|---|---|
| dCas9-Effector Plasmids | Serves as the expression vector for the epigenetic editing fusion protein. | Available from repositories like Addgene; common effectors include p300, KRAB, DNMT3A, and TET1 [65]. |
| sgRNA Expression Vectors | Drives the expression of the guide RNA for target specificity. | Cloned with a U6 promoter; must be designed with a 20-nt guide sequence specific to the target and a compatible PAM [64] [65]. |
| Cas12a (Cpf1) Enzyme | RNA-guided nuclease used in diagnostic applications like SEEKER. | Recognizes a T-rich PAM (5'-TTTN-3'); exhibits robust collateral cleavage activity upon target binding [67]. |
| ssDNA-FQ Reporter | Provides a detectable signal upon cleavage by activated Cas proteins. | A short ssDNA oligo labeled with a fluorophore and a quencher; crucial for fluorescence-based readouts in diagnostics [67]. |
| Cell Line-Specific Transfection Reagents | Enables delivery of CRISPR components into cells. | Choice is critical and depends on the cell type (e.g., lipofection for HEK293T, electroporation for primary cells) [66] [65]. |
The evolution of CRISPR technology from a simple gene-editing tool into a multifaceted platform for epigenetic rewriting and molecular diagnostics marks a significant leap forward for biomedical science. Epigenetic editing with dCas9-effector fusions provides unprecedented control over gene regulation, enabling the functional dissection of epigenetic mechanisms and opening new therapeutic avenues. Simultaneously, CRISPR-based diagnostics, exemplified by the SEEKER system, demonstrate the versatility of Cas enzymes in applications beyond cellular manipulation, such as quantitative information retrieval from DNA data storage. As these toolkits continue to expand with innovations like ultrasound-controlled systems for spatiotemporal precision [68], they promise to further empower researchers and clinicians in their quest to understand and treat complex diseases.
The clinical application of CRISPR-Cas9 genome editing is rapidly advancing from theoretical promise to therapeutic reality. This whitepaper reviews the current landscape of clinical trials in cardiovascular and rare diseases, highlighting a pivotal shift toward in vivo gene editing strategies. The field has matured significantly with the first regulatory approvals of CRISPR-based therapies, most notably for sickle cell disease and beta thalassemia. Current research focuses on overcoming historical challenges in delivery systems, with lipid nanoparticles (LNPs) emerging as a key technology for targeted organ delivery. This review synthesizes the most promising clinical developments as of 2025, detailing experimental methodologies, quantitative outcomes, and the essential research toolkit required to advance this groundbreaking field. The convergence of precision genetic tools with sophisticated delivery platforms is creating unprecedented opportunities to address both common cardiovascular conditions and a spectrum of rare genetic disorders.
The adaptation of the prokaryotic CRISPR-Cas9 (Clustered Regularly Interspaced Short Palindromic Repeats-CRISPR associated protein 9) system into a programmable genome-editing tool has revolutionized therapeutic development [64]. This system functions as a RNA-guided DNA endonuclease, where a single guide RNA (sgRNA) directs the Cas9 enzyme to a specific genomic locus complementary to a 20-nucleotide spacer sequence, immediately preceding a Protospacer Adjacent Motif (PAM, 5'-NGG-3' for Streptococcus pyogenes Cas9) [64]. The resulting double-strand break (DSB) is then repaired by the cell's endogenous machinery, primarily through error-prone non-homologous end joining (NHEJ), leading to gene disruption, or the lower-efficiency homology-directed repair (HDR), enabling precise gene correction [64].
Early clinical success with ex vivo strategies—where a patient's cells are edited outside the body and reinfused—has paved the way for the more complex challenge of in vivo editing, wherein the therapeutic is administered directly to the patient. This transition is being enabled by advances in delivery vectors, particularly lipid nanoparticles (LNPs) that show a natural tropism for the liver, making hepatic targets a primary focus for early in vivo trials [7]. This whitepaper examines how these technological foundations are being applied in active clinical trials for cardiovascular and rare diseases, summarizing key findings, methodologies, and future directions.
Promising Clinical Trials in Cardiovascular Disease
Cardiovascular disease remains a leading cause of global mortality, creating an urgent need for durable therapies. Gene-editing approaches aim to mimic natural, protective genetic mutations to confer long-term risk reduction.
In Vivo ANGPTL3 Editing for Lipid Management
CTX310 (CRISPR Therapeutics) is an investigational, LNP-delivered CRISPR/Cas9 therapy designed to precisely edit the angiopoietin-like 3 (ANGPTL3) gene in hepatocytes following a single-course intravenous administration [69]. ANGPTL3 encodes a protein that regulates triglycerides and LDL cholesterol, both established risk factors for atherosclerotic cardiovascular disease (ASCVD) [69]. Individuals with naturally occurring loss-of-function mutations in ANGPTL3 have lower lipid levels and a reduced lifetime risk of cardiovascular disease [70].
- Clinical Trial Design and Demographics: The Phase 1, open-label, dose-escalation trial (NCT06451770) evaluated single IV doses of CTX310 (0.1 to 0.8 mg/kg lean body weight) in 15 adults with severe, refractory lipid disorders, including homozygous and heterozygous familial hypercholesterolemia (HoFH, HeFH), severe hypertriglyceridemia (sHTG), and mixed dyslipidemias [69] [70]. The median age was 53 years, and the majority were male. All participants had elevated lipid levels despite being on standard-of-care background therapy, with 40% taking PCSK9 inhibitors [69].
- Key Efficacy Results: The trial demonstrated robust, dose-dependent editing of ANGPTL3, leading to significant lipid reductions sustained for at least 60 days of follow-up [69] [70]. Key outcomes are summarized in Table 1.
Table 1: Key Efficacy Outcomes from the CTX310 Phase 1 Clinical Trial
| Parameter | Dose Level (mg/kg) | Mean Reduction (%) | Maximum Reduction (%) | Timepoint |
|---|---|---|---|---|
| Circulating ANGPTL3 Protein | 0.8 | -73% | -89% | Day 30 [69] |
| Triglycerides (TG) | 0.8 | -55% | -84% | Day 60 [69] |
| Triglycerides (TG) (in participants with baseline >150 mg/dL) | Therapeutic Doses | -60% | N/R | Day 60 [69] |
| LDL Cholesterol | 0.8 | -49% | -87% | Day 60 [69] |
Abbreviation: N/R = Not Reported
- Safety and Tolerability: CTX310 was generally well-tolerated. No dose-limiting toxicities or treatment-related serious adverse events were reported [69]. Adverse events were generally mild to moderate, with some participants experiencing infusion-related reactions (e.g., back pain, nausea) that resolved with medication. One participant with elevated liver enzymes at screening had a transient, self-resolving Grade 2 elevation [70]. The safety profile supports continued clinical advancement [69].
Other Notable Cardiovascular Trials
The landscape of cardiovascular gene editing extends beyond ANGPTL3, targeting other key pathways involved in cholesterol metabolism and blood pressure regulation.
- Lp(a) Reduction with CTX320: CRISPR Therapeutics is also developing CTX320, an LNP-delivered therapy targeting the LPA gene, which encodes apolipoprotein(a), a major component of lipoprotein(a) [Lp(a)] [69]. Elevated Lp(a) is an independent, genetically determined risk factor for ASCVD. CTX320 is currently in ongoing clinical trials [69].
- Twice-Yearly siRNA for Hypertension: While not a CRISPR-based therapy, zilebesiran is an investigational siRNA therapy that targets angiotensinogen (AGT) and is administered once every six months. The KARDIA-3 trial is evaluating this therapy, representing a parallel approach in long-acting, RNA-targeted cardiovascular therapeutics that could complement gene-editing strategies [71].
The following diagram illustrates the mechanistic workflow of an LNP-delivered CRISPR therapy for a cardiovascular target like ANGPTL3.
Promising Clinical Trials in Rare Diseases
Rare diseases, with their typically monogenic origins, are ideal candidates for CRISPR-based intervention. While over 6,000 rare diseases affect an estimated 300-400 million people globally, only about 5% have an approved treatment, highlighting a massive unmet medical need [72]. The following trials exemplify the progress being made.
Hereditary Transthyretin Amyloidosis (hATTR)
NTLA-2001 (Intellia Therapeutics) is a landmark therapy as the first systemically administered in vivo CRISPR-Cas9 therapy to enter clinical trials [7]. It utilizes LNPs to deliver CRISPR components targeting the transthyretin (TTR) gene in the liver for the treatment of hATTR, a condition characterized by the accumulation of misfolded TTR protein in nerves and the heart [7].
- Clinical Outcomes: In a Phase 1 trial, a single infusion of NTLA-2001 resulted in "quick, deep, and long-lasting" average reductions of approximately 90% in serum TTR levels, sustained over two years of follow-up [7]. Functional and quality-of-life assessments in participants largely showed disease stability or improvement.
- Safety: The therapy was well-tolerated, with mild or moderate infusion-related events being the most common side effects [7]. Phase III global trials for hATTR patients with cardiomyopathy and neuropathy are now underway, with data expected to support commercialization in the coming years [7].
Hereditary Angioedema (HAE)
Also developed by Intellia Therapeutics, this in vivo LNP-delivered therapy targets the kallikrein B1 (KLKB1) gene to reduce the production of plasma kallikrein, a key driver of pathological inflammation in HAE [7].
- Clinical Outcomes: In a Phase I/II trial, participants receiving the higher dose demonstrated an average 86% reduction in kallikrein levels and a significant reduction in the rate of HAE attacks. Eight of eleven participants in the high-dose group were attack-free during the 16-week observation period reported in 2024 [7].
PersonalizedIn VivoTherapy for CPS1 Deficiency
In a landmark case of personalized medicine, a team including researchers from the Innovative Genomics Institute developed a bespoke in vivo CRISPR therapy for an infant with CPS1 deficiency, a rare, life-threatening metabolic disorder [7].
- Protocol and Outcome: The therapy was delivered via LNP and administered by IV infusion. Crucially, the use of LNPs instead of a viral vector allowed for multiple doses to increase editing efficiency. The patient, KJ, received three doses, showed improved symptoms, reduced medication dependence, and no serious side effects, providing a proof-of-concept for rapid, on-demand CRISPR therapy for ultra-rare diseases [7].
Table 2: Summary of Key Rare Disease Clinical Trials Utilizing CRISPR
| Therapy / Trial | Target Gene | Condition | Delivery Method | Key Outcome |
|---|---|---|---|---|
| NTLA-2001 (Intellia) | TTR | Hereditary Transthyretin Amyloidosis (hATTR) | LNP, IV Infusion | ~90% sustained reduction in serum TTR protein [7] |
| Intellia HAE Therapy | KLKB1 | Hereditary Angioedema (HAE) | LNP, IV Infusion | 86% reduction in kallikrein; most patients attack-free [7] |
| Personalized CPS1 Therapy | CPS1 | CPS1 Deficiency (Ultra-rare) | LNP, IV Infusion (multi-dose) | Symptom improvement; proof-of-concept for N-of-1 therapy [7] |
Detailed Experimental Protocols
The successful translation of CRISPR therapies relies on standardized, robust experimental workflows. Below is a detailed protocol for an in vivo LNP-based therapy, representative of the trials discussed.
Protocol:In VivoGene Knockout via LNP-Delivered CRISPR-Cas9
Objective: To achieve durable knockout of a target gene (e.g., ANGPTL3, TTR) in hepatocytes in vivo via a single intravenous administration of an LNP formulation containing CRISPR-Cas9 ribonucleoprotein (RNP) or mRNA/gRNA constructs.
Materials:
- CRISPR Components: Purified S. pyogenes Cas9 protein and synthetic sgRNA targeting the gene of interest, OR codon-optimized Cas9 mRNA and sgRNA.
- Lipid Nanoparticles (LNPs): A proprietary or commercially available LNP formulation (e.g., comprising ionizable lipid, phospholipid, cholesterol, and PEG-lipid) for in vivo use.
- Animal Model: A relevant preclinical model (e.g., mouse, non-human primate) with appropriate disease phenotype.
- Formulation Buffer: Typically, a sterile, isotonic buffer such as PBS, pH 7.4.
- Analytical Tools: Next-generation sequencing (NGS) for indel analysis, ELISA for target protein quantification, and clinical chemistry analyzers for biomarkers (e.g., ALT/AST for liver safety).
Methodology:
- sgRNA Design and Validation:
- Design a 20-nucleotide spacer sequence targeting an early exon of the target gene, ensuring high on-target activity and minimal off-target potential via predictive algorithms.
- In vitro transcription or chemically synthesize the sgRNA.
- Validate cutting efficiency in vitro by co-transfecting Cas9 and sgRNA into a relevant cell line, followed by NGS of the target locus to determine the indel percentage.
LNP Formulation:
- Formulate the CRISPR payload (either pre-complexed Cas9 protein:sgRNA RNP or co-encapsulated Cas9 mRNA and sgRNA) into LNPs using a microfluidic mixing device.
- Purify the formulated LNPs via tangential flow filtration or dialysis to remove residual organic solvent and exchange the buffer into the final formulation buffer.
- Characterize the LNPs for particle size (e.g., 70-100 nm), polydispersity index, encapsulation efficiency, and concentration.
In Vivo Dosing:
- Randomize and acclimate animals.
- Administer the LNP formulation as a single, slow intravenous injection via the tail vein (mouse) or peripheral vein (NHP) at a predetermined dose (e.g., mg/kg lean body weight). Pre-treatment with corticosteroids and antihistamines may be used to mitigate infusion reactions [69].
- Include control groups receiving LNP formulations with a non-targeting sgRNA.
Efficacy and Safety Assessment:
- Bioanalysis: Periodically collect blood samples to monitor:
- Target Engagement: Reduction in circulating target protein (e.g., ANGPTL3, TTR) via ELISA.
- Phenotypic Effect: Reduction in downstream biomarkers (e.g., LDL, triglycerides).
- Safety: Clinical chemistry (liver transaminases ALT/AST, bilirubin) and hematology.
- Molecular Confirmation: At the terminal endpoint, harvest liver tissue. Isolate genomic DNA and perform PCR amplification of the on-target region. Use NGS to quantify the frequency of insertions and deletions (indels), confirming successful gene editing.
- Bioanalysis: Periodically collect blood samples to monitor:
Long-Term Follow-Up:
- As per FDA guidance for gene therapies, conduct long-term studies to monitor the durability of effect and assess for any delayed adverse events, including potential off-target editing events via unbiased methods like CIRCLE-seq.
The Scientist's Toolkit: Research Reagent Solutions
Advancing CRISPR therapies from bench to bedside requires a suite of specialized reagents and tools. The following table details essential materials for preclinical development.
Table 3: Essential Research Reagents for Developing CRISPR Therapies
| Reagent / Material | Function | Key Considerations |
|---|---|---|
| CRISPR-Cas9 Nuclease | The enzyme that creates a double-strand break at the target DNA sequence. | High-purity, recombinant protein (for RNP delivery) or IVT-grade, codon-optimized mRNA. Truncated sgRNAs can enhance specificity [64]. |
| Single Guide RNA (sgRNA) | A chimeric RNA that combines the functions of crRNA and tracrRNA to confer DNA target specificity [64]. | Chemically modified synthetic sgRNAs improve stability and reduce immunogenicity. Must be designed with high on-target and low off-target activity scores. |
| Lipid Nanoparticles (LNPs) | A delivery vehicle that encapsulates and protects CRISPR components and facilitates cellular uptake, particularly in the liver. | Formulation must balance efficacy, stability, and safety (reactogenicity). Comprising ionizable lipid, phospholipid, cholesterol, and PEG-lipid. |
| Vector Plasmid DNA | For in vitro and in vivo production of Cas9 mRNA and sgRNA via in vitro transcription (IVT). | High-copy number plasmid with T7/SP6 promoter; linearized template for IVT. Must be endotoxin-free. |
| Next-Generation Sequencing (NGS) | The gold standard for quantifying genome-editing efficiency (indel %) and profiling potential off-target effects. | Requires deep sequencing and specialized bioinformatics pipelines for analysis (e.g., CRISPResso2). |
| Cell Line with Target Expression | An in vitro model for initial sgRNA validation and functional assays. | Ideally, a human hepatocyte-derived cell line (e.g., HepG2, primary hepatocytes) for liver targets. |
The logical flow from target identification to clinical trial, and the associated toolkit, can be visualized as a multi-stage process.
Navigating CRISPR Challenges: Strategies for Enhancing Efficiency and Safety
CRISPR-Cas9 systems have revolutionized genome engineering by enabling precise modification of target genes, yet off-target effects remain a significant challenge for research and therapeutic applications [73]. These unintended genetic alterations occur when the Cas nuclease cleaves genomic sites other than the intended target, potentially leading to confounding experimental results and serious safety concerns in clinical applications [74] [75]. The tolerance of wild-type CRISPR systems for mismatches between the guide RNA (gRNA) and target DNA means that even sequences with three to five base pair mismatches can be cleaved under certain conditions [74]. For researchers embarking on CRISPR experiments, understanding and mitigating these off-target effects is paramount for generating reliable data and developing safe therapeutic interventions.
The clinical implications of off-target editing are substantial. Unintended mutations in protein-coding regions can disrupt gene function, and in worst-case scenarios, mutations in tumor suppressor genes or oncogenes could potentially initiate malignant transformation [25]. Recent studies have revealed that CRISPR-induced DNA damage extends beyond small insertions and deletions to include large structural variations such as chromosomal translocations and megabase-scale deletions [25]. This comprehensive technical guide examines the core strategies for minimizing off-target effects through optimized gRNA design and selection of high-fidelity Cas variants, providing foundational knowledge essential for new researchers in CRISPR genome editing.
Fundamentals of gRNA Design
The design of the single guide RNA (sgRNA) represents the most critical factor in determining both on-target efficiency and off-target potential. A well-designed gRNA maximizes specific binding to the intended genomic target while minimizing interactions with off-target sites.
Key Principles for Optimal gRNA Design
Several fundamental principles govern the design of gRNAs with minimal off-target potential:
GC Content Optimization: The GC content in the gRNA seed sequence (positions 1-12 adjacent to the PAM) significantly influences editing specificity. Research indicates that maintaining GC content between 40% and 60% stabilizes the DNA:RNA duplex for on-target binding while destabilizing off-target interactions [76]. gRNAs with GC content outside this range show increased off-target activity.
Guide Length Modification: Traditional 20-nucleotide gRNAs can be truncated to 17-19 nucleotides to reduce off-target effects while largely maintaining on-target activity. Shorter gRNAs have reduced tolerance for mismatches, thereby increasing specificity [76]. However, this approach requires empirical validation as excessive truncation can severely compromise on-target efficiency.
Specificity-Enhancing Modifications: The "GG20" approach, which incorporates two guanine nucleotides at the 5' end of the gRNA (creating ggX20 gRNAs), has demonstrated significantly reduced off-target effects while maintaining robust on-target activity [76]. Additionally, chemical modifications such as 2'-O-methyl-3'-phosphonoacetate at specific positions in the ribose-phosphate backbone can enhance specificity without compromising on-target performance [76].
Computational Tools for gRNA Design and Off-Target Prediction
Numerous computational tools have been developed to predict potential off-target sites and assist with gRNA design. These tools employ different algorithms to identify genomic sites with sequence similarity to the intended target.
Table 1: Computational Tools for gRNA Design and Off-Target Prediction
| Tool Name | Algorithm Type | Key Features | Advantages |
|---|---|---|---|
| Cas-OFFinder [75] | Alignment-based | Adjustable sgRNA length, PAM type, mismatch/bulge tolerance | Wide application range with high customizability |
| FlashFry [75] | Alignment-based | High-throughput analysis, GC content scoring | Rapid processing of large target sets |
| CCTop [75] | Scoring-based | Considers mismatch distance from PAM | User-friendly interface with reliable predictions |
| DeepCRISPR [75] | Machine Learning | Incorporates sequence and epigenetic features | Comprehensive profiling with higher accuracy |
These computational tools primarily identify sgRNA-dependent off-target sites based on sequence similarity but may overlook factors such as chromatin accessibility and epigenetic modifications [75]. Therefore, their predictions should be supplemented with experimental validation.
The following diagram illustrates the systematic workflow for optimal gRNA design and selection:
High-Fidelity Cas Variants
While gRNA design significantly influences specificity, the choice of Cas nuclease itself plays an equally crucial role in minimizing off-target effects. Both naturally occurring and engineered high-fidelity Cas variants offer improved specificity profiles compared to wild-type SpCas9.
Engineered High-Fidelity Cas9 Variants
Protein engineering approaches have yielded SpCas9 variants with dramatically reduced off-target activity through rational design targeting specific protein-DNA interactions:
SpCas9-HF1: This high-fidelity variant contains four alterations (N497A/R661A/Q695A/Q926A) designed to reduce non-specific contacts with the DNA phosphate backbone [77]. SpCas9-HF1 retains >85% of wild-type on-target activity for most gRNAs while rendering nearly all off-target events undetectable by genome-wide analysis methods [77] [76]. In comprehensive testing, SpCas9-HF1 exhibited comparable on-target activity to wild-type SpCas9 with 32 of 37 different sgRNAs (86%), demonstrating robust performance across diverse genomic targets [77].
eSpCas9: The enhanced specificity Cas9 variant was engineered through a similar approach targeting residues involved in non-specific DNA binding. Both eSpCas9 and SpCas9-HF1 employ a "proofreading mechanism" that traps the mutants in an inactive state when bound to mismatched targets [76], providing a structural basis for their improved fidelity.
eSpOT-ON: This commercially available engineered variant derived from Parasutterella secunda Cas9 (PsCas9) achieves exceptionally low off-target editing while retaining robust on-target activity, addressing the common trade-off between specificity and efficiency [78].
Alternative Cas Nucleases with Native High Specificity
Beyond engineered SpCas9 variants, several naturally occurring Cas nucleases from other bacterial species offer inherent advantages for specific applications:
SaCas9: Isolated from Staphylococcus aureus, SaCas9 recognizes a more complex PAM sequence (5'-NNGRRT-3') compared to SpCas9's 5'-NGG-3' [78] [76]. This longer PAM requirement substantially reduces the number of potential off-target sites in the genome. Additionally, at 1053 amino acids, SaCas9 is approximately 1 kb smaller than SpCas9, facilitating delivery with viral vectors such as AAV [78].
hfCas12Max: Engineered from the Cas12i family, this variant combines enhanced editing capabilities with reduced off-target effects [78]. Its simple 5'-TN PAM requirement expands targetable genomic regions while maintaining high fidelity, making it particularly valuable for therapeutic development.
Cas9 Nickase: By mutating one nuclease domain (RuvC or HNH), Cas9 nickase creates single-strand breaks instead of double-strand breaks [76]. When used in paired nickase systems with two appropriately spaced gRNAs, this approach significantly reduces off-target mutations while still enabling efficient genome editing [78].
Table 2: Comparison of High-Fidelity Cas Variants
| Cas Variant | PAM Sequence | Size (aa) | Key Features | Best Applications |
|---|---|---|---|---|
| SpCas9-HF1 [77] [76] | 5'-NGG-3' | 1368 | Quadruple mutations reducing non-specific DNA contacts | High-precision editing where SpCas9 target range is required |
| SaCas9 [78] [76] | 5'-NNGRRT-3' | 1053 | Native high fidelity; compact size for viral delivery | In vivo therapeutic applications requiring AAV delivery |
| hfCas12Max [78] | 5'-TN-3' | 1080 | Broad targeting range with high fidelity; staggered ends | Therapeutic development requiring diverse genomic targeting |
| eSpOT-ON [78] | Varies by source | ~1100 | Engineered PsCas9 with exceptional on/off-target ratio | Clinical applications demanding maximal specificity |
The following diagram illustrates the strategic decision process for selecting appropriate high-fidelity Cas variants based on experimental requirements:
Experimental Protocols for Off-Target Assessment
Rigorous experimental validation of off-target effects is essential for confirming the specificity of CRISPR editing systems. Both genome-wide unbiased methods and targeted approaches provide complementary information for comprehensive off-target assessment.
Genome-Wide Detection Methods
Unbiased genome-wide methods enable discovery of potential off-target sites without prior prediction:
GUIDE-seq (Genome-wide Unbiased Identification of DSBs Enabled by Sequencing): This highly sensitive method uses double-stranded oligodeoxynucleotides (dsODNs) that integrate into double-strand breaks, allowing comprehensive mapping of nuclease activity across the genome [77] [75]. The protocol involves: (1) Co-transfecting cells with Cas9-sgRNA plasmids and dsODN tags; (2) Harvesting genomic DNA 72 hours post-transfection; (3) Amplifying integrated tag sites; (4) High-throughput sequencing and bioinformatic analysis [77]. GUIDE-seq has demonstrated exceptional sensitivity in identifying off-target sites with frequencies as low as 0.1% [75].
CIRCLE-seq: This cell-free approach provides an ultra-sensitive assessment of nuclease specificity by: (1) Fragmenting and circularizing genomic DNA; (2) Incubating with Cas9-sgRNA ribonucleoprotein complexes; (3) Linearizing cleaved DNA fragments; (4) Sequencing and analyzing the resulting fragments [75]. CIRCLE-seq can detect potential off-target sites with single-nucleotide resolution and is particularly valuable for pre-clinical assessment of therapeutic gRNAs.
DISCOVER-seq (Discovery of In Situ Cas Off-Targets by Verification and Sequencing): This method exploits the natural DNA repair machinery by identifying sites enriched for the MRE11 repair protein following Cas9 cleavage [75]. The protocol involves: (1) Transfecting cells with CRISPR components; (2) Performing MRE11-specific chromatin immunoprecipitation; (3) Sequencing the immunoprecipitated DNA; (4) Bioinformatics analysis to identify off-target sites.
Targeted Sequencing Approaches
For validation of predicted off-target sites, targeted sequencing provides a cost-effective and focused approach:
Candidate Site Selection: Compile potential off-target sites using multiple computational tools (e.g., Cas-OFFinder, CCTop) with liberal mismatch parameters (up to 5-6 mismatches) [75].
PCR Amplification: Design primers flanking each predicted off-target site and the on-target site. Include barcodes for multiplexed sequencing.
Library Preparation and Sequencing: Amplify target regions from treated and control samples using high-fidelity polymerases. Prepare sequencing libraries using standard protocols and sequence with sufficient coverage (minimum 100,000x read depth per site) [77].
Data Analysis: Process sequencing data through a standardized pipeline: (a) Demultiplex samples; (b) Align reads to reference genome; (c) Quantify insertion/deletion frequencies at each site using tools like CRISPResso2 or ICE; (d) Statistically compare indel frequencies between treated and control samples [77].
Table 3: Experimental Methods for Off-Target Detection
| Method | Detection Principle | Sensitivity | Advantages | Limitations |
|---|---|---|---|---|
| GUIDE-seq [77] [75] | dsODN integration into DSBs | ~0.1% | Highly sensitive, genome-wide, low false positive rate | Requires efficient dsODN delivery |
| CIRCLE-seq [75] | In vitro cleavage of circularized DNA | ~0.01% | Ultra-sensitive, cell-free, minimal background | Does not account for cellular context |
| DISCOVER-seq [75] | MRE11 ChIP-seq at repair sites | ~1% | Works in primary cells, identifies functional off-targets | Lower sensitivity than other methods |
| Amplicon Sequencing [77] | Targeted sequencing of candidate sites | ~0.1-0.5% | Cost-effective, focused validation | Limited to predicted sites |
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of CRISPR genome editing with minimal off-target effects requires access to specialized reagents and tools. The following table outlines essential components for researchers designing specificity-optimized CRISPR experiments.
Table 4: Essential Research Reagents for Off-Target Minimization
| Reagent Category | Specific Examples | Function & Importance | Considerations for Use |
|---|---|---|---|
| High-Fidelity Cas Variants | SpCas9-HF1 [77], eSpCas9 [76], SaCas9 [78] | Engineered or natural variants with reduced off-target activity while maintaining on-target efficiency | Balance between specificity and efficiency; match nuclease to delivery constraints |
| Specificity-Optimized gRNAs | Chemically modified sgRNAs [74], truncated gRNAs [76] | Enhanced stability and reduced off-target binding through structural modifications | Chemical modifications (2'-O-Me, PS bonds) improve nuclease resistance and specificity |
| Off-Target Prediction Tools | Cas-OFFinder [75], CCTop [75], DeepCRISPR [75] | Computational nomination of potential off-target sites for experimental validation | Use multiple algorithms with different scoring systems for comprehensive prediction |
| Detection Kits & Assays | GUIDE-seq kits [75], T7 Endonuclease I assay [77] | Experimental validation of editing efficiency and specificity | GUIDE-seq provides genome-wide coverage; T7EI offers rapid efficiency assessment |
| Delivery Vehicles | AAV vectors [78], Lipid Nanoparticles (LNPs) [78] | Efficient intracellular delivery of CRISPR components with appropriate duration of expression | Transient expression reduces off-target risk; viral vectors require size-optimized components |
Minimizing off-target effects in CRISPR genome editing requires a multifaceted approach combining computational prediction, biochemical optimization, and rigorous experimental validation. Optimized gRNA design focusing on GC content, appropriate length, and strategic chemical modifications establishes the foundation for specific targeting. Complementarily, selection of high-fidelity Cas variants—whether engineered mutants like SpCas9-HF1 or naturally specific alternatives like SaCas9—dramatically reduces off-target cleavage while maintaining therapeutic efficacy. As CRISPR technologies evolve toward clinical application, comprehensive assessment using sensitive detection methods remains essential for verifying editing specificity. By systematically implementing these strategies, researchers can harness the full potential of CRISPR genome editing while minimizing unintended genetic consequences, enabling more reliable experimental outcomes and safer therapeutic interventions.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas system represents a transformative technology in genome editing, offering unprecedented capability for precise genetic modifications. However, the therapeutic application of CRISPR is fundamentally constrained by a single, critical factor: the efficient and safe delivery of its molecular components into target cells. The genome editing machinery—typically comprising the Cas nuclease and a guide RNA (gRNA)—is a large, negatively charged molecular complex that cannot passively cross cell membranes. Furthermore, these components are vulnerable to degradation by nucleases and can elicit undesirable immune responses. Consequently, the development of sophisticated delivery vehicles is not merely an auxiliary support technology but a prerequisite for realizing the full clinical potential of CRISPR-based therapies. The two most prominent strategies for overcoming this hurdle are lipid nanoparticles (LNPs) and optimized viral vectors, each offering distinct mechanisms, advantages, and limitations for researchers to consider [79] [56].
This guide provides an in-depth technical overview of these two delivery platforms, framed within the practical context of contemporary research and clinical development. The effective translocation of CRISPR cargo—which can be in the form of DNA, mRNA, or pre-assembled Ribonucleoprotein (RNP) complexes—is what bridges the gap between theoretical genome editing and its practical application in both basic research and therapeutic interventions [56].
Lipid Nanoparticles (LNPs): A Versatile Non-Viral Platform
Mechanism and Composition
Lipid Nanoparticles (LNPs) are synthetic, nano-sized vesicles primarily composed of ionizable lipids, phospholipids, cholesterol, and lipid-anchored polyethylene glycol (PEG). They function by encapsulating and protecting CRISPR-Cas9 components within a lipid bilayer, forming stable particles typically between 50-200 nm in diameter. The core mechanism of action involves leveraging the natural affinity of certain LNPs for specific organs, most notably the liver, following systemic administration via intravenous (IV) infusion [7] [79].
The journey of an LNP from administration to gene editing involves a coordinated sequence of cellular events, as illustrated below:
The critical step in this process is endosomal escape. Ionizable lipids within the LNP become protonated in the acidic environment of the endosome, leading to destabilization of the endosomal membrane and subsequent release of the CRISPR cargo into the cytoplasm before it can be degraded in the lysosome [79] [56].
Key Advances and Clinical Validation
LNPs have transitioned from a promising technology to a clinically validated platform, with demonstrated success in both common and rare diseases. The following table summarizes quantitative data from key clinical trials and studies utilizing LNP-mediated CRISPR delivery.
Table 1: Performance Data from LNP-Based CRISPR Clinical Trials and Studies
| Target Disease | CRISPR Cargo | Key Metric | Result | Significance |
|---|---|---|---|---|
| Hereditary Transthyretin Amyloidosis (hATTR) [7] | Cas9 mRNA + sgRNA (TTR) | Reduction in serum TTR protein | ~90% average reduction | Sustained for over 2 years in all participants |
| Hereditary Angioedema (HAE) [7] | Cas9 mRNA + sgRNA (Kallikrein) | Reduction in Kallikrein & attack frequency | 86% avg. reduction; 8/11 patients attack-free | Proof-of-concept for inflammatory disease |
| CPS1 Deficiency (Infant) [7] | Bespoke CRISPR Therapy | Patient outcome post-LNP dosing | Symptom improvement; safe redosing | First personalized in vivo CRISPR therapy |
A pivotal advantage of LNPs confirmed in recent clinical trials is the potential for redosing. Unlike viral vectors, which often provoke immune responses that preclude repeated administration, LNPs have demonstrated a tolerable safety profile that allows for multiple doses. For instance, in the case of an infant with CPS1 deficiency, three separate LNP doses were safely administered, each leading to incremental therapeutic benefits [7]. This flexibility is a significant asset for titrating therapy to achieve optimal editing efficiency.
Experimental Protocol: Formulating and Testing LNPs for CRISPR Delivery
Objective: To formulate, characterize, and test the efficacy of LNPs encapsulating CRISPR-Cas9 ribonucleoprotein (RNP) for in vitro gene editing.
Materials:
- Ionizable lipid (e.g., DLin-MC3-DMA)
- Helper lipids (DSPC, Cholesterol)
- PEG-lipid (DMG-PEG 2000)
- Cas9 protein and sgRNA
- Microfluidic mixer (e.g., NanoAssemblr)
- Dialysis membranes (MWCO 100 kDa)
- Cell line of interest (e.g., HEK293, HepG2)
Methodology:
- LNP Formulation:
- Prepare the organic phase: Dissolve ionizable lipid, DSPC, cholesterol, and PEG-lipid at a molar ratio (e.g., 50:10:38.5:1.5) in ethanol.
- Prepare the aqueous phase: Mix pre-complexed Cas9-sgRNA RNP in a citrate buffer (pH 4.0).
- Using a microfluidic mixer, rapidly combine the organic and aqueous phases at a defined flow rate ratio (e.g., 3:1, aqueous:organic) to facilitate spontaneous nanoparticle formation.
- Purification and Characterization:
- Dialyze the formulated LNPs against a phosphate-buffered saline (PBS) solution (pH 7.4) for 24 hours to remove residual ethanol and exchange the buffer.
- Characterize the final product using Dynamic Light Scattering (DLS) for particle size and polydispersity index (PDI), and nanoparticle tracking analysis (NTA) for concentration. Aim for a size of 80-120 nm with PDI < 0.2.
- Use the RiboGreen assay to quantify the encapsulation efficiency of the RNP.
- In Vitro Testing:
- Seed target cells in a 24-well plate and culture until 70-80% confluent.
- Treat cells with LNP formulations across a range of concentrations (e.g., 0.1 - 1.0 µg RNP/well). Include a negative control (e.g., PBS) and a positive control (e.g., commercial transfection reagent).
- After 72 hours, harvest cells and extract genomic DNA.
- Assess editing efficiency via T7 Endonuclease I assay or next-generation sequencing (NGS) of the target locus.
Viral Vector Optimization: Engineering Precision and Capacity
The rAAV Vector Platform
Recombinant adeno-associated virus (rAAV) vectors are among the most widely used viral platforms for in vivo gene therapy due to their favorable safety profile, high tissue specificity, and capacity for long-term transgene expression. rAAVs are non-pathogenic, predominantly persist in an episomal form without integrating into the host genome, and elicit relatively low immune responses compared to other viral vectors [58].
The primary constraint of rAAVs is their limited packaging capacity of less than 4.7 kb. The commonly used Streptococcus pyogenes Cas9 (SpCas9), at over 4.2 kb, leaves insufficient space for the necessary regulatory elements when combined with a gRNA expression cassette in a single vector. This has spurred the development of sophisticated workaround strategies [58].
Innovative Strategies for rAAV Optimization
To overcome the packaging limitation, researchers have engineered multiple innovative rAAV platforms. The logical relationships and workflows of these strategies are summarized in the diagram below.
Table 2: Optimized rAAV Platforms for CRISPR Delivery
| Strategy | Mechanism | Example | Advantage | Challenge |
|---|---|---|---|---|
| Compact Cas Orthologs [58] | Use of naturally small Cas proteins | SaCas9, CjCas9, Cas12f, IscB | Fits gRNA and Cas in single vector; simplified production | May have different PAM requirements; potential lower efficiency |
| Dual rAAV Vectors [56] [58] | Split Cas9 and gRNA into two separate vectors | SpCas9 split across two AAVs | Delivers full-length SpCas9; leverages high-efficacy nucleases | Requires high co-infection rate; increased manufacturing burden |
| Trans-Splicing Inteins [58] | Split Cas9 with intein tags; reconstitute post-delivery | SpCas9 split at specific sites | Delivers large nucleases beyond standard split capacity | Reconstitution efficiency can be variable |
The successful clinical application of rAAV-CRISPR is exemplified by EDIT-101, the first in vivo CRISPR therapy to enter human trials. This therapy uses an rAAV5 vector to deliver SaCas9 and two gRNAs to the retina for the treatment of Leber Congenital Amaurosis type 10 (LCA10). Early trial results demonstrated a favorable safety profile and improved photoreceptor function in the majority of participants, providing crucial proof-of-concept for rAAV-mediated in vivo genome editing in humans [58].
Experimental Protocol: Utilizing Dual rAAV Vectors forIn VivoEditing
Objective: To achieve in vivo genome editing in a mouse model using a dual rAAV system delivering SpCas9 and a target-specific gRNA.
Materials:
- rAAV-Cas9: Purified rAAV vector (e.g., serotype 8 or 9) encoding the SpCas9 nuclease.
- rAAV-gRNA: Purified rAAV vector of the same serotype encoding the U6-promoter driven sgRNA.
- Control rAAV: rAAV encoding a non-targeting gRNA.
- Animal model (e.g., C57BL/6 mice).
- Injection supplies (syringes, needles, sterile PBS).
Methodology:
- Vector Preparation and Quality Control:
- Produce and purify both rAAV-Cas9 and rAAV-gRNA vectors using a standard system (e.g., triple-transfection in HEK293 cells followed by iodixanol gradient ultracentrifugation).
- Quantify vector genomes (vg) via quantitative PCR (qPCR) and confirm the absence of replication-competent AAV.
- Mix rAAV-Cas9 and rAAV-gRNA at a 1:1 molar ratio in sterile PBS to the final working concentration (e.g., 1x10^12-10^13 vg/mL total).
- In Vivo Administration:
- Anesthetize mice according to approved animal protocol guidelines.
- Systemically administer the rAAV mixture via tail vein injection (common for liver targeting). A typical dose for a 20g mouse is 100-200 µL of the prepared vector solution.
- Include a control group injected with the rAAV-Cas9 + control gRNA vector.
- Efficiency Analysis:
- After 2-4 weeks, euthanize the animals and harvest the target tissue (e.g., liver).
- Extract genomic DNA from a portion of the tissue.
- Evaluate editing efficiency by NGS of the PCR-amplified target genomic locus.
- For functional assessment, analyze protein expression changes by Western Blot or immunohistochemistry on tissue sections.
Successful execution of CRISPR delivery experiments requires a suite of specialized reagents and tools. The following table catalogs key solutions for research in this field.
Table 3: Research Reagent Solutions for CRISPR Delivery Studies
| Item / Reagent | Function & Application | Key Considerations |
|---|---|---|
| Ionizable Cationic Lipids [79] | Core component of LNPs for nucleic acid complexation and endosomal escape. | Critical for efficiency; new formulations (e.g., SORT molecules) improve organ targeting beyond the liver. |
| Pre-complexed Cas9 RNP [56] | Directly usable CRISPR cargo; offers rapid action and reduced off-target effects. | Superior to DNA/mRNA delivery in reducing off-target effects and immune stimulation. |
| rAAV Serotype Library [58] | Different serotypes (e.g., AAV2, AAV8, AAV9) confer distinct tissue tropism. | Selection is critical for in vivo targeting (e.g., AAV9 for broad tissue uptake, AAV8 for liver). |
| Compact Cas Orthologs [58] | Smaller Cas proteins (e.g., SaCas9, Cas12f) for single-vector AAV packaging. | Must verify editing efficiency and PAM compatibility for the target locus. |
| Spherical Nucleic Acids (SNAs) [80] | Nanostructures that enhance cellular uptake and gene-editing efficiency. | Emerging technology showing 3x improved uptake and 60% higher precise repair rates vs. standard LNPs. |
| Enveloped Delivery Vehicles (EDVs) [81] | Engineered virus-like particles allowing surface decoration with targeting ligands. | Enables highly specific "AND-gate" targeting of cell types (e.g., T-cells) in vivo. |
The advancement of CRISPR genome editing from a powerful laboratory technique to a robust therapeutic modality is inextricably linked to progress in delivery technologies. As this guide has detailed, both Lipid Nanoparticles (LNPs) and optimized viral vectors provide powerful, though imperfect, solutions to the delivery challenge. LNPs excel in safety, redosing capability, and clinical validation for liver-targeted therapies, while engineered rAAV vectors offer the potential for long-term expression and high tropism for specific tissues like the retina.
The future of CRISPR delivery lies in the continued refinement of these platforms—developing novel lipids with enhanced tissue specificity, engineering next-generation viral vectors with expanded cargo capacity and targeting precision, and potentially combining the best attributes of both into hybrid systems. For researchers entering the field, a deep understanding of the principles, protocols, and tools outlined in this technical guide provides the foundational knowledge required to contribute to overcoming the central hurdle of delivery and unlocking the full potential of CRISPR-based medicine.
Addressing Scalability and Manufacturing Challenges for Clinical-Grade Therapies
The advancement of CRISPR-based therapies from laboratory research to approved medicines represents a monumental achievement in modern biotechnology. The approval of the first CRISPR-based medicine, Casgevy, for sickle cell disease and transfusion-dependent beta thalassemia, has solidified the therapeutic potential of gene editing [7]. However, the field now faces a critical transition from proving efficacy in individual cases to establishing scalable, robust, and economically viable manufacturing processes that can meet clinical demand. The scalability challenge encompasses both technical and regulatory hurdles, including the procurement of true Good Manufacturing Practice (GMP) reagents, complex manufacturing workflows, and evolving regulatory frameworks that must adapt to these novel therapeutic modalities [82]. Furthermore, market forces have increased pressure on companies to narrow their pipelines and focus on getting a smaller set of products to market quickly, rather than building broader therapeutic pipelines [7]. This whitepaper examines the core challenges in scaling CRISPR therapies and provides a detailed technical roadmap for researchers and drug development professionals navigating this complex landscape.
Current Challenges in Scaling CRISPR Therapies
Technical and Manufacturing Hurdles
The development of CRISPR cell and gene therapies faces several interconnected technical challenges that impact scalability:
GMP Reagent Procurement: Obtaining true GMP-grade CRISPR components (Cas nucleases and guide RNAs) remains a significant bottleneck. The complexity of GMP requirements means few companies offer true GMP reagents (not just "GMP-like"), and demand is rapidly outstripping supply. This can delay clinical trials by months to years [82].
Process Consistency: CRISPR therapies are inherently variable, and changing vendors of critical raw materials between research and clinical stages can result in unintended process changes. This variability risks clinical results that are not comparable and poses additional patient safety concerns [82].
Delivery System Limitations: Efficient delivery of CRISPR components to target cells remains a fundamental challenge, particularly for in vivo therapies. While lipid nanoparticles (LNPs) have shown success for liver-targeted therapies, their application to other tissues and organs requires further development [7].
Regulatory and Expertise Challenges
The regulatory landscape for CRISPR therapies continues to evolve, presenting unique challenges:
Unclear Regulatory Guidelines: The existing clinical development framework was designed for small molecule drugs, not complex CRISPR therapies. Regulatory agencies are still developing appropriate frameworks for assessing questions unique to gene editing, such as confirming editing sequences, determining durability of effect, and addressing potential off-target effects [82].
Expertise Shortages: The complexity and novelty of CRISPR therapies demand highly specialized expertise, including scientists, clinical project managers, data managers, regulatory experts, and medical writers. The current boom in cell and gene therapy development has led to staff shortages that can impede clinical trial progress [82].
Table 1: Key Challenges in Scaling CRISPR Therapies and Their Impact
| Challenge Category | Specific Challenge | Impact on Scalability |
|---|---|---|
| Manufacturing | GMP reagent procurement | Delays clinical trials by months to years; limits production capacity |
| Manufacturing | Process consistency & standardization | Risks variable efficacy and safety; complicates regulatory approval |
| Technical | Delivery system limitations | Restricts treatable diseases to specific tissues/organs |
| Technical | Off-target effects & safety concerns | Requires extensive safety profiling; may limit therapeutic applications |
| Regulatory | Evolving regulatory frameworks | Creates uncertainty in development pathways; extends timelines |
| Workforce | Specialized expertise shortages | Impedes clinical trial progress and technology advancement |
Analytical Framework: Assessing Scalability Across Modalities
The scalability challenges differ significantly between ex vivo and in vivo CRISPR therapy approaches, each with distinct manufacturing and regulatory considerations.
Ex Vivo vs. In Vivo Therapeutic Approaches
Ex Vivo Therapies involve editing cells outside the body before reinfusion into patients. This approach, used in Casgevy, offers greater control over editing efficiency and safety but requires complex, patient-specific manufacturing processes [7]. The autologous nature of these therapies creates significant scalability challenges due to the need for individualized manufacturing batches.
In Vivo Therapies deliver CRISPR components directly to cells inside the body, typically using viral vectors or lipid nanoparticles (LNPs). This approach offers better scalability potential as it uses standardized, off-the-shelf manufacturing [7]. Recent advances include the first personalized in vivo CRISPR treatment for an infant with CPS1 deficiency, developed and delivered in just six months [7].
Diagram 1: CRISPR Therapy Modalities and Scalability
Economic and Funding Constraints
The CRISPR therapy landscape faces significant economic challenges that impact scalability. Recent reductions in venture capital investment have forced companies to narrow their pipelines and focus on getting a smaller set of products to market quickly [7]. Additionally, government funding for basic and applied scientific research has seen major cuts, with National Science Foundation funding cut in half and funding for undergraduate STEM education cut by 71% [7]. These financial pressures have led to significant layoffs across CRISPR-focused companies and threaten to slow the pace of research and development of new manufacturing approaches.
Manufacturing Workflows and Quality Control
Comprehensive Manufacturing Process
A robust manufacturing workflow is essential for producing clinical-grade CRISPR therapies. The process varies between ex vivo and in vivo approaches but shares common elements requiring stringent quality control.
Diagram 2: CRISPR Therapy Manufacturing Workflows
Essential Research Reagent Solutions
Successful development of CRISPR therapies requires carefully selected research reagents and materials. The table below details key components and their functions in therapeutic development.
Table 2: Essential Research Reagent Solutions for CRISPR Therapy Development
| Reagent/Material | Function | GMP Requirements | Considerations for Scaling |
|---|---|---|---|
| Cas Nuclease | Creates double-strand breaks in DNA | Required for clinical use | High purity; minimal off-target activity; multiple variants available (Cas9, Cas12) |
| Guide RNA (gRNA) | Targets nuclease to specific genomic sequence | Required for clinical use | Sequence specificity; stability; modified bases for enhanced performance |
| Delivery Vector | Delivers editing components to cells | Required for clinical use | LNP vs. viral vector (AAV, lentivirus); tissue tropism; immunogenicity |
| Cell Culture Media | Supports growth and maintenance of cells | Required for ex vivo therapies | Serum-free formulations; defined components; scalability |
| Editing Enhancers | Improves HDR efficiency; reduces NHEJ | Preclinical assessment | Small molecules (e.g., DNA-PKcs inhibitors); potential safety concerns |
| Analytical Tools | Assesses editing efficiency and safety | Quality control testing | NGS for on/off-target assessment; CAST-Seq for structural variations |
Safety Considerations and Risk Mitigation
Genome Integrity and Structural Variations
Recent research has revealed that beyond well-documented concerns of off-target mutagenesis, CRISPR editing can cause large structural variations (SVs), including chromosomal translocations and megabase-scale deletions [25]. These undervalued genomic alterations raise substantial safety concerns for clinical translation. Particularly concerning is that traditional short-read amplicon sequencing often fails to detect extensive deletions or genomic rearrangements that delete primer-binding sites, rendering them 'invisible' to conventional analysis [25]. This limitation can lead to overestimation of homology-directed repair (HDR) rates and concurrent underestimation of indels.
Strategies to enhance HDR efficiency, such as using DNA-PKcs inhibitors, have been shown to exacerbate these genomic aberrations. One study found that the DNA-PKcs inhibitor AZD7648 significantly increased frequencies of kilobase- and megabase-scale deletions as well as chromosomal arm losses across multiple human cell types and loci [25]. Furthermore, off-target profiles were markedly aggravated, with surveys revealing not only a qualitative rise in translocation sites but also an alarming thousand-fold increase in the frequency of such structural variations.
Risk Assessment and Safety Profiling
Comprehensive safety assessment of CRISPR therapies requires advanced analytical methods to detect both on-target and off-target effects:
Off-Target Analysis: Cell-based genome-wide analyses of off-target activity at sites with sequence similarity to the intended target are crucial. Advances in sensitive detection methods have driven the engineering of Cas variants with enhanced target site selectivity as well as refined gRNA design [25].
Structural Variation Detection: Methods like CAST-Seq and LAM-HTGTS can identify large structural variations and chromosomal rearrangements that conventional sequencing might miss [25].
Tumorigenicity Assessment: Evaluation of potential oncogenic consequences through analysis of edits in tumor suppressor genes or proto-oncogenes, combined with long-term cell culture studies to monitor for malignant transformation.
Emerging Solutions and Future Directions
Technical Innovations in CRISPR Platforms
Several innovative approaches are being developed to address current scalability and safety challenges:
Novel CRISPR Systems: Companies like Mammoth Biosciences are developing ultra-small CRISPR systems (Cas14, CasΦ) that are significantly smaller than standard Cas9, potentially enabling delivery to a wider range of tissues [5].
Base and Prime Editing: Beam Therapeutics is pioneering base editing technologies that enable single-nucleotide changes without double-strand breaks, potentially reducing unwanted indels and off-target damage [5]. Prime editing offers even greater precision for specific sequence changes.
Epigenetic Editing: Companies like nChroma Bio (formed from the merger of Chroma Medicine and Nvelop Therapeutics) are developing epigenetic editing approaches that modify gene expression without changing the underlying DNA sequence, potentially avoiding risks associated with DNA breaks [5].
Allogeneic Approaches: Companies including Caribou Biosciences and CRISPR Therapeutics are developing allogeneic (off-the-shelf) cell therapies that could significantly improve scalability compared to patient-specific autologous approaches [83] [5].
Process Improvement and Standardization
Standardization of manufacturing processes is critical for scaling CRISPR therapies:
Platform Process Development: Establishing standardized platform processes that can be applied across multiple therapeutic programs can reduce development timelines and improve manufacturing consistency.
Automated Closed Systems: Implementing automated closed-system manufacturing technologies can reduce manual operations, improve process consistency, and decrease contamination risk.
Analytical Advancements: Developing improved analytical methods to better characterize CRISPR therapies, including advanced sequencing approaches to detect structural variations and more sensitive off-target detection methods.
The global market for genome editing is projected to grow from $10.8 billion in 2025 to $23.7 billion by 2030, representing a compound annual growth rate of 16.9% [84]. This significant market expansion will likely drive further investment in manufacturing innovations and scalability solutions.
The path to scalable manufacturing of clinical-grade CRISPR therapies requires addressing interconnected challenges in process development, safety assessment, regulatory alignment, and workforce development. While significant hurdles remain, the rapid pace of innovation in CRISPR technology, coupled with growing clinical validation, provides a strong foundation for overcoming these challenges. Success will depend on collaborative efforts between researchers, manufacturers, regulators, and clinicians to establish robust, scalable manufacturing platforms that can deliver on the full therapeutic potential of CRISPR technologies for patients in need. The companies and researchers who prioritize addressing these scalability challenges today will be best positioned to deliver the transformative medicines of tomorrow.
The field of genome engineering has evolved remarkably, progressing from early protein-based systems like zinc-finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) to the revolutionary CRISPR-Cas system [85] [86]. CRISPR technology has fundamentally transformed genetic research through its simplicity and versatility, utilizing guide RNA (gRNA) to direct Cas proteins to specific genomic targets [85]. Despite its transformative impact, CRISPR technology faces significant challenges, including variable editing efficiencies across different cell types, sequence context dependencies, and unintended off-target effects throughout the genome [85].
Artificial intelligence (AI), particularly machine learning (ML) and deep learning (DL), has emerged as a powerful solution to these limitations [85] [86]. By leveraging large-scale datasets from diverse experiments, AI enhances gRNA design, predicts off-target activities, improves editing efficiency, and even facilitates the creation of novel CRISPR systems beyond natural evolutionary constraints [85]. This integration of AI with CRISPR technology provides new modalities essential for innovating personalized therapies while ensuring efficiency, precision, and safety [85]. This technical guide explores how AI-driven approaches are revolutionizing CRISPR genome editing, focusing on AI-generated editors and improved gRNA prediction methodologies for new researchers and drug development professionals.
AI-Generated CRISPR Editors: Breaking Natural Constraints
Traditional approaches to optimizing CRISPR systems, such as directed evolution and structure-guided mutagenesis, are limited by their reliance on naturally occurring sequences and often involve trade-offs between different properties [87]. Generative AI models present a paradigm shift by enabling the design of novel gene editors from scratch, unconstrained by natural evolution.
OpenCRISPR-1: The First AI-Designed Gene Editor
Researchers at Profluent Bio have demonstrated this capability by creating OpenCRISPR-1, the first fully AI-generated gene editor [87] [88]. Their approach involved several key methodological innovations:
- Training Data Curation: The team compiled the CRISPR-Cas Atlas, an extensive dataset of over one million CRISPR operons mined from 26 terabases of assembled genomes and metagenomes, representing the most comprehensive dataset of CRISPR systems curated to date [87].
- Model Architecture and Training: They fine-tuned ProGen2, a protein language model previously developed by Profluent, using the CRISPR-Cas Atlas to specialize in generating CRISPR-Cas proteins [87]. The training data was balanced for protein family representation and sequence cluster size to ensure broad coverage.
- Sequence Generation and Filtering: The fine-tuned models generated four million novel CRISPR-Cas protein sequences, which were then filtered and clustered to assess novelty and diversity [87].
- Structural Validation: AlphaFold2 predicted the structures of 5,000 AI-generated sequences to assess structural viability before experimental testing [87].
- Experimental Validation: 209 Cas9-like proteins were synthesized, human codon-optimized, cloned into expression plasmids, and tested for gene-editing activity in HEK293T cells [87]. Both on-target efficiency and off-target effects were assessed across multiple genomic sites using next-generation sequencing.
The resulting OpenCRISPR-1 editor maintains the prototypical architecture of a Type II Cas9 nuclease but contains 403 mutations compared to SpCas9 and 182 mutations from any natural protein in the CRISPR-Cas Atlas [87] [88]. Experimental characterization revealed that OpenCRISPR-1 achieves comparable on-target editing efficiency to SpCas9 (median indel rates of 55.7% versus 48.3%) while demonstrating a 95% reduction in off-target editing across multiple genomic sites (median indel rates of 0.32% versus 6.1%) [87]. Furthermore, OpenCRISPR-1 lacks immunodominant and subdominant T cell epitopes for HLA-A*02:01 previously identified in SpCas9, suggesting potentially lower immunogenicity [87].
Workflow for AI-Driven Editor Design
The following diagram illustrates the comprehensive workflow for designing and validating AI-generated CRISPR editors:
Enhanced gRNA Prediction Through Advanced AI Models
Accurate prediction of gRNA efficiency and specificity remains a fundamental challenge in CRISPR experiment design. AI models have dramatically improved these predictions by learning from large-scale experimental datasets.
Evolution of gRNA Efficiency Prediction Models
The development of AI models for gRNA design has progressed through several generations, each incorporating more sophisticated algorithms and larger datasets:
- Early Models: Doench et al. (2014) developed Rule Set 1 by assembling tiling gRNA pools for endogenous genes and classifying gRNAs with high activity, identifying sequence features predictive of efficiency [85]. Subsequent work led to Rule Set 2, which incorporated a library including perfectly matched gRNAs and those with insertions, deletions, or mismatches, deriving the cutting frequency determination (CFD) score for off-target prediction [85].
- Deep Learning Approaches: Chuai et al. formulated DeepCRISPR, a deep learning model that simultaneously predicts on-target efficiencies and genome-wide off-target effects of Cas9 by addressing data imbalances through augmentation and bootstrapping [85]. Kim et al. designed DeepSpCas9 using a convolutional neural network (CNN) trained on high-throughput screening of 12,832 target sequences, demonstrating better generalization across different datasets compared to existing models [85].
- Recent Innovations: Rule Set 3 elucidated how variations among trans-activating CRISPR RNA (tracrRNA) variants influence gRNA activity, incorporating these insights into a prediction model using LightGBM [85].
Multi-Dataset Training for Base Editing Prediction
Base editors (BEs), including adenine base editors (ABEs) that convert A•T to G•C and cytosine base editors (CBEs) that convert C•G to T•A, enable precise single nucleotide substitutions without introducing double-strand breaks [89]. However, predicting their efficiency is complicated by "bystander" edits within an approximately 8-nucleotide window [89] [90].
A groundbreaking approach from researchers in Denmark addresses the challenge of data heterogeneity by developing deep learning models trained simultaneously on multiple datasets while explicitly tracking their origins [89] [90]. The key methodological advances include:
- Dataset-Aware Training: Rather than simply pooling data from different sources, the model architecture labels each gRNA by its dataset of origin during training, allowing the model to learn systematic differences between datasets without forcing them into a single unified scale [89] [90].
- Multi-Task Prediction: The models predict both overall gRNA editing efficiency and the frequency of specific editing outcomes simultaneously from a 30-nucleotide input DNA target sequence [89].
- Feature Integration: The architecture incorporates the 30nt DNA sequences (20nt protospacer + 3nt PAM + flanking sequences), gRNA-DNA binding energy (ΔGB), labeling of target nucleotide editing positions for different outcomes, and predicted Cas9 efficiency [89].
The researchers generated substantial new experimental data using their SURRO-seq technology, measuring base-editing efficiency for approximately 11,500 gRNAs each for ABE7.10 and BE4-Gam base editors in HEK293T cells [89] [90]. After integration with published datasets, they developed CRISPRon-ABE and CRISPRon-CBE models, which demonstrated superior performance compared to existing tools including DeepABE/CBE, BE-HIVE, BE-DICT, BE_Endo, and BEDICT2.0 when evaluated on independent test sets [89] [90].
Architecture for Multi-Dataset Base Editing Prediction
The following diagram illustrates the dataset-aware training approach for predicting base editing outcomes:
Practical AI Tools for CRISPR Experiment Design
Beyond specific model architectures, researchers have developed comprehensive AI assistant systems that streamline the entire CRISPR experiment design process.
CRISPR-GPT: An AI Co-pilot for Gene Editing
Stanford Medicine researchers have developed CRISPR-GPT, an LLM agent system that automates and enhances CRISPR-based gene-editing design and data analysis [91] [8] [92]. This system incorporates domain expertise, retrieval techniques, external tools, and a specialized LLM fine-tuned with open-forum discussions among scientists [91]. CRISPR-GPT offers three operational modes:
- Meta Mode: Designed for beginner researchers, guiding them through essential tasks from CRISPR system selection and delivery methods to gRNA design, off-target assessment, protocol generation, and data analysis [91].
- Auto Mode: Caters to advanced researchers, allowing freestyle requests that the LLM Planner decomposes into tasks, manages interdependencies, builds customized workflows, and executes automatically [91].
- Q&A Mode: Supports users with on-demand scientific inquiries about gene editing [91].
In validation experiments, junior researchers using CRISPR-GPT successfully knocked out four genes with CRISPR-Cas12a in a human lung adenocarcinoma cell line and epigenetically activated two genes using CRISPR-dCas9 in a human melanoma cell line on their first attempt, achieving over 90% editing efficiency [91] [8] [92].
Experimental Protocols for AI-Enhanced CRISPR Workflows
SURRO-seq Protocol for Base Editing Data Generation
The SURRO-seq (lentiviral gRNA-target pair library) technology enables massive parallel quantification of base editing efficiency and outcomes [89] [90]:
- Library Construction: Create a lentiviral library pairing gRNAs with their target sequences integrated into the genome.
- Cell Transduction: Transduce HEK293T cells expressing base editors (ABE7.10 or BE4-Gam) with the gRNA-target pair library at a low multiplicity of infection (MOI of 0.3) to ensure approximately 1000x coverage.
- Selection and Induction: Culture transduced cells in selective medium containing puromycin (for selecting cells with integrated gRNA-target pair construct) and doxycycline (for induction of ABE/CBE expression) for 8 days.
- Amplicon Sequencing: Perform deep amplicon sequencing using surrogate target site-specific PCR products with approximately 2000 reads per gRNA.
- Data Processing: Remove low-quality gRNAs (<100 reads) and analyze editing efficiencies and outcomes from the remaining gRNAs (>11,000 per editor).
Validation Protocol for AI-Designed Editors
The experimental validation of AI-generated editors like OpenCRISPR-1 follows this methodology [87]:
- Candidate Selection: Filter AI-generated sequences based on novelty, diversity, and predicted structural viability using AlphaFold2.
- Synthesis and Cloning: Synthesize selected Cas9-like proteins, human codon-optimize them, and clone into mammalian expression plasmids.
- Cell Culture and Transfection: Culture HEK293T cells and transfect with plasmids expressing the AI-designed editors and corresponding gRNAs.
- Editing Assessment: Harvest cells 3-5 days post-transfection and extract genomic DNA.
- Next-Generation Sequencing: Amplify target regions and perform next-generation sequencing to assess both on-target efficiency and off-target effects across multiple genomic sites.
- Data Analysis: Calculate indel percentages for on-target and off-target sites, comparing against positive controls (e.g., SpCas9).
The Scientist's Toolkit: Essential Research Reagents
Table 1: Key Research Reagents for AI-Enhanced CRISPR Experiments
| Reagent/Material | Function and Application |
|---|---|
| SURRO-seq Library | Paired gRNA-target constructs for high-throughput measurement of editing efficiency and outcomes [89] [90]. |
| ABE7.10 & BE4-Gam | Base editor variants for A•T to G•C and C•G to T•A conversions, used in efficiency prediction studies [89] [90]. |
| OpenCRISPR-1 | AI-generated gene editor with comparable on-target efficiency and improved specificity relative to SpCas9 [87] [88]. |
| CRISPRon-ABE/CBE | Deep learning models for predicting base editing gRNA efficiency and outcome frequencies [89] [90]. |
| CRISPR-GPT | LLM agent system for automated CRISPR experiment planning, design, and analysis [91] [8]. |
| HEK293T Cells | Commonly used human cell line for validating CRISPR editing efficiency and specificity [89] [87]. |
Performance Comparison of AI-Enhanced CRISPR Technologies
Table 2: Quantitative Performance of AI-Enhanced CRISPR Technologies
| Technology | Key Metrics | Performance Advantages |
|---|---|---|
| OpenCRISPR-1 | Median on-target indel rate: 55.7%Median off-target indel rate: 0.32% [87] | Comparable on-target efficiency to SpCas9 (48.3%) with 95% reduction in off-target editing [87] |
| CRISPRon-ABE/CBE | Two-dimensional correlation coefficients (R² and ρ²) for joint evaluation of efficiency and outcome predictions [89] | Superior performance versus DeepABE/CBE, BE-HIVE, BE-DICT, BE_Endo, and BEDICT2.0 on independent test sets [89] [90] |
| CRISPR-GPT | >90% editing efficiency achieved by novice researchers on first attempt [8] [92] | Successful knockout of 4 genes and epigenetic activation of 2 genes across different cell lines [91] |
| Rule Set 3 | Incorporates tracrRNA variant effects on gRNA activity [85] | Improved gRNA activity prediction using LightGBM algorithm [85] |
Mitigating Immune Responses and Ensuring Long-Term Safety of Edits
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) system represents a transformative technology for genome editing, yet its therapeutic application faces significant immunological hurdles. These challenges primarily stem from the bacterial origin of CRISPR components, which the human immune system can recognize as foreign substances. Pre-existing immunity exists in a substantial proportion of the human population—approximately 80% of people have been found to have antibodies against Cas9 proteins from Staphylococcus aureus and Streptococcus pyogenes [93]. This immune recognition can trigger both antibody-mediated and T-cell-mediated responses that may eliminate edited cells, reduce therapeutic efficacy, and potentially cause adverse inflammatory reactions [93]. Understanding and mitigating these immune responses is therefore critical for developing safe and effective CRISPR-based therapies.
The immune system can be activated by multiple components of the CRISPR system. Beyond the Cas nuclease proteins, studies have revealed that the guide RNAs (gRNAs) produced via in vitro transcription can also trigger innate immune responses when they contain a 5'-triphosphate group (5'-ppp gRNAs) [94]. These gRNAs are recognized by the DDX58 receptor (also known as RIG-I) in the cytosol, activating type I interferon pathways that can lead to significant cytotoxicity—causing death in up to 80% of transfected cells in some experimental systems [94]. This comprehensive immune recognition of both protein and nucleic acid components creates a complex challenge for therapeutic development that requires multifaceted mitigation strategies.
Mechanisms of Immune Activation
Adaptive Immunity to Cas Proteins
The bacterial origin of Cas nucleases presents a fundamental challenge for therapeutic applications. Common sources of Cas9 include Staphylococcus aureus (SaCas9) and Streptococcus pyogenes (SpCas9), bacteria that frequently colonize humans and cause common infections [93]. As a result, most people have pre-existing immune memory to these bacterial proteins. Serological studies have detected anti-Cas9 IgG antibodies in 79% of samples tested against SaCas9 and 65% against SpCas9 [93]. Perhaps more importantly, cellular immunity with T cells reactive to Cas9 has been observed at rates of 46% for SaCas9, though at lower levels for SpCas9 in the same study [93].
When Cas9 is introduced during therapy, these pre-existing immune responses can be activated, potentially leading to the destruction of the very cells that the therapy aims to correct. The cytotoxic T lymphocytes (CTLs) can recognize Cas9-derived peptides presented on major histocompatibility complex (MHC) molecules on the surface of treated cells, marking them for destruction [93]. This immune elimination would render the therapy ineffective and could potentially cause inflammatory side effects. The risk is particularly significant for delivery approaches that lead to long-term Cas9 expression, as this provides a persistent stimulus for immune activation.
Innate Immune Recognition of CRISPR Components
In addition to adaptive immune responses to Cas proteins, the nucleic acid components of CRISPR systems can trigger innate immune pathways. Guide RNAs produced by in vitro transcription typically contain a 5'-triphosphate group that is recognized by cytosolic RNA sensors, primarily DDX58 (RIG-I) [94]. This recognition activates a signaling cascade that leads to the production of type I interferons and the upregulation of interferon-stimulated genes (ISGs) such as OAS2 and PKR [94].
The table below summarizes key immune triggers in CRISPR components and their consequences:
Table 1: Immune Triggers in CRISPR Components and Their Consequences
| CRISPR Component | Immune Trigger | Recognition Receptor | Immune Response | Functional Consequences |
|---|---|---|---|---|
| Cas9 Protein (SaCas9, SpCas9) | Bacterial protein sequences | MHC I/II, B-cell receptors | Pre-existing antibodies and T-cells | Potential elimination of edited cells; Reduced therapy efficacy |
| In Vitro Transcribed gRNA | 5'-triphosphate group | DDX58 (RIG-I) | Type I interferon production | Cytotoxicity; Up to 80% cell death |
| Plasmid DNA | Unmethylated CpG motifs | TLR9 | Inflammatory cytokine production | Cellular toxicity; Reduced editing efficiency |
This activation of innate immunity not only causes direct cytotoxicity but can also create an inflammatory environment that may enhance adaptive immune responses to the CRISPR components. The interferon response triggered by 5'-ppp gRNAs can lead to widespread changes in cellular gene expression that reduce cell viability and potentially compromise the function of the edited cells that survive [94].
Strategies for Mitigating Immune Responses
Protein Engineering to Reduce Immunogenicity
Recent advances in protein engineering have enabled the development of minimally immunogenic Cas nucleases. Researchers have employed structure-based computational tools to redesign Cas9 and Cas12 proteins, identifying and modifying immunogenic epitopes while preserving enzymatic function [95]. This rational engineering approach involves:
- Identification of immunogenic sequences using mass spectrometry to analyze protein fragments recognized by immune cells
- Computational protein design to create variants that lack these immunogenic sequences
- Functional validation of the engineered nucleases to ensure retained editing efficiency
In one implementation of this approach, researchers identified three short sequences (approximately eight amino acids long) on both Cas9 and Cas12 that evoked immune responses [95]. Through computational modeling in collaboration with Cyrus Biotechnology, they designed novel versions without these immune-triggering sequences. When tested in humanized mouse models, these engineered enzymes demonstrated significantly reduced immune responses while maintaining similar gene-editing efficiency compared to standard nucleases [95].
The following diagram illustrates the workflow for engineering minimally immunogenic nucleases:
Delivery System Optimization
The choice of delivery system significantly influences the immunogenicity of CRISPR therapies. Lipid nanoparticles (LNPs) have emerged as a promising delivery modality that can reduce immune recognition compared to viral vectors [7]. Key advantages of LNPs include:
- Reduced pre-existing immunity: Unlike viral vectors such as AAV, LNPs do not have high rates of pre-existing immunity in the human population
- Controlled expression duration: LNP-delivered mRNA typically results in transient Cas9 expression, limiting the window for immune recognition
- Redosing capability: LNPs do not trigger the same immune memory responses as viral vectors, allowing for multiple administrations if needed [7]
Clinical evidence supports the reduced immunogenicity of LNP delivery. In trials of CRISPR therapies for hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) delivered via LNPs, participants showed sustained protein reduction with no evidence of loss of effect over time, suggesting limited immune-mediated clearance of edited cells [7]. Additionally, the successful redosing of participants in these trials demonstrates that LNP delivery does not induce the strong anti-vector immunity that precludes repeated administration with viral vectors [7].
Chemical Modifications of Guide RNAs
The innate immune response triggered by in vitro transcribed (IVT) gRNAs can be effectively mitigated through chemical modifications of the RNA molecules. The primary strategy involves removing the 5'-triphosphate group that is recognized by DDX58 [94]. Practical approaches include:
- Enzymatic dephosphorylation using calf intestinal phosphatase (CIP) to convert 5'-triphosphate to 5'-hydroxyl groups
- Chemical synthesis of gRNAs with 5'-hydroxyl groups instead of triphosphate groups
- Post-synthesis purification to remove immunogenic RNA species
Experimental evidence demonstrates that these modifications effectively prevent immune activation without compromising editing efficiency. In primary human CD4+ T cells, 5'-hydroxyl gRNAs complexed with Cas9 avoided innate immune responses while achieving targeted mutagenesis at a frequency of 95% [94]. In contrast, 5'-triphosphate gRNAs in the same system activated strong interferon responses and caused significant cell death [94].
Table 2: Comparison of Guide RNA Modification Strategies
| gRNA Type | 5' End Chemistry | Immune Activation | Editing Efficiency | Production Cost |
|---|---|---|---|---|
| IVT gRNA | 5'-triphosphate | High (DDX58-mediated) | High | Low |
| CIP-treated IVT gRNA | 5'-hydroxyl | Minimal | High | Moderate |
| Chemically Synthesized gRNA | 5'-hydroxyl | Minimal | High | High |
Additional Mitigation Approaches
Several complementary strategies can further reduce immune responses to CRISPR components:
- Tissue-specific promoters: Using promoters that restrict expression to target tissues (e.g., liver-specific promoters) can prevent Cas9 expression in antigen-presenting cells, reducing immune activation [93]
- Transient expression systems: Delivery of preassembled ribonucleoprotein (RNP) complexes rather than nucleic acid templates results in shorter Cas9 persistence, limiting exposure to the immune system [94]
- Immunosuppressive regimens: Short-term corticosteroid treatment during initial therapy can suppress inflammatory responses without requiring long-term immunosuppression [93]
- Novel Cas orthologs: Sourcing Cas proteins from bacteria with low human prevalence can reduce rates of pre-existing immunity [93]
Experimental Protocols for Assessing Immunogenicity
In Vitro Immunogenicity Testing
Comprehensive assessment of CRISPR component immunogenicity requires a combination of in vitro and in vivo approaches. For initial screening, the following protocol can be used to evaluate immune activation by guide RNAs:
Protocol: Assessing gRNA-mediated Immune Activation in Human Cells
- Cell Culture: Maintain HeLa cells or primary human cells in appropriate medium under standard conditions
- gRNA Preparation:
- Synthesize target gRNAs via in vitro transcription (IVT) and chemical synthesis
- Treat IVT gRNAs with calf intestinal phosphatase (CIP) to remove 5'-triphosphate groups
- Complex gRNAs with recombinant Cas9 protein to form ribonucleoprotein (RNP) complexes
- Transfection: Introduce RNP complexes into cells using lipofection or electroporation
- Immune Response Analysis (24 hours post-transfection):
- Quantify IFNB1 mRNA expression by quantitative PCR
- Measure IFNB1 protein secretion by ELISA
- Assess expression of interferon-stimulated genes (DDX58, OAS2) by qPCR
- Evaluate cytotoxicity by cell viability assays
This protocol was used to demonstrate that 5'-ppp gRNAs up-regulated IFNB1 mRNA levels by approximately 1000-fold and protein levels by 200-fold, while 5'-OH gRNAs showed no significant immune activation [94].
In Vivo Immunogenicity Assessment
For preclinical assessment of Cas protein immunogenicity, humanized mouse models provide a relevant experimental system:
Protocol: Evaluating Cas9 Immune Responses in Humanized Mouse Models
- Model Generation: Utilize immunodeficient mice engrafted with human immune cells
- CRISPR Delivery: Administer CRISPR components via the intended therapeutic route (e.g., intravenous injection of LNP-formulated mRNA)
- Immune Monitoring:
- Measure anti-Cas9 antibody titers at baseline and weekly post-treatment using ELISA
- Isolate peripheral blood mononuclear cells (PBMCs) for T-cell proliferation assays using Cas9-derived peptides
- Assess Cas9-specific T-cell responses by interferon-γ ELISpot
- Analyze inflammatory cytokine levels in serum
- Evaluate editing efficiency in target tissues by sequencing
- Histopathological Examination: Assess immune cell infiltration in target tissues
Using similar approaches, researchers have validated engineered Cas variants with reduced immunogenicity, demonstrating significantly lower immune responses while maintaining editing efficiency in vivo [95].
The following diagram illustrates the key immune recognition pathways for CRISPR components:
Research Reagent Solutions
The table below provides essential reagents and their functions for studying and mitigating immune responses in CRISPR applications:
Table 3: Essential Research Reagents for CRISPR Immunogenicity Studies
| Reagent/Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Low-Immunogenicity Cas Variants | Engineered Cas9/Cas12 [95] | Gene editing with reduced immune recognition | Computationally designed to eliminate immunogenic epitopes; Retains editing efficiency |
| Guide RNA Modifications | CIP-treated IVT gRNAs [94] | Avoid DDX58-mediated immune activation | 5'-hydroxyl group prevents RIG-I recognition; Cost-effective production |
| Immune Assessment Tools | IFN-β ELISA [94] | Quantify innate immune activation | Sensitive detection of interferon response; Standardized quantification |
| Specialized Delivery Systems | Lipid Nanoparticles (LNPs) [7] | In vivo delivery with reduced immunogenicity | Enables redosing; Transient expression; Liver-targeted delivery |
| Animal Models | Humanized mice [95] | Preclinical immunogenicity testing | Human immune system components; Predictive of human responses |
| Control Reagents | Nontargeting sgRNAs [96] | Control for off-target immune effects | Validated lack of genomic target; Baseline for immune activation studies |
The journey toward safe and effective CRISPR-based therapies requires comprehensive strategies to address immune recognition of bacterial-derived editing components. Significant progress has been made in developing minimally immunogenic Cas variants, optimized delivery systems such as lipid nanoparticles, and chemical modifications to prevent guide RNA-mediated immune activation. The successful application of these approaches is evidenced by recent clinical trials where CRISPR therapies have demonstrated durable effects without evidence of immune-mediated clearance [7] [97].
As the field advances, the integration of multiple mitigation strategies—combining engineered nucleases, optimized delivery vehicles, and selective immunosuppression—will likely provide the most robust solution to immune challenges. Furthermore, continued refinement of preclinical immunogenicity assessment protocols will enable better prediction of human immune responses. These developments collectively support the tremendous potential of CRISPR genome editing to yield safe, effective, and durable therapies for a wide range of genetic diseases.
Confirming Your Edits: A Guide to CRISPR Analysis and Validation Methods
The advent of CRISPR-Cas9 gene editing technology has undeniably revolutionized the landscape of genetic research and therapeutic applications, providing an unprecedented ability to precisely modify specific genomic loci [98]. However, the full potential of this revolutionary tool can only be harnessed with robust assessment and quality control measures to ensure the accuracy and safety of genomic manipulations [98]. Next-Generation Sequencing (NGS) has emerged as the gold-standard technology for this comprehensive evaluation, offering a high-throughput, precise, and scalable platform for analyzing CRISPR-edited genomes [98] [99]. Unlike inference-based methods that estimate editing events, NGS provides a direct, nucleotide-resolution view of editing outcomes, enabling researchers to move from asking "Did editing occur?" to "What specific sequence changes occurred, and how frequently?" [99] [100]. This in-depth technical guide outlines the critical role of NGS in validating CRISPR experiments, detailing specific methodologies for detecting on-target and off-target effects, quantifying efficiency, and integrating advanced quality control techniques within the context of modern genomic research and drug development.
The Critical Applications of NGS in CRISPR Analysis
NGS technologies empower a multi-faceted assessment of CRISPR experiments, moving beyond simple efficiency checks to a full characterization of editing outcomes. The primary applications are summarized in the table below.
Table 1: Core Applications of NGS in CRISPR Genome Editing Analysis
| Application Area | Key Objective | NGS Approach | Data Output |
|---|---|---|---|
| On-Target Analysis | Precise characterization of intended edits at the target site [98] [99] | Targeted Amplicon Sequencing (e.g., rhAmpSeq) [99] | Spectrum and frequency of indels; HDR precision [98] |
| Off-Target Identification | Genome-wide discovery of unintended cleavage sites [98] [99] | Whole Genome Sequencing (WGS) or methods like GUIDE-seq, CIRCLE-seq [98] [99] | A list of nominated off-target sites with semi-quantitative editing frequencies [99] |
| Off-Target Quantification | Accurate measurement of editing frequency at known potential off-target sites [99] | Targeted Amplicon Sequencing [99] | Precise quantification of indel percentages at specific loci [99] |
| Editing Efficiency | Measurement of the percentage of alleles successfully modified [98] | Amplicon Sequencing or Digital PCR combined with NGS [98] | Allele-specific quantification of editing rates [98] |
Comprehensive On-Target Analysis
NGS allows researchers to interrogate the targeted genomic region at base-pair resolution, enabling the precise detection of insertions, deletions (indels), and other sequence modifications introduced by CRISPR-Cas9 [98]. The most common method is targeted amplicon sequencing, where the edited genomic region is PCR-amplified, prepared as an NGS library, and deeply sequenced [99] [100]. This approach provides a complete picture of the editing landscape, revealing the exact sequences and relative abundance of all induced indels, which is crucial for applications like generating knockout models or verifying precise knock-ins [99]. Furthermore, long-read sequencing technologies can be employed to resolve complex structural variations and allelic phasing, ensuring unambiguous annotation of edited loci [98].
Unbiased Off-Target Effect Profiling
A significant concern in CRISPR applications is the potential for off-target effects—unintended edits at genomic sites with sequence similarity to the target [98]. NGS-based strategies are indispensable for identifying these events. While whole-genome sequencing (WGS) can theoretically detect off-targets anywhere in the genome, its sensitivity in a therapeutic context can be limited by cost and depth of sequencing [99]. Consequently, more sensitive, unbiased in vitro and in vivo methods have been developed to nominate potential off-target "hotspots" empirically:
- GUIDE-seq: Uses integration of a oligodeoxynucleotide tag into double-strand breaks (DSBs) in vivo to report the locations of CRISPR-Cas9 cleavage sites across the genome [99].
- CIRCLE-seq: A highly sensitive in vitro method that uses circularized genomic DNA to profile the nuclease activity of Cas9, capable of detecting even rare off-target sites [99].
- DISCOVER-Seq: An in vivo method that relies on the recruitment of DNA repair factors (e.g., MRE11) to DSB sites to identify off-target cleavages [99].
Once potential off-target sites are nominated, targeted amplicon sequencing is used for accurate quantification of editing frequencies at those specific loci, providing a complete risk assessment [99].
Precise Quantification of Editing Efficiency
Accurate quantification of editing efficiency is vital for optimizing CRISPR-Cas9 experiments and assessing the impact of various experimental parameters [98]. NGS-based approaches, particularly amplicon sequencing, enable digital allele quantification. By counting the number of sequence reads containing a specific edit versus wild-type reads, researchers can determine the precise percentage of edited alleles within a heterogeneous cell population [98]. This high-resolution data is essential for titrating editing reagents, comparing the efficacy of different guide RNAs, and ensuring that therapeutic editing meets a minimum threshold for biological effect.
Experimental Protocols for NGS-Based CRISPR Analysis
Protocol 1: Targeted Amplicon Sequencing for On-Target and Off-Target Quantification
This protocol is used for the precise characterization and quantification of edits at a predefined set of sites (e.g., the on-target site and a panel of nominated off-target sites) [99].
- DNA Extraction: Isolate high-quality genomic DNA from CRISPR-treated and control cells.
- Amplicon Library Design: Design PCR primers to amplify ~200-300 bp regions flanking each target site. Incorporate universal sequencing adapters and sample barcodes into the primer designs.
- Library Amplification: Perform PCR to amplify the target regions from all samples. Using a technology like rhAmpSeq can improve specificity by reducing primer-dimer formation [99].
- Library Pooling and Purification: Combine the amplified products from multiple samples and target sites into a single pool. Purify the pooled library to remove primers and enzymes.
- Sequencing: Load the library onto an NGS platform (e.g., Illumina) for high-depth sequencing (often >100,000x coverage per site) to detect low-frequency events.
- Bioinformatic Analysis:
- Demultiplexing: Assign sequences to individual samples based on their unique barcodes.
- Alignment: Map sequence reads to the reference genome.
- Variant Calling: Use specialized algorithms (e.g., those in the rhAmpSeq analysis pipeline or MAGeCK) to identify and quantify indels at each target site relative to the control [101] [99].
Protocol 2: Genome-Wide Off-Target Discovery with GUIDE-seq
This protocol is used for unbiased identification of off-target sites in relevant cell lines [99].
- Co-delivery: Co-transfect cells with the CRISPR-Cas9 components (e.g., Cas9/sgRNA RNP) and the GUIDE-seq oligonucleotide.
- Genomic DNA Extraction: Harvest genomic DNA 48-72 hours post-transfection.
- Library Preparation for GUIDE-seq:
- Fragment the genomic DNA.
- Ligate sequencing adapters to the fragments.
- Perform a pull-down enrichment for fragments containing the integrated GUIDE-seq oligo.
- Amplify the enriched library by PCR.
- Sequencing and Analysis: Sequence the library and use the published GUIDE-seq computational pipeline to identify genomic locations where the oligo was integrated, indicating a CRISPR-Cas9-induced double-strand break.
The Scientist's Toolkit: Essential Reagents and Solutions
Successful NGS-based CRISPR analysis relies on a suite of specialized reagents and tools. The following table details key components for building a robust workflow.
Table 2: Research Reagent Solutions for NGS-based CRISPR Analysis
| Item | Function | Example/Note |
|---|---|---|
| CRISPR Nucleases | Introduces targeted double-strand breaks | Alt-R S.p. Cas9 Nuclease V3 (for NGG PAM sites); Alt-R Cas12a (Cpf1) Ultra (for T-rich PAMs) [99] |
| Targeted Amplicon System | Multiplexed PCR for sequencing library preparation | rhAmpSeq CRISPR Analysis System enables highly specific amplification of multiple on- and off-target sites [99] |
| NGS Platform | High-throughput sequencing | Illumina sequencing systems are the most common platform for this application [99] |
| Bioinformatics Software | Data analysis, alignment, and variant calling | MAGeCK [101]; CRISPRCloud2 [101]; commercial pipelines (e.g., from IDT) [99] |
| Off-Target Discovery Kit | Unbiased identification of off-target sites | GUIDE-seq kit for Cas9; DISCOVER-Seq may be preferred for Cas12a [99] |
NGS Data Analysis and Bioinformatics
The deluge of data generated by NGS necessitates robust bioinformatic pipelines to process and interpret sequencing reads accurately [98]. The general workflow includes:
- Sequence Quality Assessment and Read Alignment: Initial processing to ensure data quality and map sequences to the reference genome [101].
- Read Count Normalization: Adjusting for differences in library size and distribution [101].
- sgRNA Abundance Estimation: Quantifying the representation of each targeted site.
- Statistical Analysis for Gene Ranking: Using algorithms to determine which genes or sites show statistically significant enrichment or depletion of edits. Common tools and methods include:
- MAGeCK (Model-based Analysis of Genome-wide CRISPR/Cas9 Knockout): Uses a negative binomial distribution and a Robust Rank Aggregation (RRA) method to identify significantly enriched or depleted sgRNAs [101].
- BAGEL: A Bayesian algorithm that uses a reference set of essential and non-essential genes to calculate a Bayes factor for each gene [101].
- EdgeR/DESeq2: Repurposed RNA-seq analysis packages that can be applied to model read count over-dispersion in CRISPR screens [101].
Table 3: Common Bioinformatics Tools for CRISPR Screen Analysis
| Tool | Year | Key Statistical Method | Best For |
|---|---|---|---|
| MAGeCK | 2014 | Negative Binomial + Robust Rank Aggregation (RRA) [101] | Genome-wide knockout and activation screens [101] |
| BAGEL | 2016 | Bayesian Analysis with Reference Gene Sets [101] | Knockout screens with a focus on essential genes [101] |
| CRISPhieRmix | 2018 | Hierarchical Mixture Model [101] | Analyzing screens with weaker effect sizes [101] |
| JACKS | 2019 | Bayesian Hierarchical Modeling [101] | Inferring single-guide and gene-level effects precisely [101] |
NGS Workflow Visualization
The following diagram illustrates the logical workflow for a comprehensive NGS-based analysis of a CRISPR experiment, integrating both on-target and off-target assessments.
Next-Generation Sequencing has firmly established itself as the indispensable tool for the comprehensive analysis of CRISPR genome editing experiments. Its unparalleled precision, sensitivity, and scalability provide researchers and drug developers with the depth of information required to confidently characterize on-target edits, identify and quantify off-target effects, and measure editing efficiency [98] [99]. As CRISPR technology continues to evolve toward more complex therapeutic applications, the integration of NGS with advanced bioinformatics and quality control measures will be paramount to ensuring the development of safe and effective genetic therapies [98] [102]. By adopting the NGS gold standard, the scientific community can continue to harness the transformative power of CRISPR with the necessary rigor, paving the way for a new era of precision medicine and biotechnology.
The advent of CRISPR-Cas9 genome editing has revolutionized biological research by providing scientists with a precise and programmable method for making targeted changes to DNA sequences [64] [11]. This bacterial immune system, harnessed for use in eukaryotic cells, functions like molecular scissors that create double-strand breaks at specific locations in the genome guided by a short RNA sequence [103]. When the cell repairs this break, it can introduce mutations—typically small insertions or deletions (indels)—through the error-prone non-homologous end joining (NHEJ) pathway [64]. The efficiency of this process is crucial for successful gene editing experiments, creating an essential need for robust, accessible methods to quantify these editing outcomes.
For researchers, particularly those new to the field, analyzing the results of CRISPR experiments presents a significant challenge. While Sanger sequencing remains the gold standard for accurate DNA sequencing [104] [105], interpreting its output to quantify CRISPR editing efficiency traditionally required sophisticated bioinformatic skills or expensive next-generation sequencing approaches. In response to this gap, computational tools ICE (Inference of CRISPR Edits) and TIDE (Tracking of Indels by Decomposition) were developed to democratize access to CRISPR analysis [106] [107]. These methods enable researchers to obtain quantitative, next-generation sequencing-quality data from standard Sanger sequencing traces, making robust CRISPR analysis accessible to laboratories without specialized sequencing infrastructure or bioinformatics expertise [108].
Understanding Sanger Sequencing Fundamentals
Principles of Sanger Sequencing Data Generation
Sanger sequencing, developed by Frederick Sanger in 1977, operates on the principle of chain-terminating dideoxynucleotides [105]. The method involves synthesizing a complementary DNA strand using a DNA polymerase enzyme, template DNA, and a primer, with the key addition of fluorescently labeled dideoxynucleotides (ddNTPs) that randomly terminate DNA strand extension [104]. The resulting fragments are separated by size using capillary electrophoresis, with a laser detecting the fluorescent label at the end of each fragment [109]. The output is a chromatogram (also called an electropherogram), which displays peaks of four colors corresponding to the four bases (A, T, C, G) along the sequence [109].
The quality of Sanger sequencing data is not uniform across the entire read. The initial 20-40 bases typically show poor resolution, while the region between 100-500 bases provides the most reliable data with sharp, well-spaced peaks [109]. Toward the end of the trace, peaks become less defined and lower in intensity due to decreased efficiency in generating larger sequencing products [109]. Understanding these quality considerations is essential for proper experimental design in CRISPR editing analysis, particularly in ensuring that the target region falls within the high-quality portion of the sequence read.
Interpreting Chromatogram Quality Metrics
Several quality metrics help researchers evaluate the reliability of Sanger sequencing data. The Quality Value (QV) is assigned to each base and is logarithmically related to the base-calling error probability (e.g., QV = 20 indicates a 1% error probability) [109]. The Quality Score (QS) represents the average QV for all bases in the trace, with values ≥ 40 indicating good quality data [109]. The Continuous Read Length (CRL) identifies the longest stretch of bases with a running QV average of 20 or higher, with values above 500 associated with high-quality data for plasmid samples and PCR products [109].
Table 1: Key Quality Metrics for Sanger Sequencing Data Interpretation
| Metric | Description | Interpretation Guidelines |
|---|---|---|
| Quality Value (QV) | Logarithmic measure of base-calling accuracy | QV ≥ 20: High confidenceQV < 10: Base called as 'N' |
| Quality Score (QS) | Average QV for all bases in trace | QS ≥ 40: Good qualityQS ~30: Requires scrutinyQS < 20: Poor quality |
| Continuous Read Length (CRL) | Longest stretch with running QV average ≥ 20 | CRL > 500: High quality for plasmids/PCR products |
| Signal Intensity | Average fluorescence intensity | >1000: Robust reaction>100: Noisy traces>10,000: Potential oversaturation |
ICE and TIDE: Core Methodologies and Workflows
TIDE (Tracking of Indels by Decomposition)
TIDE was developed as a simple and accurate method for determining the spectrum and frequency of targeted mutations generated by CRISPR-Cas9, TALENs, and ZFNs [106]. The method is specifically designed for non-templated editing where no donor DNA template is provided, resulting in indels formed through NHEJ repair [106]. The TIDE workflow requires only two Sanger sequencing traces—one from the edited cell pool and one from a wild-type control [106]. The algorithm decomposes the complex sequencing trace from the edited sample by comparing it to the wild-type reference, quantitatively reconstructing the spectrum of indels around the cut site and reporting their identities and frequencies [106].
A related method, TIDER, extends this capability for template-directed editing where a donor DNA template is used to introduce specific mutations through homology-directed repair (HDR) [106]. TIDER requires three sequencing traces—the edited sample, wild-type control, and a special "reference" sample that incorporates the desired templated mutation—and quantifies both the templated mutations and the non-templated indels [106].
ICE (Inference of CRISPR Edits)
ICE is a similarly powerful tool developed by Synthego that provides NGS-quality analysis from Sanger sequencing data at a fraction of the cost [107]. ICE analyzes Sanger sequencing files by comparing edited and control samples after the user inputs the guide RNA (gRNA) sequence and selects the nuclease used [107]. The algorithm calculates overall editing efficiency and determines the profiles and relative abundances of different edit types present in the sample [107]. Unlike earlier tools, ICE can analyze more complex editing experiments, including those using multiple gRNAs simultaneously and various nucleases such as SpCas9, hfCas12Max, Cas12a, and MAD7 [107].
ICE provides several key metrics, including Indel Percentage (editing efficiency), Model Fit (R²) Score (confidence in the ICE score), Knockout Score (proportion of cells with frameshift or 21+ bp indel), and Knock-in Score (proportion of sequences with desired knock-in edit) [107]. These metrics give researchers comprehensive insight into both the efficiency and functional consequences of their editing experiments.
Diagram 1: CRISPR workflow with ICE/TIDE analysis (43 characters)
Comparative Analysis of ICE and TIDE
Performance and Accuracy Assessment
A systematic comparison of computational tools for Sanger-based CRISPR analysis published in 2024 revealed important insights into the performance characteristics of ICE and TIDE [108]. The study used artificial sequencing templates with predetermined indels to quantitatively assess tool accuracy, demonstrating that both tools estimate indel frequency with acceptable accuracy when indels are simple and contain only a few base changes [108]. However, the estimated values became more variable among tools when sequencing templates contained complex indels or when indel frequencies were in low or high ranges [108].
The study found that while all tools accurately estimated net indel sizes, their capabilities for deconvoluting specific indel sequences varied with certain limitations [108]. For knock-in analysis of short epitope tag sequences, TIDE-based TIDER outperformed other tools [108]. Among the tools evaluated, DECODR provided the most accurate estimations of indel frequencies for most samples, though each tool had specific strengths depending on the editing context [108].
Table 2: Comparative Analysis of ICE and TIDE Capabilities
| Feature | TIDE | ICE |
|---|---|---|
| Primary Application | Non-templated editing (TIDE)Template-directed editing (TIDER) | Knockout and knock-in analysis |
| Input Requirements | 2 traces (TIDE)3 traces (TIDER) | Edited + control traces + gRNA sequence |
| Nuclease Support | CRISPR-Cas9, TALENs, ZFNs | SpCas9, hfCas12Max, Cas12a, MAD7 |
| Key Output Metrics | Indel spectrum and frequenciesTemplated mutation frequency (TIDER) | Indel percentage, KO/KI scoresModel fit (R²) |
| Complex Editing Analysis | Limited | Multiple gRNAs simultaneously |
| Strengths | Accurate for simple indelsSuperior for knock-in quantification | Broader nuclease supportBatch analysis capability |
Practical Implementation Guidelines
For researchers implementing these tools, specific experimental protocols are critical for success. The genotyping protocol for ICE analysis involves careful primer design, genomic DNA extraction, and PCR amplification of the target region [107]. Primers should be designed to bind at least 60-100 bp away from the key base of interest to ensure the target region falls within the high-quality portion of the sequencing read [109]. For PCR amplification, using high-fidelity DNA polymerases with proofreading capabilities helps minimize amplification errors that could compromise sequencing accuracy [105].
When preparing samples for Sanger sequencing, researchers should optimize PCR conditions—including annealing temperature, extension duration, and primer concentrations—to ensure efficient and precise amplification of the target DNA template [105]. After sequencing, careful inspection of the chromatogram quality metrics is essential before proceeding with ICE or TIDE analysis. Traces with average quality scores (QS) below 30 require extra scrutiny, and those with QS below 20 are likely to have issues that could compromise analysis accuracy [109].
Integration with CRISPR Genome Editing Workflows
Successful CRISPR genome editing followed by ICE/TIDE analysis requires several key reagents and resources. The core components include the Cas nuclease (e.g., SpCas9, Cas12a), which cleaves the target DNA; guide RNA molecules that direct Cas to the specific genomic target; and target cells or organisms for editing [64] [103]. For analysis, researchers need PCR reagents for target amplification, Sanger sequencing services or capabilities, and access to either the ICE web tool or TIDE web tool [106] [107].
Table 3: Essential Research Reagent Solutions for CRISPR Analysis
| Reagent/Resource | Function | Implementation Considerations |
|---|---|---|
| Cas Nuclease | Creates double-strand breaks at target DNA sites | Choice affects PAM requirement and editing efficiency |
| Guide RNA (gRNA) | Directs Cas nuclease to specific genomic target | Sequence quality crucial for specificity and efficiency |
| PCR Reagents | Amplifies target region from genomic DNA | High-fidelity polymerases reduce amplification errors |
| Sanger Sequencing | Generates sequence traces for analysis | Quality metrics must meet minimum thresholds |
| ICE/TIDE Web Tools | Quantifies editing efficiency and indel spectra | Input requirements vary between platforms |
Applications in Gene Editing Assessment
ICE and TIDE find particular utility in assessing two main types of CRISPR editing outcomes: knockout and knock-in experiments. For knockout studies, where the goal is to disrupt gene function by introducing frameshift mutations, the key metric is the Knockout Score provided by ICE, which represents the proportion of cells with either a frameshift or 21+ bp indel [107]. This score helps researchers understand how many editing events are likely to result in functional gene knockout.
For knock-in experiments, where a specific DNA sequence is introduced using a donor template, the Knock-in Score from ICE or TIDER's quantification of templated mutations provides the critical measure of success [106] [107]. After obtaining these computational predictions, researchers are advised to perform downstream protein-level validation (e.g., Western blots for knockouts or functional assays for knock-ins) to confirm the phenotypic consequences of editing [107].
Diagram 2: ICE/TIDE data processing workflow (41 characters)
The Evolving Landscape of CRISPR Analysis
The field of CRISPR genome editing continues to advance rapidly, with new technologies like base editing and prime editing offering more precise genetic modifications without requiring double-strand breaks [11] [110]. As these technologies mature, analysis methods like ICE and TIDE will need to evolve to quantify their distinct editing outcomes. The 2024 systematic comparison of computational tools highlights that while current methods perform well for simple edits, there remains variability in analyzing complex indels, suggesting areas for future algorithm improvement [108].
The integration of machine learning approaches may further enhance the accuracy of Sanger-based analysis tools, potentially allowing them to extract even more information from standard sequencing traces. Additionally, as CRISPR applications expand beyond basic research into therapeutic development [110], the demand for robust, accessible, and cost-effective analysis methods will only increase.
ICE and TIDE represent significant advancements in making CRISPR genome editing analysis accessible to researchers across disciplines and resource settings. By transforming standard Sanger sequencing data into quantitative assessments of editing efficiency and indel spectra, these tools bridge the gap between simple gel-based assays and expensive next-generation sequencing. For new researchers entering the field of CRISPR genome editing, mastering these accessible analysis methods provides a foundation for rigorous experimental validation while maintaining cost-effectiveness and workflow efficiency. As the CRISPR toolbox continues to expand, these accessible analysis alternatives will play an increasingly important role in empowering researchers to precisely characterize their gene editing outcomes.
Clustered Regularly Interspaced Short Palindromic Repeat (CRISPR)-based technologies have revolutionized genome engineering, becoming a cornerstone technique in both fundamental research and clinical applications for their remarkable efficiency and versatility [111]. The CRISPR-Cas9 system, originating from an adaptive immune system in Streptococcus pyogenes, functions by creating targeted double-strand breaks (DSBs) in DNA at sequences specified by a guide RNA (gRNA) [13]. The cell's subsequent repair of these breaks, primarily via the error-prone non-homologous end joining (NHEJ) pathway, often results in small insertions or deletions (indels) that can disrupt gene function [13] [112].
However, not all designed gRNAs are equally effective; their activity can be influenced by factors such as sequence context, chromatin structure, and GC content [113]. Consequently, validating the success and efficiency of the editing process is a critical step in any CRISPR workflow. Among the various methods developed for this purpose, the T7 Endonuclease I (T7E1) mismatch detection assay stands out as a widely used tool for the rapid, initial screening of editing events, despite its well-characterized limitations [113] [114]. This guide provides an in-depth technical examination of the T7E1 assay, detailing its mechanism, protocol, and appropriate place within a researcher's CRISPR validation toolkit.
The T7E1 Assay: Mechanism and Workflow
Core Principle and Molecular Mechanism
The T7 Endonuclease I is a structure-selective enzyme derived from bacteriophage T7 that recognizes and cleaves imperfect base pairs in heteroduplexed DNA [113] [115]. Its application in CRISPR validation capitalizes on this property to detect the presence of indel mutations introduced by NHEJ repair.
The fundamental principle is as follows: after CRISPR editing, a pool of cells contains a mixture of wild-type alleles and mutant alleles with small indels. When the genomic region surrounding the target site is amplified by PCR, the products include homoduplexes (wild-type/wild-type or mutant/mutant) and, crucially, heteroduplexes formed when a wild-type DNA strand anneals with an indel-containing strand [111] [115]. The insertion or deletion in one strand creates a structural distortion—a mismatch or an extrahelical loop—in the otherwise double-stranded DNA. The T7E1 enzyme specifically binds to and cleaves at the 5' base of these distorted structures, generating discrete DNA fragments that can be resolved and quantified via gel electrophoresis [111] [113]. The editing efficiency is then semi-quantitatively estimated based on the proportion of cleaved to uncleaved PCR product.
Detailed Experimental Protocol
The following workflow outlines the standard steps for performing the T7E1 assay, from sample preparation to analysis.
Diagram 1: T7E1 assay workflow for CRISPR validation.
Step-by-Step Methodology:
Genomic DNA Isolation and PCR Amplification: Harvest cells typically 3-4 days post-transfection with CRISPR components and extract genomic DNA. Amplify the target locus using primers that bind approximately 250 base pairs upstream and downstream of the expected cut site, generating a 400-800 base pair amplicon [115] [114]. It is critical to use a high-fidelity DNA polymerase (e.g., AccuTaq, Q5 Hot Start Master Mix) to minimize PCR-introduced errors that could lead to false positives [111] [114]. Include a PCR amplification from an unedited control sample.
Heteroduplex Formation: Purify the PCR products. To form heteroduplexes, denature the DNA by heating (e.g., 95°C for 5 minutes) and then slowly reanneal it by ramping the temperature down to room temperature slowly (e.g., -0.1°C per second) [114]. This process allows strands from different alleles (wild-type and mutant) to hybridize.
T7E1 Digestion: Incubate the reannealed DNA with the T7E1 enzyme in an appropriate reaction buffer (e.g., NEBuffer 2) at 37°C for 30 minutes [111]. The reaction is often performed in a small volume for efficient cleavage. The digestion is then stopped, typically by adding a chelating agent like EDTA.
Analysis via Gel Electrophoresis: Run the T7E1-treated samples, alongside an untreated PCR product control, on an agarose gel (1-2%) containing a DNA stain like Ethidium Bromide or GelRed [111]. Visualize the bands using a gel documentation system.
Calculation of Editing Efficiency: Use densitometric software (e.g., ImageJ) to measure the intensity of the DNA bands. The editing efficiency, representing the indel frequency, is calculated using the following formula [111]:
Indel Frequency (%) = [1 - (1 - (a + b)/(a + b + c))^{1/2}] × 100
Where:
c= intensity of the uncut (parental) banda + b= combined intensity of the cleavage product bands
Essential Research Reagent Solutions
Table 1: Key reagents and materials for the T7E1 assay.
| Reagent/Material | Function | Examples & Notes |
|---|---|---|
| T7 Endonuclease I | Mismatch-cleaving enzyme | Sold in kits from suppliers like New England Biolabs [111] or Sigma-Aldrich [114]. |
| High-Fidelity Polymerase | PCR amplification of target locus | Critical to prevent false positives from PCR errors. Examples: AccuTaq LA DNA Polymerase [114], Q5 Hot Start Master Mix [111]. |
| PCR Purification Kit | Clean-up of PCR amplicons | Used prior to heteroduplex formation to remove primers and dNTPs. |
| Gel Electrophoresis System | Separation and visualization of DNA fragments | Standard agarose gel equipment and DNA stains (Ethidium Bromide, GelRed) [111]. |
| Densitometry Software | Quantification of band intensities | Software like ImageJ or commercial gel imaging system software [116]. |
Performance and Limitations in CRISPR Validation
While popular for its simplicity, the T7E1 assay has significant limitations that researchers must consider when interpreting results.
Semi-Quantitative and Low Dynamic Range: The assay is not truly quantitative and its accuracy is limited, particularly at high editing efficiencies. A landmark study comparing T7E1 to targeted next-generation sequencing (NGS) revealed that T7E1 consistently underestimated editing efficiency. sgRNAs with >90% indel frequency by NGS appeared only modestly active by T7E1, and sgRNAs with similar T7E1 scores could have dramatically different actual efficiencies (e.g., 40% vs. 92%) [113]. The signal plateaus around 30-40%, making it unreliable for quantifying highly active sgRNAs [113].
Inability to Identify Specific Mutations: T7E1 only indicates that an indel has occurred; it provides no information on the exact sequence change [115] [114]. This is a critical shortcoming, as not all indels result in a functional knockout (e.g., in-frame deletions may still produce a functional protein) [116] [114].
Dependence on Heteroduplex Formation: The assay relies on the formation of wild-type/mutant heteroduplexes. Homoduplexes of mutant/mutant DNA, which can occur in highly edited or clonal populations, will not be cleaved, leading to an underestimation of the mutation rate [115].
Sensitivity to Reaction Conditions: Cleavage efficiency is affected by factors such as incubation time, temperature, salt concentration, and enzyme amount, requiring optimization for different conditions [115]. Furthermore, the enzyme has limited sensitivity for single-nucleotide polymorphisms and can be influenced by the sequence context surrounding the mismatch [113].
Comparison with Other Validation Methodologies
To contextualize the role of the T7E1 assay, it is essential to compare its performance against other common validation methods. The following table synthesizes quantitative and qualitative data from comparative studies [111] [113].
Table 2: Comparative analysis of CRISPR-Cas9 editing efficiency validation methods.
| Method | Quantitative Rigor | Indel Identification | Throughput | Relative Cost | Key Advantage | Key Disadvantage |
|---|---|---|---|---|---|---|
| T7E1 Assay | Semi-Quantitative | No | Low-Moderate | $ | Low cost and technical simplicity [115] | Low dynamic range, cannot identify specific edits [113] |
| TIDE/ICE | Quantitative | Yes (Decomposed) | Moderate | $$ | Good balance of cost, speed, and information [111] | Accuracy relies on sequencing quality; less effective for complex edits [111] [113] |
| ddPCR | Highly Quantitative | No (Predefined edits) | High | $$ | High precision and sensitivity for known edits [111] | Requires specific probe design; not for discovery [111] |
| Next-Generation Sequencing (NGS) | Highly Quantitative | Yes (Complete sequence) | High (Post-processing) | $$$ | Unbiased, comprehensive data on all edits and frequencies [113] | High cost, complex data analysis, longer turnaround [113] [114] |
Abbreviations: TIDE (Tracking of Indels by Decomposition); ICE (Inference of CRISPR Edits); ddPCR (droplet digital PCR).
As demonstrated, T7E1 is the least expensive and most technically straightforward option but provides the least amount of specific information. Sequencing-based methods (TIDE, ICE, NGS) offer superior quantification and detail, with NGS being the gold standard for comprehensive analysis [113].
Best Practices and Strategic Implementation
Recommendations for Accurate T7E1 Use
To maximize the reliability of T7E1 results, researchers should adopt the following best practices:
- Primer Design: Design primers to produce a 400-800 bp amplicon, with the target site located such that the cleaved products are both >100 bp and can be clearly resolved on a gel [115].
- Include Rigorous Controls: Always run the assay with an unedited (wild-type) control sample. This confirms that any observed cleavage is due to CRISPR-induced mutations and not natural sequence variations or PCR artifacts [114].
- Optimize Reaction Conditions: Titrate the amount of T7E1 enzyme and duration of digestion to ensure complete cleavage without non-specific activity. The addition of MnCl₂ has been reported to increase efficiency in some protocols [115].
- Pre-digestion to Enrich Mutants: For low-efficiency editing, consider pre-digesting genomic DNA with a restriction enzyme that cuts the wild-type sequence to reduce the background of wild-type alleles before PCR amplification [115].
Position in the CRISPR Workflow: A Screening Tool
The limitations of the T7E1 assay define its optimal role in the CRISPR validation pipeline. The following diagram illustrates a recommended workflow for validating CRISPR experiments, positioning T7E1 as an initial screening step.
Diagram 2: Recommended CRISPR validation workflow with T7E1 as a screening tool.
Given its speed and low cost, the T7E1 assay is best suited for the rapid screening of multiple sgRNAs to identify those with any detectable activity [111] [114]. A positive T7E1 result justifies the investment of further time and resources. However, any sgRNA deemed "active" by T7E1 must be followed up with a more rigorous, sequence-based method.
- For characterizing mixed cell pools: TIDE or ICE analysis of Sanger sequencing data provides a more quantitative and informative assessment of the distribution of indels in the population [111] [116].
- For definitive analysis, especially of clonal lines: Targeted NGS is the gold standard, providing a complete picture of all introduced mutations with high accuracy [113].
- For confirming functional knockout: Ultimately, DNA-level validation should be complemented by protein-level analysis (e.g., Western blot) or functional assays to confirm the loss of gene function, as indels do not always guarantee a null phenotype [116] [114].
The T7E1 mismatch detection assay remains a useful tool in the genome engineer's toolkit, primarily valued for its procedural simplicity, low cost, and rapid turnaround for initial screens. It provides a practical method for quickly triaging a set of sgRNAs to identify candidates worthy of deeper investigation. However, its role must be understood in the context of its significant limitations: it is semi-quantitative, possesses a low dynamic range that obscures high editing efficiencies, and crucially, fails to reveal the specific nature of the induced mutations. Therefore, while T7E1 can effectively serve as a first-pass filter, it should not be used as the sole or final validation method. Robust CRISPR experimental design mandates that T7E1 results be confirmed and refined by sequencing-based techniques like TIDE, ICE, or NGS, followed by phenotypic validation, to ensure accurate and reliable interpretation of genome editing outcomes.
For researchers embarking on CRISPR genome editing projects, selecting the appropriate analysis method is as critical as the editing experiment itself. The choice of validation technology directly impacts the reliability of results, experimental timelines, and resource allocation. This technical guide provides a comprehensive comparative analysis of the primary CRISPR analysis methods, focusing on the core dimensions of cost, throughput, and data depth to inform evidence-based decision-making for researchers and drug development professionals.
The fundamental goal of CRISPR analysis is to determine the efficiency and precision of genetic modifications introduced by the CRISPR-Cas system. When the CRISPR-Cas complex induces a double-strand break, cellular repair pathways result in either random insertions or deletions (indels) via non-homologous end joining (NHEJ) or precise edits via homology-directed repair (HDR) [1] [13]. Characterizing these outcomes requires specialized methodologies ranging from simple enzymatic tests to sophisticated sequencing approaches, each with distinct advantages and limitations.
Methodologies for CRISPR Analysis
Next-Generation Sequencing (NGS)
Overview: NGS represents the gold standard for CRISPR analysis, providing comprehensive, sequence-level data on editing outcomes through deep sequencing of target loci [100]. This high-throughput method enables precise characterization of indel spectra, multiplexed sample analysis, and detection of complex editing events.
Experimental Protocol: The typical workflow for targeted NGS analysis involves:
- DNA Extraction: Isolate genomic DNA from edited cells or organisms
- Primary PCR Amplification: Amplify target regions using gene-specific primers with partial Illumina adapter overhangs (Forward DS tag: 5′-CTACACGACGCTCTTCCGATCT-3′; Reverse DS tag: 5′-CAGACGTGTGCTCTTCCGATCT-3′) [117]
- Secondary PCR Amplification: Add complete Illumina adapter sequences and unique dual indices using indexed primers
- Library Pooling & Normalization: Combine amplified libraries in equimolar ratios
- Sequencing: Run on Illumina platforms (MiSeq, HiSeq) using 150-250 bp paired-end reads
- Bioinformatic Analysis: Process data through specialized tools like CRIS.py to quantify editing efficiencies and characterize mutations [117]
For large deletion screening, primer design requires a forward primer upstream of the 5′ break site and a reverse primer downstream of the 3′ break site. Successful deletion generates a smaller amplicon detectable by NGS [117].
Inference of CRISPR Edits (ICE)
Overview: ICE is a sophisticated computational tool from Synthego that uses Sanger sequencing data to deconvolve complex editing patterns and quantify indel frequencies [100]. It provides NGS-comparable accuracy (R² = 0.96 against NGS) at substantially lower cost and complexity.
Experimental Protocol:
- DNA Amplification: PCR-amplify the target region from edited and control samples
- Sanger Sequencing: Perform capillary sequencing of PCR products
- Data Upload: Submit sequencing chromatogram files (.ab1) to the web-based ICE platform
- Algorithmic Analysis: ICE software aligns edited sequences to reference traces, decomposing mixed signals into individual indel components
- Result Interpretation: Review ICE score (indel percentage), knockout score (frameshift frequency), and specific indel distributions
Tracking of Indels by Decomposition (TIDE)
Overview: TIDE represents an earlier generation decomposition method that estimates indel frequencies from Sanger sequencing traces through computational decomposition [100]. While cost-effective, it has limitations in detecting complex editing patterns compared to ICE.
Experimental Protocol:
- Sample Preparation: PCR-amplify and sequence target regions from control and edited populations
- Sequence Submission: Upload sequencing data to the TIDE web tool
- Parameter Optimization: Define decomposition window and guide RNA target site
- Statistical Analysis: TIDE decomposes sequencing traces to estimate indel percentages and provides statistical significance for identified mutations
T7 Endonuclease 1 (T7E1) Assay
Overview: The T7E1 assay is a rapid, non-sequencing method that detects CRISPR-induced mutations through enzymatic cleavage of heteroduplex DNA [100]. While cost-effective and fast, it provides limited quantitative data and no sequence-level information.
Experimental Protocol:
- PCR Amplification: Amplify the target region from edited and control samples
- DNA Denaturation & Renaturation: Heat-denature PCR products (95°C, 5 minutes) followed by slow reannealing to form heteroduplexes where indels create mismatches
- Enzymatic Digestion: Incubate with T7 Endonuclease I, which cleaves mismatched DNA duplexes
- Gel Electrophoresis: Separate cleavage products by agarose gel electrophoresis
- Band Analysis: Visualize and quantify cleavage fragments to estimate editing efficiency
Comparative Analysis of Performance Metrics
Quantitative Method Comparison
Table 1: Comprehensive Comparison of CRISPR Analysis Methods
| Method | Cost per Sample | Throughput | Data Depth | Detection Limit | Key Applications |
|---|---|---|---|---|---|
| NGS | High ($50-100) | High (96-1000+ samples/run) | Nucleotide-level resolution, full indel spectrum, multiplexing capability | <1% variant frequency | Validation of clinical edits, mechanistic studies, off-target detection |
| ICE | Medium ($10-20) | Medium (96 samples/run) | Indel percentage, specific mutation profiles, frameshift analysis | ~5% variant frequency | Routine lab validation, pilot studies, quality control |
| TIDE | Medium ($10-20) | Medium (96 samples/run) | Indel percentage, limited to predominant mutations | ~5-10% variant frequency | Initial optimization, educational settings |
| T7E1 | Low ($5-10) | Low to Medium (manual processing) | Presence/absence of editing, semi-quantitative efficiency | ~10% variant frequency | Rapid screening during guide RNA optimization |
Performance Dimension Analysis
Cost Considerations: Next-generation sequencing carries the highest per-sample cost due to reagent expenses and bioinformatics infrastructure requirements [100]. Sanger-based methods (ICE, TIDE) reduce costs by approximately 60-80% by leveraging capillary sequencing infrastructure. The T7E1 assay provides the most economical option but trades cost savings for informational depth.
Throughput Capacity: NGS provides the highest multiplexing capability, with modern platforms processing thousands of amplicons simultaneously through dual indexing strategies [117] [118]. ICE and TIDE throughput is constrained by Sanger sequencing capacity, typically processing 96 samples per run. T7E1 throughput is limited by manual gel electrophoresis steps.
Data Depth and Quality: NGS delivers nucleotide-level resolution, enabling comprehensive characterization of editing outcomes, including precise indel sequences, their relative frequencies, and complex patterns such as large deletions [117] [100]. ICE provides detailed indel characterization without single-base resolution, while TIDE offers less comprehensive decomposition. T7E1 provides minimal sequence information, detecting only that editing has occurred.
Experimental Workflow Visualization
Diagram 1: Comparative workflows for major CRISPR analysis methods highlighting divergent paths after initial DNA extraction.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for CRISPR Analysis
| Reagent/Category | Function | Example Products |
|---|---|---|
| PCR Enzymes | Amplification of target loci for sequencing or analysis | MyTaq Red Mix, Platinum SuperFi II Master Mix [117] |
| NGS Library Prep Kits | Preparation of sequencing libraries for Illumina platforms | Illumina TruSeq DNA PCR-Free, Nextera XT [117] |
| CRISPR Analysis Software | Bioinformatics analysis of editing outcomes | CRIS.py, CRISPR-finder, ICE, TIDE [117] [100] [118] |
| Enzymatic Assay Kits | T7E1 mismatch detection | Surveyor Mutation Detection Kit, T7 Endonuclease I [100] |
| Quantitation Reagents | Accurate DNA concentration measurement for library normalization | Quant-iT PicoGreen dsDNA Assay [118] |
| Purification Kits | Cleanup of PCR products and libraries | AMPure XP beads, QIAquick PCR Purification Kit |
Strategic Implementation Guidelines
Method Selection Framework
Choose analysis methods based on these strategic considerations:
For Therapeutic Development & Clinical Applications: Implement NGS as the primary validation method, particularly utilizing single-cell DNA sequencing platforms like Tapestri for characterizing triple-edited cells simultaneously at multiple loci [119]. This approach provides comprehensive assessment of editing zygosity, structural variations, and cell clonality essential for regulatory compliance.
For Functional Genomics Screens: Employ pooled CRISPR screens analyzed through specialized algorithms like MAGeCK, PinAPL-Py, or CRISPRcleanR [120]. These tools identify hit genes by comparing guide RNA abundance between treated and control populations, with proper normalization critical for accurate results.
For Agricultural & Industrial Biotechnology: Utilize CRISPR-finder for high-throughput genotyping of plant and microbial strains [118]. This cost-effective NGS approach efficiently processes thousands of individuals in a single sequencing run through a streamlined two-step PCR barcoding system.
Emerging Technologies and Future Directions
The CRISPR analysis landscape continues to evolve with several promising developments:
- Single-Cell Sequencing: Technologies like Tapestri enable unprecedented resolution of editing outcomes in heterogeneous cell populations [119]
- Automated Platforms: Integrated robotic systems perform hundreds of CRISPR protocols simultaneously with AI-optimized guide RNA design [121]
- Advanced Algorithms: Continuous improvement in bioinformatic tools increases detection accuracy and reduces false positives in screen analysis [120]
Selecting the appropriate CRISPR analysis method requires careful consideration of project goals, resources, and required data quality. Next-generation sequencing provides the most comprehensive data for critical applications but demands significant infrastructure investment. Decomposition methods like ICE offer an optimal balance of cost and information for routine laboratory work, while T7E1 assays serve well for initial screening. By aligning methodological capabilities with experimental objectives, researchers can optimize their CRISPR validation strategies to advance therapeutic development, basic research, and agricultural applications efficiently and reliably.
The advent of CRISPR genome editing has revolutionized genetic research and therapeutic development, providing scientists with an unprecedented ability to modify DNA sequences with precision. While confirming the presence of intended genetic modifications—a process known as genotyping—represents a crucial first step, it constitutes merely the beginning of a comprehensive functional validation workflow. Functional validation extends beyond sequence verification to assess the downstream biological consequences of genetic perturbations, including changes in gene expression, protein function, and cellular behavior [122]. This systematic approach to phenotypic assessment is indispensable for establishing causal relationships between genetic modifications and their functional outcomes, thereby bridging the gap between genotype and phenotype.
The necessity for robust functional validation protocols stems from several technical challenges inherent to CRISPR editing. Despite high on-target efficiency, editing outcomes can be heterogeneous, with only a fraction of cells successfully incorporating the desired modification [123]. Furthermore, nonspecific transcriptional changes and cellular responses to the editing process itself can confound phenotypic readouts, creating artifacts that may be misinterpreted as genuine functional effects [123]. Advanced single-cell analyses have revealed that even in successfully transfected cell populations, a significant proportion may lack the intended edit, necessitating techniques that can directly link genotypic and phenotypic information at the single-cell level [123].
Within the context of drug development and therapeutic applications, functional validation provides critical evidence supporting mechanism of action, efficacy, and safety. As CRISPR-based therapies progress through clinical trials, comprehensive functional characterization becomes paramount for regulatory approval and understanding patient responses [7]. This technical guide outlines established and emerging methodologies for functional validation, providing researchers with a framework to confidently assess the phenotypic outcomes of their CRISPR experiments.
Multi-Modal Assessment of Phenotypic Outcomes
Successful functional validation requires interrogating phenotypic changes across multiple molecular levels, from transcriptomic alterations to functional cellular behaviors. The integration of these complementary data types provides a comprehensive understanding of editing outcomes.
Transcriptomic and Proteomic Profiling
Gene expression analysis represents a fundamental approach for assessing functional consequences of CRISPR interventions. Quantitative PCR (qPCR) offers a targeted method for evaluating expression changes in specific genes of interest, while RNA sequencing provides an unbiased assessment of global transcriptional changes [122]. For investigations of non-coding regions, CRISPR tools can be adapted to modulate gene expression without altering DNA sequence through CRISPR interference (CRISPRi) with repressive domains like KRAB, or CRISPR activation (CRISPRa) with activator domains like VP64 [124]. These approaches enable functional characterization of regulatory elements by assessing their impact on gene expression.
At the protein level, western blotting enables direct quantification of protein abundance and can confirm the loss of target proteins in knockout experiments or detect modified proteins in knock-in approaches [125]. For higher-throughput protein expression analysis, antibody-derived tags (ADTs) sequenced alongside transcriptomes enable simultaneous profiling of numerous cell-surface proteins, providing multi-parametric characterization of cellular states [123].
Cellular Phenotyping and Functional Assays
Beyond molecular profiling, functional validation must assess how genetic perturbations impact cellular behavior and physiology. High-content screening (HCS) platforms automate the quantification of morphological features, protein localization, and subcellular structures, enabling sophisticated phenotypic characterization [125]. For example, HCS can automatically identify and quantify LC3B granules in CRISPR-edited cells to investigate autophagy pathways [125].
Cell culture studies monitoring viability, proliferation, and apoptosis provide crucial information about the functional consequences of gene editing, particularly when investigating essential genes or therapeutic applications [125]. For immune cells or other specialized cell types, functional assays might include measures of cytotoxicity, cytokine production, or migration capacity [126]. In the context of cancer research, edited cells can be subjected to drug sensitivity screens to identify genetic modifiers of treatment response [127].
Table 1: Functional Assays for Different Biological Questions
| Biological Question | Recommended Assays | Key Readouts |
|---|---|---|
| Gene Knockout Efficacy | Western blot, Flow cytometry, Immunofluorescence | Protein loss, Surface marker expression |
| Transcriptional Regulation | qPCR, RNA-seq, CRISPRa/CRISPRi | Gene expression changes, Enhancer/promoter activity |
| Cell Survival & Proliferation | MTT assay, Colony formation, Live-cell imaging | Viability, Growth kinetics, Clonogenic capacity |
| Subcellular Phenotypes | High-content screening, Immunocytochemistry | Organelle morphology, Protein localization |
| Therapeutic Efficacy | Cytotoxicity assays, Xenograft models, Patient-derived organoids | Tumor cell killing, Disease-relevant biomarkers |
Advanced Methodologies for Integrated Genotype-Phenotype Analysis
Traditional CRISPR validation approaches often analyze genotypes and phenotypes in separate experimental workflows, making it difficult to directly correlate editing outcomes with functional effects in individual cells. Recent methodological advances now enable simultaneous assessment of both parameters.
Single-Cell Multi-Omic Approaches
The CRAFTseq (CRISPR by ADT, flow cytometry and transcriptome sequencing) methodology represents a significant advancement in functional validation by enabling quad-modal analysis of individual cells [123]. This integrated approach sequences genomic DNA amplicons to confirm editing outcomes while simultaneously profiling the whole transcriptome and numerous cell-surface proteins, with additional indexing through flow cytometry-based cell hashing. By directly linking genotypic and phenotypic information within the same cell, CRAFTseq controls for confounding factors such as variable editing efficiency and nonspecific cellular responses, thereby increasing power to detect true functional effects [123].
The experimental workflow for CRAFTseq involves several key steps. First, edited cells are stained with oligonucleotide-conjugated antibodies targeting surface markers of interest. Cells are then sorted into multi-well plates, with each well receiving a unique cell hashing antibody to enable sample multiplexing. After lysis, targeted genomic regions are amplified through nested PCR, while mRNA is captured using barcoded oligo-dT primers. All modalities are then sequenced simultaneously, with bioinformatic demultiplexing assigning each read to its cell of origin [123]. This approach generates high-quality data, with studies reporting recovery of approximately 5,000 genes and 57,500 unique molecular identifiers per cell, alongside confident genotype calling in over 95% of cells analyzed [123].
Diagram 1: CRAFTseq multi-omic workflow for linking CRISPR edits to phenotypic outcomes in single cells. ADTs: antibody-derived tags.
In Vivo Functional Validation
While in vitro models provide valuable insights, ultimately many therapeutic applications require validation in living organisms. In vivo models enable researchers to assess how genetic modifications influence complex physiological processes, tissue function, and organismal phenotypes [127]. Several delivery methods facilitate in vivo CRISPR editing, including direct injection of Cas9 ribonucleoprotein complexes into zygotes for germline modifications, viral vector delivery for somatic editing, and lipid nanoparticle (LNP)-encapsulated mRNA for transient editing in specific tissues [127] [7].
Recent clinical advances highlight the importance of robust in vivo validation. For example, in vivo CRISPR therapies delivered via LNPs have demonstrated durable protein reduction in human trials for hereditary transthyretin amyloidosis (hATTR), with patients showing approximately 90% reduction in disease-related protein levels sustained over two years [7]. Notably, LNP delivery enables redosing capability, as demonstrated by multiple patients receiving additional infusions to increase editing efficacy—an approach not feasible with viral vectors due to immune concerns [7]. These clinical successes underscore how functional validation in whole organisms provides critical proof-of-concept for therapeutic applications.
Practical Implementation: From Experimental Design to Validation
Establishing Proper Experimental Controls
Robust functional validation requires carefully designed controls that account for potential confounding factors. Positive controls confirm that the experimental system is capable of detecting expected effects, while negative controls establish baseline measurements in unperturbed systems [125]. For CRISPR experiments specifically, essential controls include:
- Non-targeting sgRNAs: Guide RNAs with no perfect genomic matches control for non-specific effects of the CRISPR machinery itself [123].
- Untransfected cells: Identify changes attributable to cell culture conditions or experimental handling.
- Targeting controls: Guides targeting genes with known phenotypes verify editing efficiency and functional detection capability.
- Delivery controls: Cells exposed to delivery reagents (e.g., transfection agents, viral vectors) without CRISPR components control for delivery-associated toxicity [125].
Additionally, researchers should implement validation controls using fluorophore expression or antibiotic resistance to verify efficient delivery of CRISPR components [125]. For therapeutic applications, bystander cells within the same culture can serve as internal controls for distinguishing cell-autonomous from non-autonomous effects [123].
The Scientist's Toolkit: Essential Reagents and Methods
Table 2: Research Reagent Solutions for CRISPR Functional Validation
| Reagent/Method | Function | Application Notes |
|---|---|---|
| Synthetic sgRNA | Guides Cas nuclease to target sequence | Higher purity and editing efficiency than IVT; minimal off-target effects [15] |
| Anti-Cas9 Antibody | Detects Cas9 protein delivery and expression | Verify intracellular Cas9 presence via immunocytochemistry or western blot [125] |
| T7 Endonuclease I | Detects indel formation | Mismatch cleavage assay; rapid but lower resolution than sequencing [125] |
| Lipid Nanoparticles (LNPs) | In vivo delivery of editing components | Liver-tropic; enable redosing; used in clinical trials [7] |
| Cell Hashing Antibodies | Multiplexing samples for single-cell analysis | Oligo-tagged antibodies enable sample pooling in CRAFTseq [123] |
| Barcoded oligo-dT Primers | Single-cell RNA sequencing | Captures transcriptome alongside genomic edits in CRAFTseq [123] |
Clinical Translation and Therapeutic Validation
The ultimate test of functional validation comes with clinical translation, where CRISPR-based interventions must demonstrate both safety and efficacy in human patients. Recent clinical developments highlight both the promise and challenges of therapeutic genome editing.
Several CRISPR therapies have shown remarkable success in clinical trials. Casgevy, the first FDA-approved CRISPR-based medicine, demonstrates durable cure for sickle cell disease and transfusion-dependent beta thalassemia by modifying hematopoietic stem cells to reactivate fetal hemoglobin [7]. For in vivo applications, Intellia Therapeutics' LNP-delivered CRISPR therapy for hATTR achieved sustained protein reduction exceeding 90% in trial participants, with corresponding clinical improvement in disease symptoms [7]. These successes illustrate how robust preclinical functional validation translates to clinical efficacy.
However, clinical development also underscores the importance of comprehensive safety assessment. Recent reports of severe liver toxicity in a Phase 3 trial for a CRISPR-Cas therapy, resulting in trial suspension, highlight the critical need for thorough functional validation of both on-target and off-target effects [126]. Advanced detection methods like TEG-seq and BEAN have been developed to measure off-target cleavage events and model heterogeneous editing outcomes, providing improved safety profiling [125] [123].
The functional validation landscape continues to evolve with emerging technologies. Prime editing strategies have achieved up to 60% editing efficiency in patient-derived keratinocytes for junctional epidermolysis bullosa, with functional correction demonstrated through selective advantage of corrected cells in xenograft models [126]. Epigenome editing approaches using dCas9-effector fusions enable reversible modulation of gene expression without altering DNA sequence, as demonstrated by targeted chromatin modifications that bidirectionally control memory formation in neuronal populations [126]. These advanced applications further expand the scope of functional validation beyond conventional knockout and knock-in approaches.
Diagram 2: Multi-level functional validation framework from DNA to organismal phenotype. HCS: High-content screening.
Functional validation represents an indispensable component of CRISPR genome editing that extends far beyond confirmation of genetic modifications to comprehensive assessment of phenotypic outcomes. As CRISPR technologies evolve toward increasingly sophisticated applications—from AI-designed editors [52] to epigenetic modulation [126]—the methods for functional validation must similarly advance. The integration of multi-omic approaches like CRAFTseq, which simultaneously captures genomic, transcriptomic, and proteomic information from single cells, provides unprecedented resolution for linking genotypes to phenotypes [123].
For researchers embarking on CRISPR experiments, a tiered validation strategy is recommended, beginning with robust genotyping and progressing through molecular, cellular, and when appropriate, organismal phenotypic assessment. This comprehensive approach ensures that observed effects genuinely result from intended genetic modifications rather than technical artifacts or confounding factors. As the field progresses toward more therapeutic applications, thorough functional validation will remain the cornerstone of translating CRISPR promise into clinical reality, enabling researchers to confidently advance from genotyping to meaningful phenotypic outcomes.
Conclusion
CRISPR genome editing has firmly transitioned from a revolutionary concept to a clinically validated technology, as demonstrated by approved therapies for sickle cell disease and a robust pipeline of clinical trials for conditions ranging from genetic disorders to cardiovascular diseases. Mastery of this tool requires a solid grasp of its foundational mechanisms, a strategic approach to application and delivery, proactive troubleshooting of challenges like off-target effects, and rigorous validation of editing outcomes. The future of CRISPR is being shaped by trends such as AI-driven editor design, enhanced delivery systems like LNPs, and the refinement of more precise editing platforms such as base and prime editing. For new researchers, mastering these facets is the key to unlocking the full potential of CRISPR to drive the next wave of breakthroughs in biomedical research and therapeutic development.
References
- 1. Comparing Gene Editing Platforms: CRISPR vs. Traditional ... [https://blog.crownbio.com/comparing-gene-editing-platforms-crispr-vs-traditional-methods]
- 2. Precision gene editing: The power of CRISPR-Cas in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590234/]
- 3. A Comparative Review of Genetic Modification Tools for ... [https://nhsjs.com/2025/a-comparative-review-of-genetic-modification-tools-for-crop-improvement-efficiency-scalability-and-usability/]
- 4. Recent advances in therapeutic gene-editing technologies [https://www.sciencedirect.com/science/article/pii/S152500162500200X]
- 5. Ten CRISPR companies to watch in 2025 [https://www.labiotech.eu/best-biotech/crispr-companies/]
- 6. CMN Weekly (17 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-17-october-2025-your-weekly-crispr-medicine-news/]
- 7. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 8. AI-powered CRISPR could lead to faster gene therapies ... [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]
- 9. PAM identification by CRISPR-Cas effector complexes: diversified mechanisms and structures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6546366/]
- 10. What is CRISPR? A bioengineer explains - Stanford Report [https://news.stanford.edu/stories/2024/06/stanford-explainer-crispr-gene-editing-and-beyond]
- 11. What is CRISPR? [https://innovativegenomics.org/what-is-crispr/]
- 12. CRISPR Advancements for Human Health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11057861/]
- 13. CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 14. PAM sequences and considerations for CRISPR | IDT [https://www.idtdna.com/pages/education/decoded/article/importance-of-the-pam-sequences-in-crispr-cas9-gene-editing]
- 15. The Complete Guide to Understanding CRISPR sgRNA [https://www.synthego.com/guide/how-to-use-crispr/sgrna/]
- 16. White Paper: CRISPR/Cas9 Gene Editing [https://www.bioskryb.com/crispr-cas9-gene-editing/]
- 17. CRISPR-induced double-strand breaks trigger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6587125/]
- 18. CRISPR-Cas systems: Overview, innovations and applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7508700/]
- 19. The CRISPR tool kit for genome editing and beyond [https://www.nature.com/articles/s41467-018-04252-2]
- 20. HDR vs NHEJ: DNA Repair Pathway Comparison [https://invivobiosystems.com/crispr/hdr-vs-nhej/]
- 21. HDR vs. NHEJ: CRISPR Gene Editing Techniques [https://www.zeclinics.com/blog/hdr-vs-nhej-in-crispr-gene]
- 22. CRISPR-Cas9-mediated homology-directed repair for ... [https://www.sciencedirect.com/science/article/pii/S2162253124002312]
- 23. NHEJ vs HDR: Difference when Repairing CRISPR DSB [https://www.idtdna.com/pages/support/faqs/which-repair-pathway-is-most-commonly-used-to-repair-crispr-mediated-double-stranded-breaks-nhej-or-hdr]
- 24. Stimulation of CRISPR-mediated homology-directed repair ... [https://www.nature.com/articles/s41467-019-11105-z]
- 25. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 26. A Comprehensive Guide on CRISPR Methods [https://www.synthego.com/guide/crispr-methods/]
- 27. CRISPR-Cas9 DNA Base-Editing and Prime-Editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7503568/]
- 28. CRISPR Base Editing Explained | ABE & CBE in Gene ... [https://www.synthego.com/crispr-base-editing-guide/]
- 29. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 30. Explainer: What Are Base Editors and How Do They Work? [https://crisprmedicinenews.com/news/explainer-what-are-base-editors-and-how-do-they-work/]
- 31. Comparative analysis of CRISPR off-target discovery tools ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10124080/]
- 32. Explainer: What Is Prime Editing and What Is It Used For? [https://crisprmedicinenews.com/news/explainer-what-is-prime-editing-and-what-is-it-used-for/]
- 33. Prime Editing: Adding Precision and Flexibility to CRISPR ... [https://blog.addgene.org/prime-editing-crisp-cas-reverse-transcriptase]
- 34. Prime Editing as a Precision Gene Editing Tool [https://www.synthego.com/guide/crispr-methods/prime-editing/]
- 35. Timeline: CRISPR-Cas9 [https://www.whatisbiotechnology.org/index.php/timeline/science/CRISPR-Cas9]
- 36. CRISPR Timeline [https://www.broadinstitute.org/what-broad/areas-focus/project-spotlight/crispr-timeline]
- 37. A Timeline of the CRISPR/Cas System [https://www.clinicallab.com/a-timeline-of-the-crispr-cas-system-24342]
- 38. FDA Approves First Gene Therapies to Treat Patients with ... [https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease]
- 39. CRISPR Therapeutics Highlights Strategic Priorities and ... [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-highlights-strategic-priorities-and]
- 40. CRISPR‐driven diagnostics: Molecular mechanisms, clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12464570/]
- 41. ensuring the social responsibility of CRISPR technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405698/]
- 42. CRISPR/Cas technologies for cancer drug discovery and ... [https://www.sciencedirect.com/science/article/abs/pii/S016561472500029X]
- 43. Comprehensive review of CRISPR-based gene editing [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01925-5]
- 44. Systematic discovery of CRISPR-boosted CAR T cell ... [https://www.nature.com/articles/s41586-025-09507-9]
- 45. CMN Weekly (26 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-26-september-2025-your-weekly-crispr-medicine-news/]
- 46. CMN Weekly (12 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-12-september-2025-your-weekly-crispr-medicine-news/]
- 47. Sickle Cell Gene Therapy Using CRISPR [https://www.synthego.com/crispr-sickle-cell-disease/]
- 48. Advances in β-Thalassemia Gene Therapy: CRISPR/Cas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562837/]
- 49. Gene Therapy Leads to Improved Quality of Life in Patients ... [https://www.hematology.org/newsroom/press-releases/2025/gene-therapy-leads-to-improved-quality-of-life]
- 50. CRISPR Therapeutics and Vertex Announce… [https://crisprtx.com/about-us/press-releases-and-presentations/crispr-therapeutics-and-vertex-announce-progress-in-clinical-development-programs-for-the-investigational-crispr-cas9-gene-editing-therapy-ctx001]
- 51. Gene therapy for sickle cell and β-thalassemia works by ... [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/gene-therapy-for-sickle-cell-and-beta-thalassemia-works-by-disrupting-three-dimensional-genome-structure.html]
- 52. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 53. A boost for the precision of genome editing [https://news.mit.edu/2025/boost-precision-genome-editing-0820]
- 54. In vivo delivery of CRISPR-Cas9 therapeutics - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8424283/]
- 55. Landscape of ex vivo gene therapies: Technological trends ... [https://www.sciencedirect.com/science/article/pii/S2329050125001755]
- 56. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 57. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 58. innovations and challenges in rAAV vector-based CRISPR ... [https://www.nature.com/articles/s41434-025-00573-2]
- 59. Viral and Non-Viral Systems to Deliver Gene Therapeutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11242246/]
- 60. Lipid Nanoparticles vs. Viral Vectors: A Comparison for ... [https://www.helixbiotech.com/post/lipid-nanoparticles-vs-viral-vectors-a-comparison-for-gene-therapy]
- 61. Comparative analysis of lipid Nanoparticle-Mediated ... [https://www.sciencedirect.com/science/article/pii/S093964112400033X]
- 62. Lipid nanoparticles allow efficient and harmless ex vivo gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10644071/]
- 63. Lung and liver editing by lipid nanoparticle delivery of a ... [https://www.nature.com/articles/s41587-024-02437-3]
- 64. Introduction to Gene Editing and Manipulation Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4963815/]
- 65. Novel Epigenetic Techniques Provided by the CRISPR/Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6079388/]
- 66. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 67. CRISPR-powered quantitative keyword search engine in ... [https://www.nature.com/articles/s41467-024-46767-x]
- 68. New CRISPR Toolkit to Allow Remote-Controlled Genome ... [https://viterbischool.usc.edu/news/2024/12/new-crispr-toolkit-to-allow-remote-controlled-genome-editing/]
- 69. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-announces-positive-phase-1-clinical-data]
- 70. First-in-human trial of CRISPR gene-editing therapy safely ... [https://newsroom.heart.org/news/first-in-human-trial-of-crispr-gene-editing-therapy-safely-lowered-cholesterol-triglycerides]
- 71. What are the most anticipated trials at ESC Congress 2025? [https://www.escardio.org/The-ESC/Press-Office/Press-releases/What-are-the-most-anticipated-trials-at-ESC-Congress-2025]
- 72. Rare Diseases in 2025: Diagnosis, Treatment & Policy [https://intuitionlabs.ai/articles/rare-disease-landscape-2025]
- 73. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 74. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 75. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 76. Recent Advancements in Reducing the Off-Target Effect of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10802171/]
- 77. High-fidelity CRISPR-Cas9 variants with undetectable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4851738/]
- 78. How to Choose the Right Cas Variant for Every CRISPR ... [https://www.synthego.com/guide/how-to-use-crispr/cas-nuclease-variants/]
- 79. Lipid nanoparticles: The game-changer in CRISPR-Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823087/]
- 80. New Nanostructure Enhances CRISPR Delivery [https://www.regmednet.com/new-nanostructure-enhances-crispr-delivery/]
- 81. Highly Targeted CRISPR Delivery Advances Gene Editing ... [https://innovativegenomics.org/news/envelope-delivery-vehicle/]
- 82. CRISPR Cell and Gene Therapies: Key Challenges in ... [https://www.synthego.com/blog/crispr-cell-gene-therapy-obstacles/]
- 83. CRISPR Clinical Trials to Follow [https://www.synthego.com/blog/crispr-clinical-trials/]
- 84. Genome Editing Market Report 2025: CRISPR and Beyond [https://finance.yahoo.com/news/genome-editing-market-report-2025-151500990.html]
- 85. Revolutionizing CRISPR technology with artificial intelligence [https://www.nature.com/articles/s12276-025-01462-9]
- 86. From Code to Life: The AI‐Driven Revolution in Genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376515/]
- 87. OpenCRISPR-1: Generative AI Meets CRISPR [https://crisprmedicinenews.com/news/opencrispr-1-generative-ai-meets-crispr/]
- 88. Profluent Modalities | Gene Editing [https://www.profluent.bio/modality/opencrispr]
- 89. Deep learning models simultaneously trained on multiple ... [https://www.nature.com/articles/s41467-025-65200-5]
- 90. Breaking: Deep learning multi-dataset training improves ... [https://crisprmedicinenews.com/news/breaking-deep-learning-multi-dataset-training-improves-crispr-base-editing-predictions/]
- 91. CRISPR-GPT for agentic automation of gene-editing ... [https://www.nature.com/articles/s41551-025-01463-z]
- 92. Stanford team creates AI gene editing tool 'CRISPR-GPT' [https://www.ddw-online.com/stanford-team-create-ai-gene-editing-tool-crispr-gpt-35864-202508/]
- 93. Cas9 immunity creates challenges for CRISPR gene ... [https://www.nature.com/articles/s41467-018-05843-9]
- 94. CRISPR RNAs trigger innate immune responses in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5848615/]
- 95. Scientists engineer CRISPR enzymes that evade ... [https://www.broadinstitute.org/news/scientists-engineer-crispr-enzymes-evade-immune-system]
- 96. Research Techniques Made Simple: CRISPR Genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8525197/]
- 97. Cleveland Clinic First-In-Human Trial of CRISPR Gene ... [https://newsroom.clevelandclinic.org/2025/11/08/cleveland-clinic-first-in-human-trial-of-crispr-gene-editing-therapy-shown-to-safely-lower-cholesterol-and-triglycerides]
- 98. Next-Generation Sequencing in CRISPR Gene Editing ... [https://www.cd-genomics.com/resource-next-generation-sequencing-in-crispr.html]
- 99. CRISPR off-target detection with NGS | IDT [https://www.idtdna.com/pages/technology/crispr/crispr-genome-editing/crispr-detection/next-generation-sequencing]
- 100. How to Pick the Best CRISPR Data Analysis Method for ... [https://www.synthego.com/guide/how-to-use-crispr/analysis-methods/]
- 101. Bioinformatics approaches to analyzing CRISPR screen data [https://pmc.ncbi.nlm.nih.gov/articles/PMC10019185/]
- 102. CRISPR screening redefines therapeutic target ... [https://www.sciencedirect.com/science/article/pii/S2095177925001741]
- 103. Research Highlights: CRISPR [https://www.broadinstitute.org/research-highlights-crispr]
- 104. Sanger sequencing — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/sanger-sequencing/]
- 105. Mastering DNA chromatogram analysis in Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10643650/]
- 106. TIDE [https://tide.nki.nl/]
- 107. How To Use ICE: A Detailed Guide for Analyzing CRISPR ... [https://www.synthego.com/guide/how-to-use-crispr/ice-analysis-guide/]
- 108. Systematic Comparison of Computational Tools for Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10854981/]
- 109. Analyzing Sanger Sequencing Data [https://blog.genewiz.com/analyzing-sanger-sequencing-data]
- 110. Past, present, and future of CRISPR genome editing ... [https://www.sciencedirect.com/science/article/pii/S0092867424001119]
- 111. Comparative Analysis of Methods for Assessing On-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11932317/]
- 112. CRISPR Gene Editing Workflow: A Step-by-Step Guide [https://www.cd-genomics.com/blog/crispr-gene-editing-workflow-a-step-by-step-guide/]
- 113. A Survey of Validation Strategies for CRISPR-Cas9 Editing [https://www.nature.com/articles/s41598-018-19441-8]
- 114. Validating CRISPR/Cas9-mediated Gene Editing [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/advanced-gene-editing/validating-crispr-cas9-mediated-gene-editing?srsltid=AfmBOop4TMHCoget6v4MxpEV-OaLSTtIwAoNrYoL5lb_GjC8khTvRVc8]
- 115. Genome Editing Validation using T7 Endonuclease I [https://www.goldbio.com/blogs/articles/genome-editing-validation-using-t7-endonuclease?srsltid=AfmBOooQ5s8-yA19cyfAsay7QHgJYcTt6iUa-hQtJ6PGvnDH5QlwFltP]
- 116. Optimization of gene knockout approaches and sgRNA ... [https://www.nature.com/articles/s41598-025-24184-4]
- 117. High Throughput Analysis of CRISPR-Cas9 Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10427880/]
- 118. CRISPR-finder: A high throughput and cost-effective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10095899/]
- 119. Precise measurement of CRISPR genome editing ... [https://www.sciencedirect.com/science/article/pii/S2329050125000440]
- 120. A benchmark of algorithms for the analysis of pooled CRISPR ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-020-01972-x]
- 121. Global CRISPR Gene Editing Market Size, Share 2025 [https://www.custommarketinsights.com/report/crispr-gene-editing-market/]
- 122. How to use CRISPR for functional validation in cell biology? [https://synapse.patsnap.com/article/how-to-use-crispr-for-functional-validation-in-cell-biology]
- 123. Precisely defining disease variant effects in CRISPR-edited ... [https://www.nature.com/articles/s41586-025-09313-3]
- 124. Functional interrogation of non-coding DNA through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5483188/]
- 125. TALEN and CRISPR Validation Tools [https://www.thermofisher.com/us/en/home/life-science/genome-editing/crispr-validation.html]
- 126. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 127. Modeling disease in vivo with CRISPR/Cas9 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4592741/]